1. The Advanced Trauma Life Support (ATLS) protocol focuses on simultaneously identifying and treating life-threatening injuries within the crucial "Golden Hour" period after trauma.
2. The ATLS protocol involves two surveys - the Primary Survey to address airway, breathing, circulation, disability, and exposure issues, and the Secondary Survey for a full history and physical exam after initial resuscitation is complete.
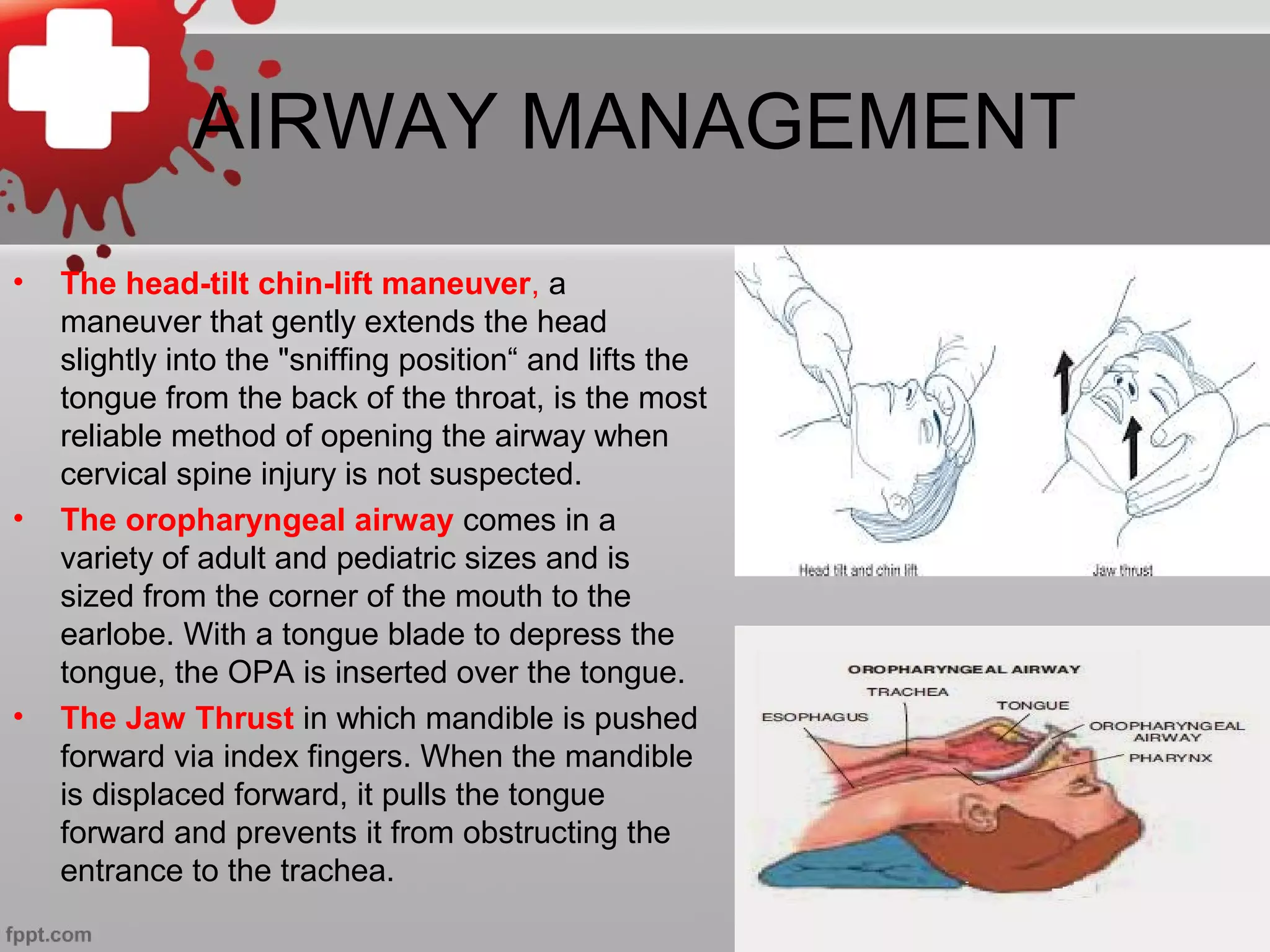
