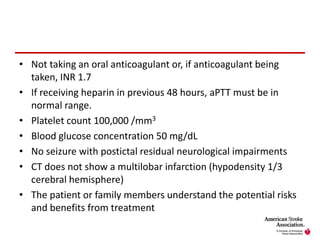
The document outlines the guidelines for the early management of adults with ischemic stroke, emphasizing critical components such as the administration of intravenous rtPA, blood pressure management, and urgent diagnostic protocols. It addresses specific criteria for treatment eligibility and monitoring procedures, along with recommendations for managing blood glucose levels and other acute care considerations. It highlights the importance of timely intervention and coordination among emergency medical services and hospital staff to improve patient outcomes.