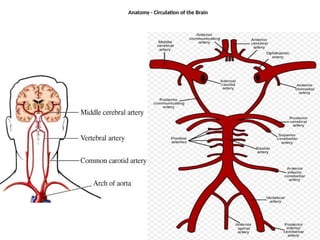
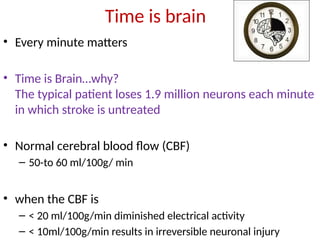
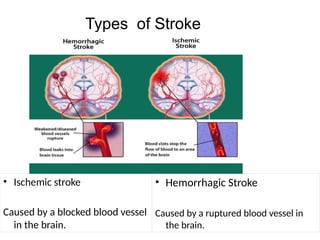
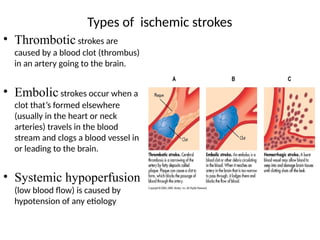
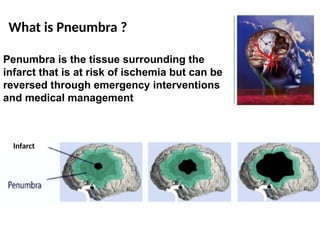
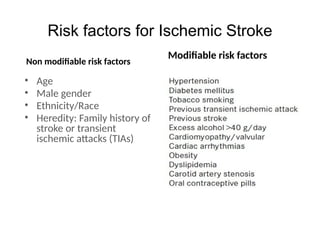
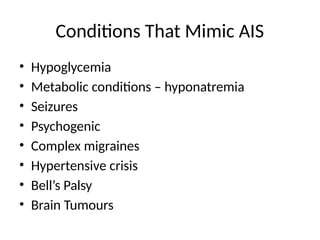
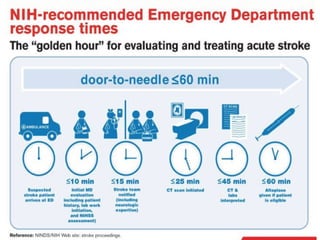
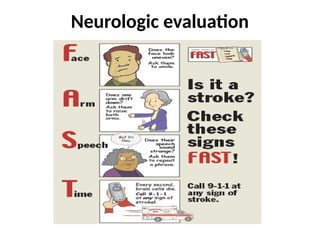
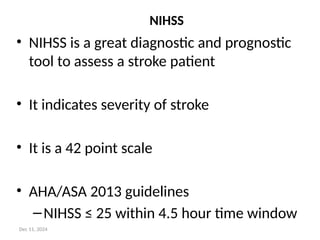
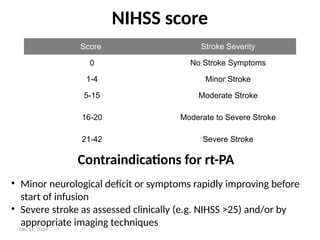
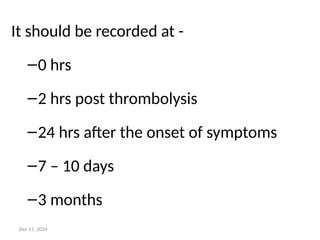
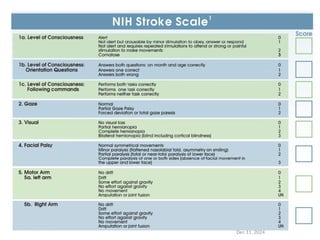
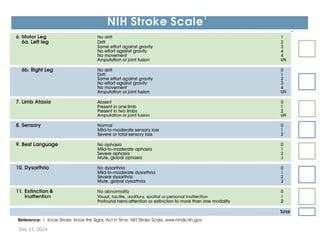
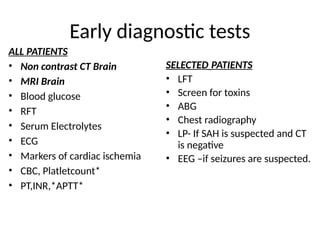
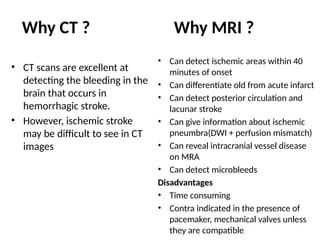
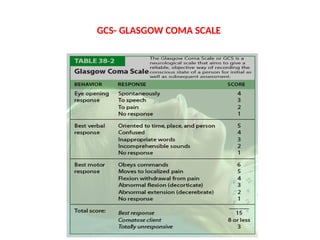
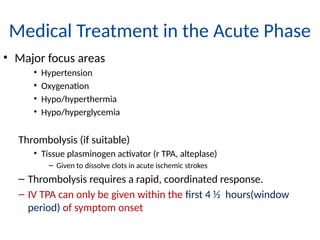
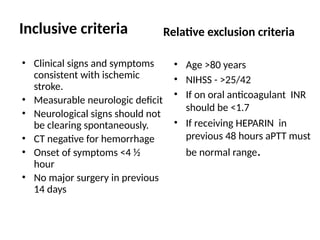
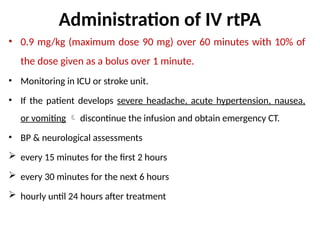
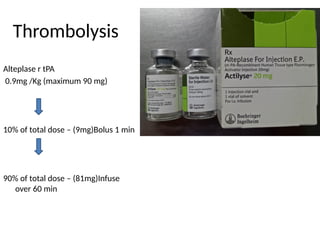
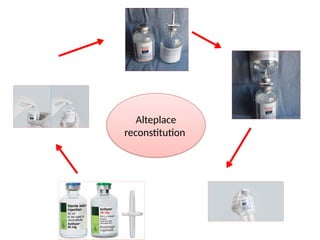