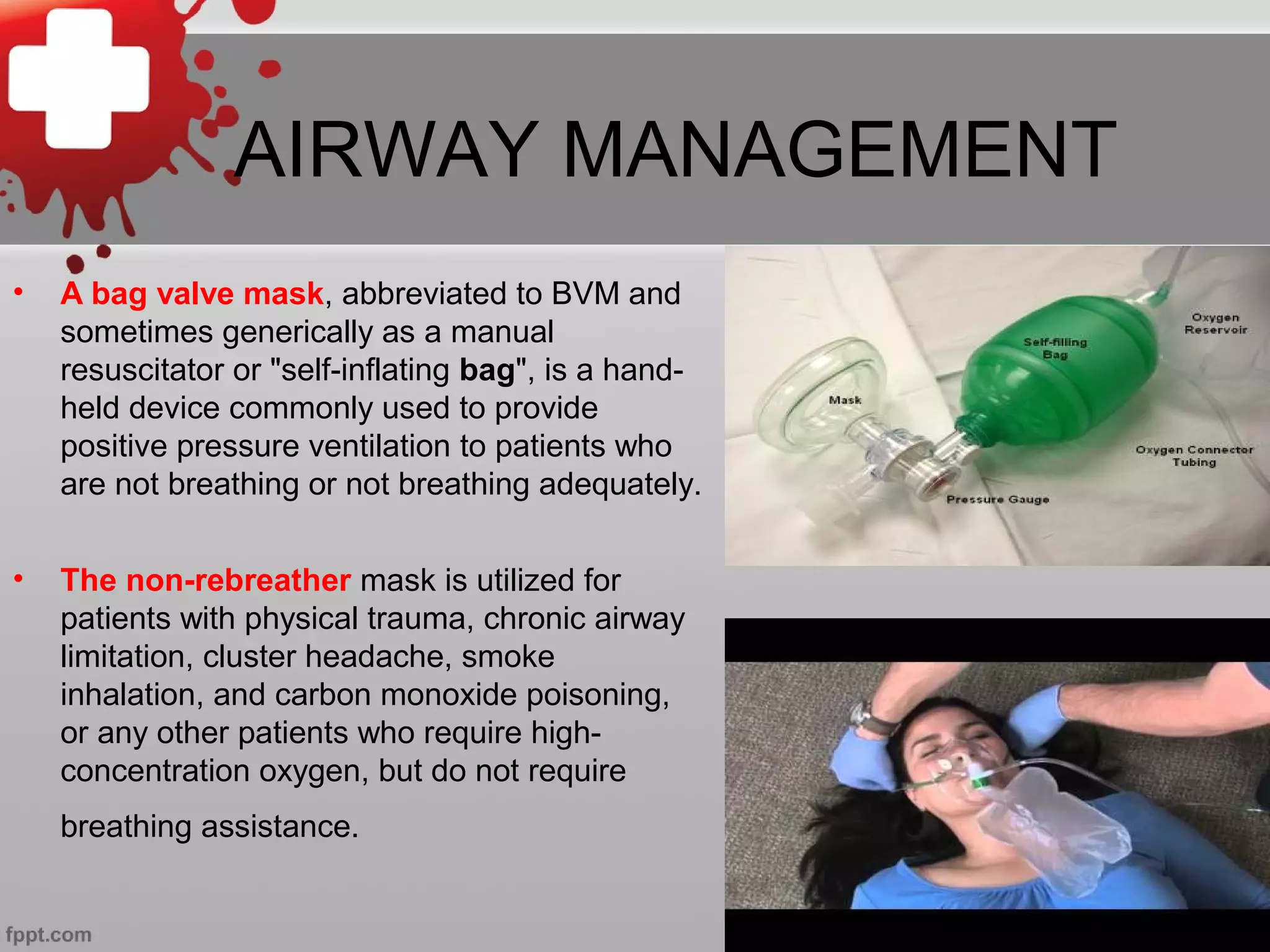
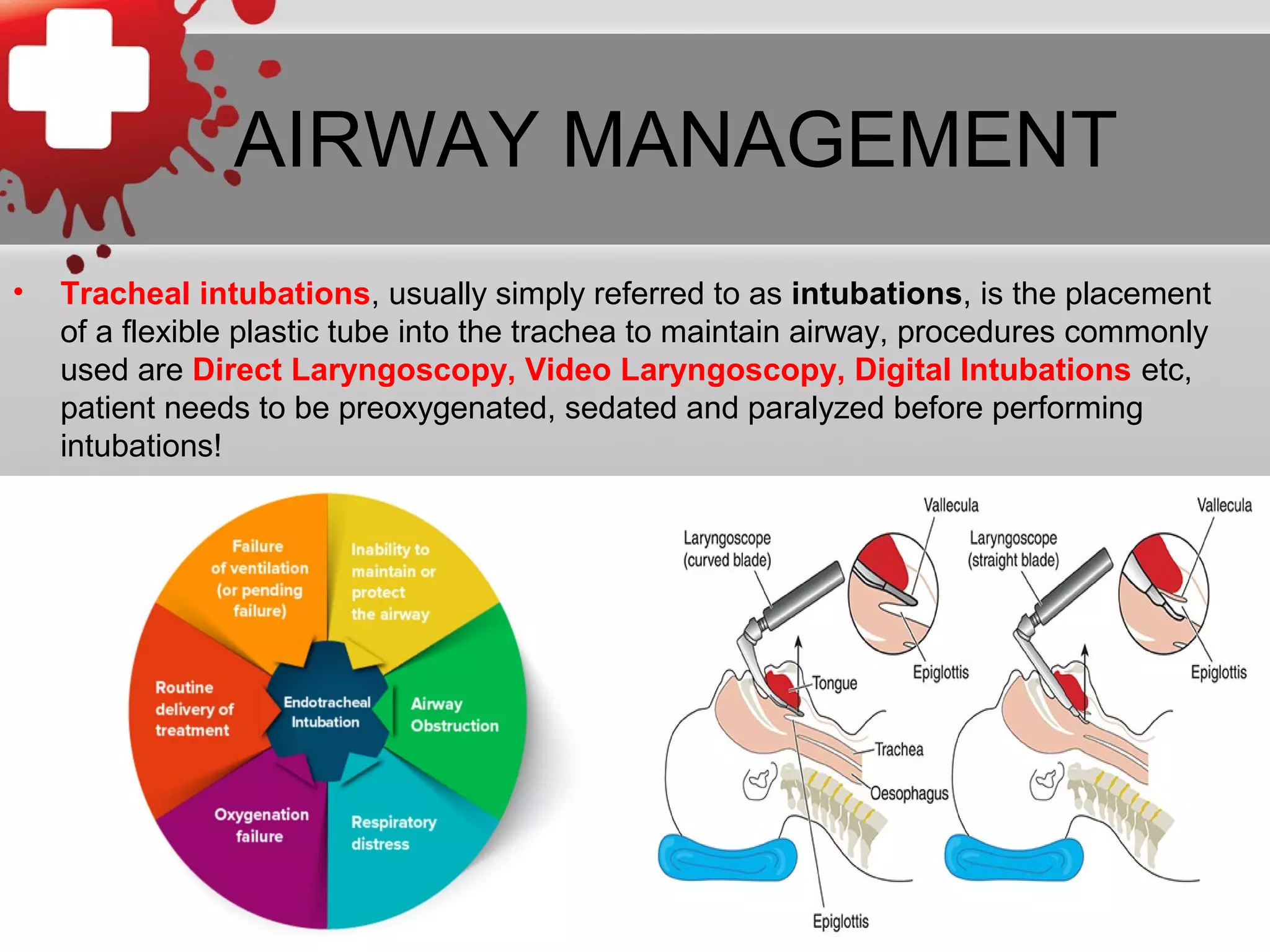
