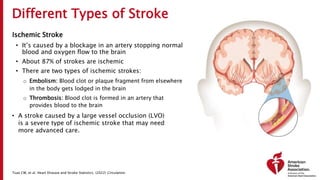
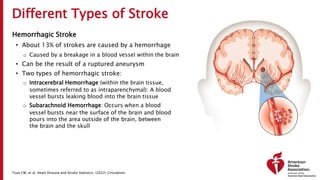
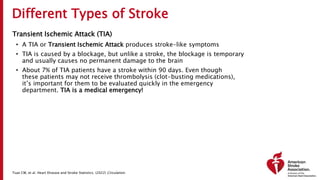
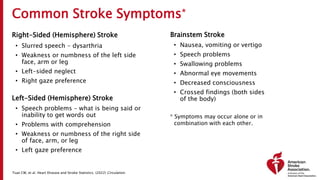
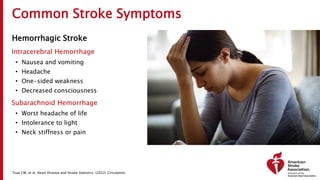
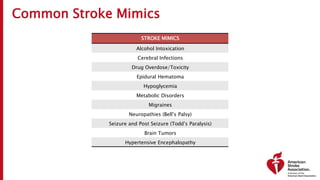
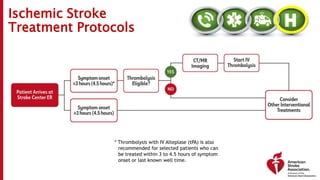
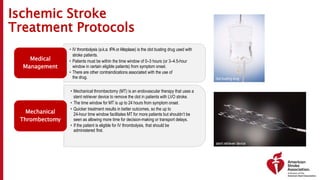
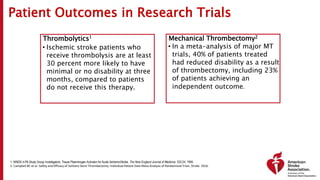
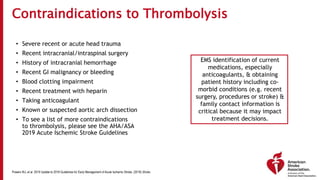
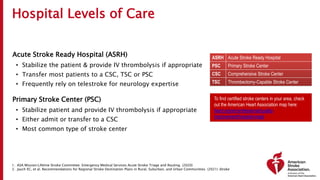
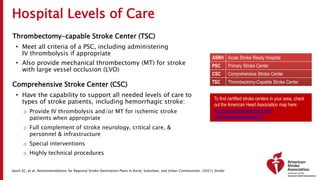
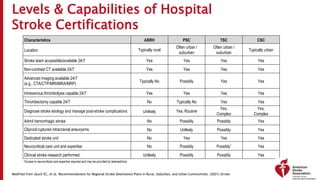
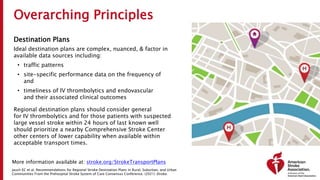
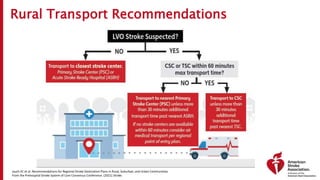
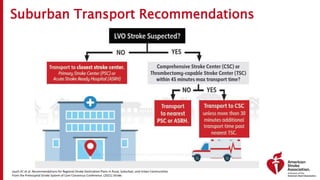
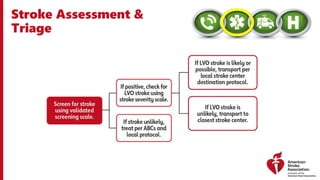
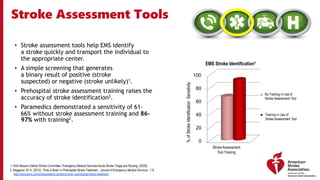
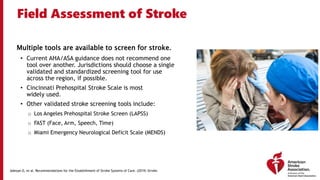
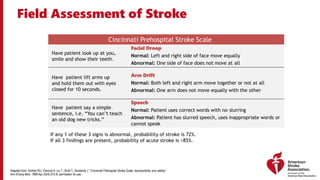
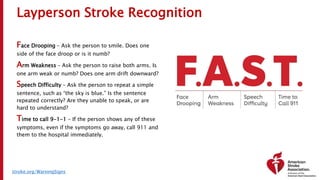
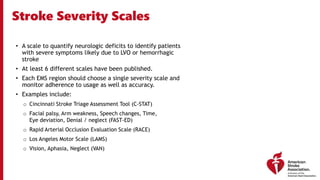
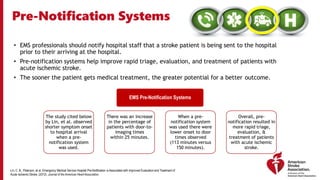
The document outlines a training course for EMS professionals focused on stroke recognition, treatment, and care protocols. It emphasizes the critical role of EMS in ensuring timely access to stroke therapies and details various stroke types, symptoms, treatment protocols, and hospital care levels. Key recommendations include early assessment, use of standardized screening tools, and swift hospital notification to maximize patient outcomes.