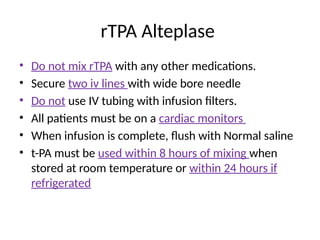
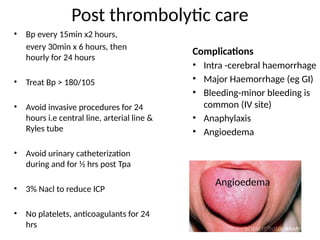
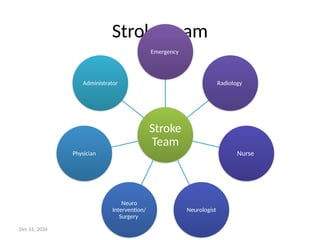
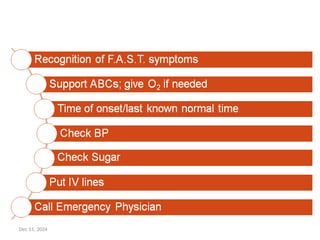
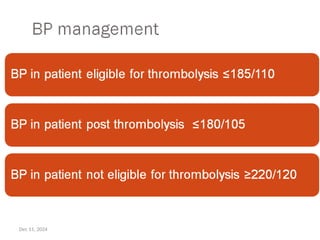
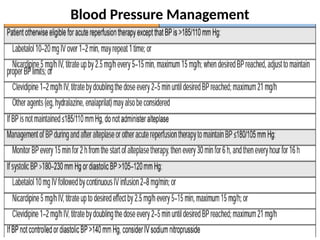
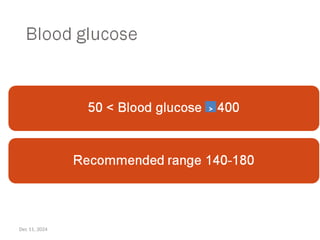
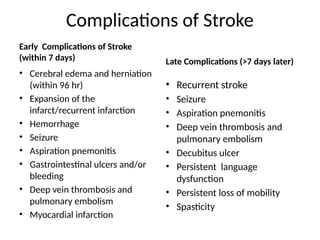
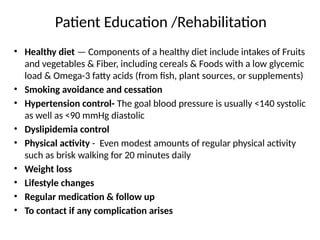
The document provides an overview of acute ischemic stroke, defining it as a clinical syndrome with focal neurological deficits lasting over 24 hours. It discusses various types of stroke, risk factors, diagnostic procedures, and treatment approaches, including thrombolysis with tissue plasminogen activator. The text emphasizes the importance of timely intervention, the role of the National Institutes of Health Stroke Scale (NIHSS), and post-stroke management and rehabilitation strategies.