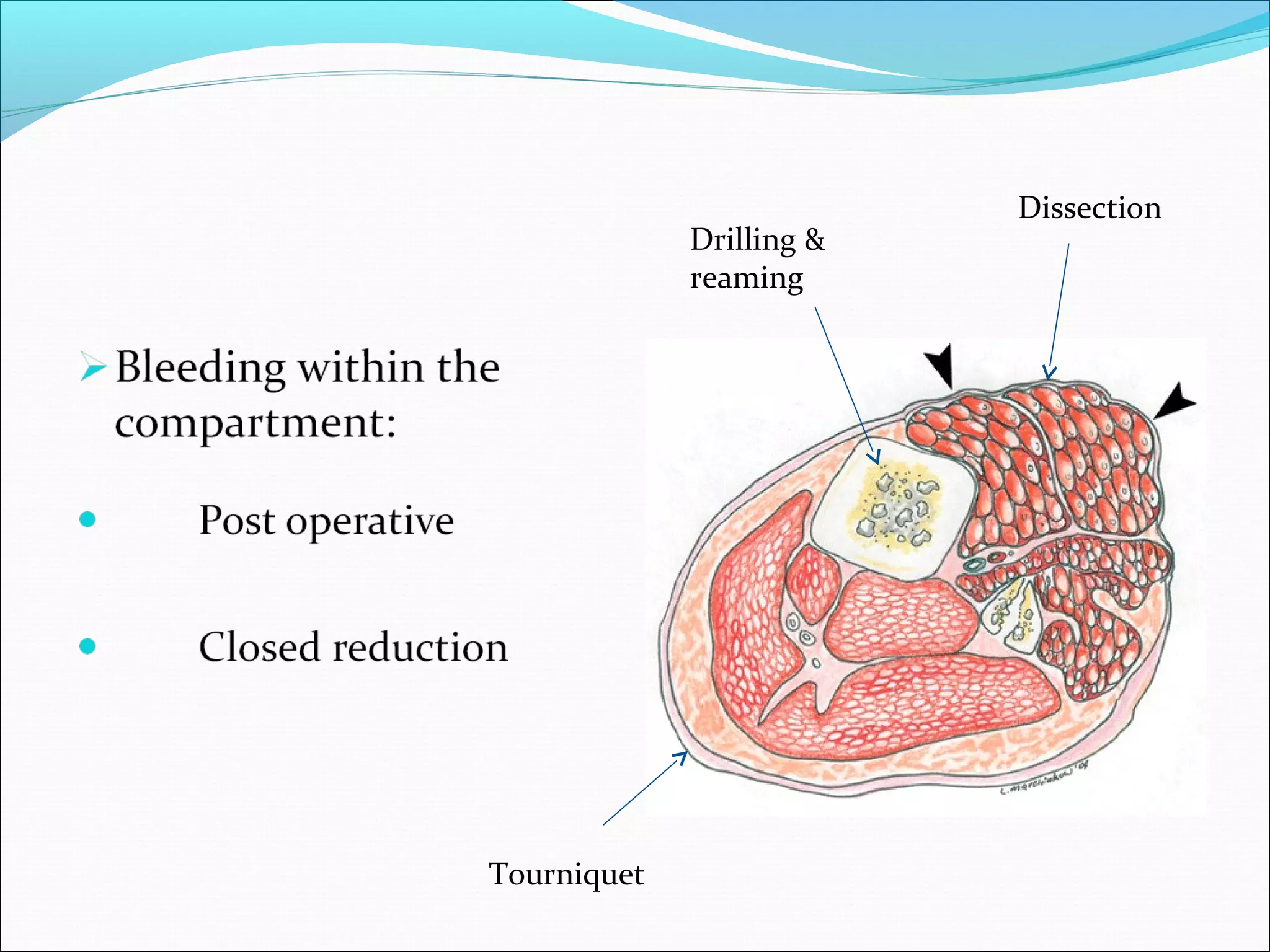
Compartment syndrome occurs when increased pressure within a closed muscle compartment reduces blood flow, potentially causing tissue death. It is caused by factors that increase swelling such as fractures. Symptoms include pain disproportionate to the injury that worsens with stretching of muscles. Diagnosis involves measuring compartment pressure. Early fasciotomy, in which fascia is cut to release pressure, can prevent complications if performed within 6-8 hours of onset. Later surgery risks muscle death and contractures.