Emergency treatment of stroke involves several steps:
1. Rapid diagnosis through imaging such as CT or MRI to determine if the stroke is ischemic or hemorrhagic.
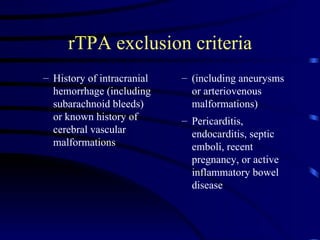
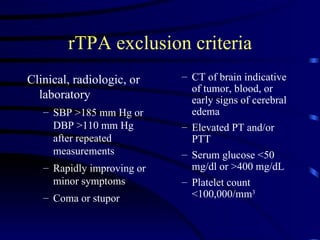
2. For ischemic strokes within 3 hours, treatment with rTPA (recombinant tissue plasminogen activator) can dissolve clots and reduce long-term disability if eligibility criteria are met.
3. Intensive monitoring is required after rTPA to control blood pressure and watch for bleeding complications.
4. Surgery may be considered for large hemorrhagic strokes or subarachnoid hemorrhage from aneurysms to relieve pressure on the brain.