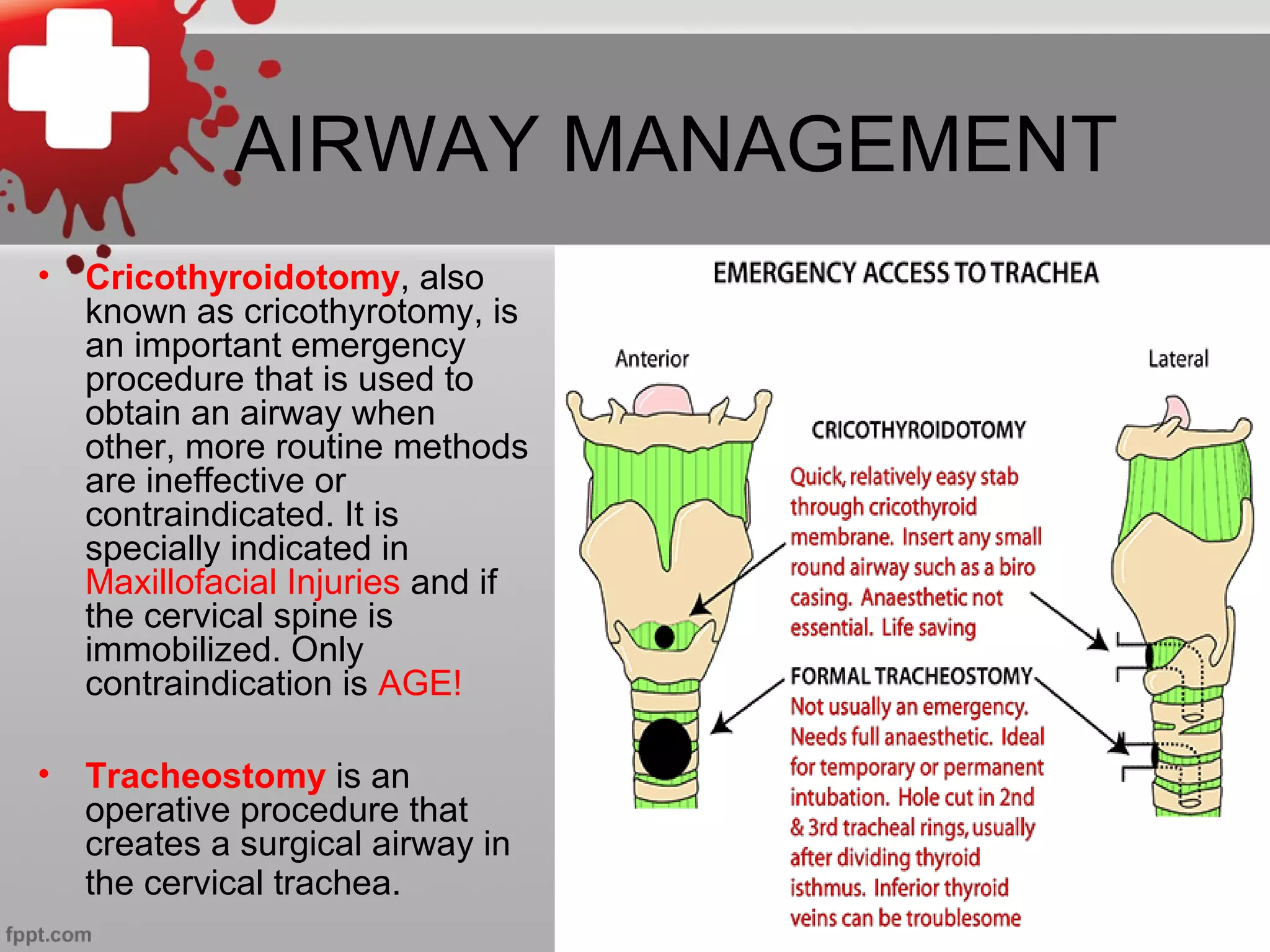
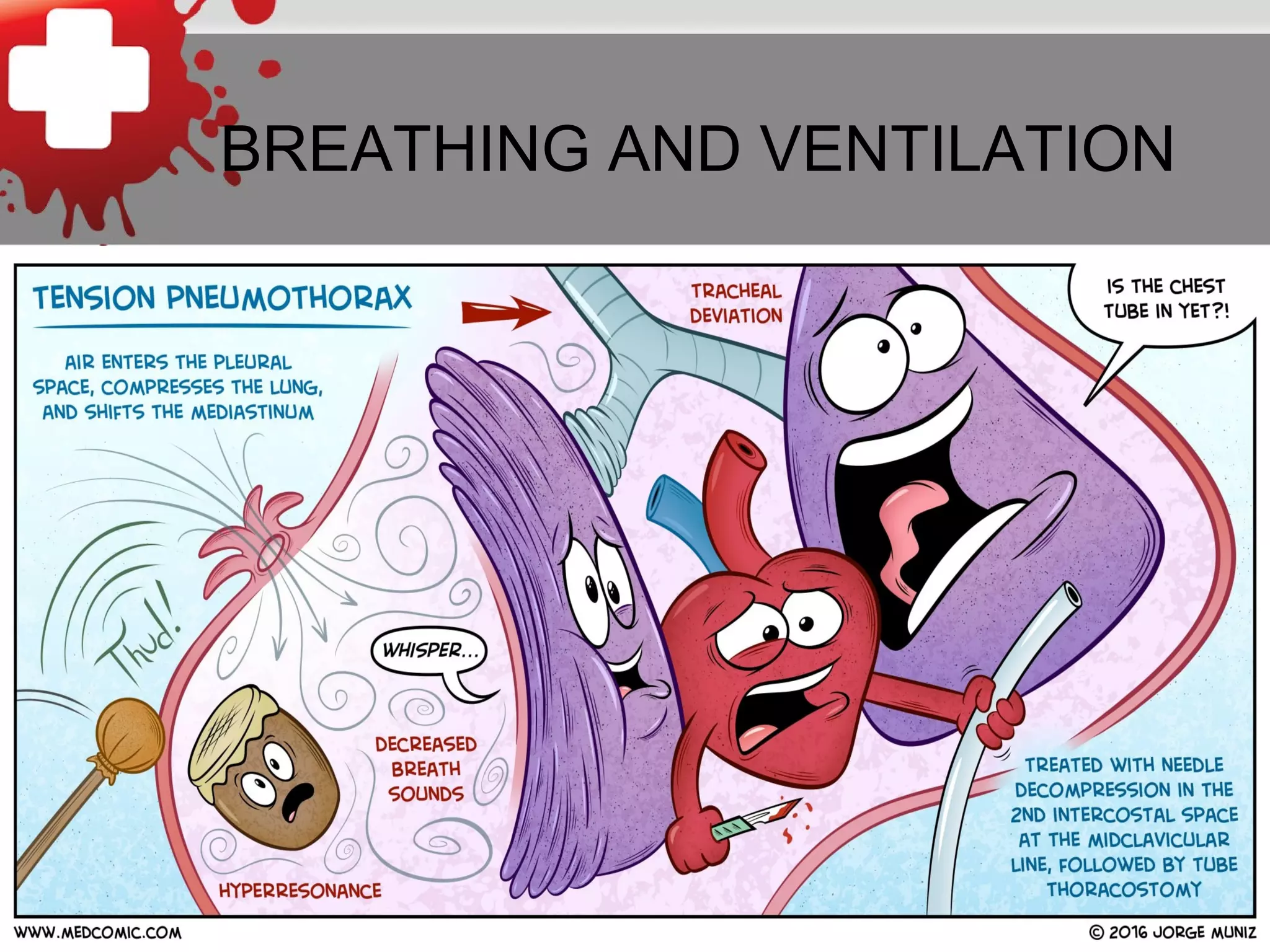
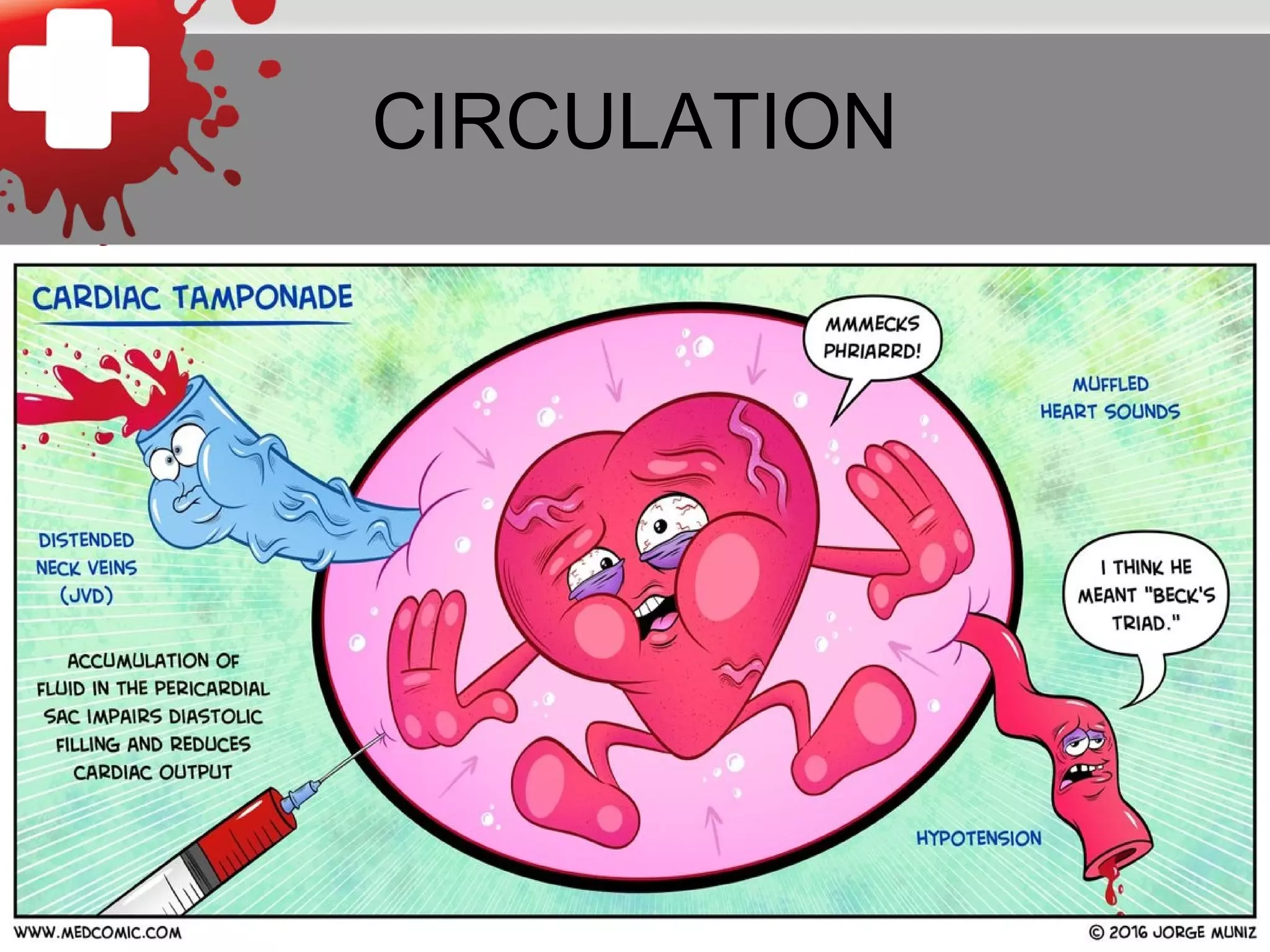
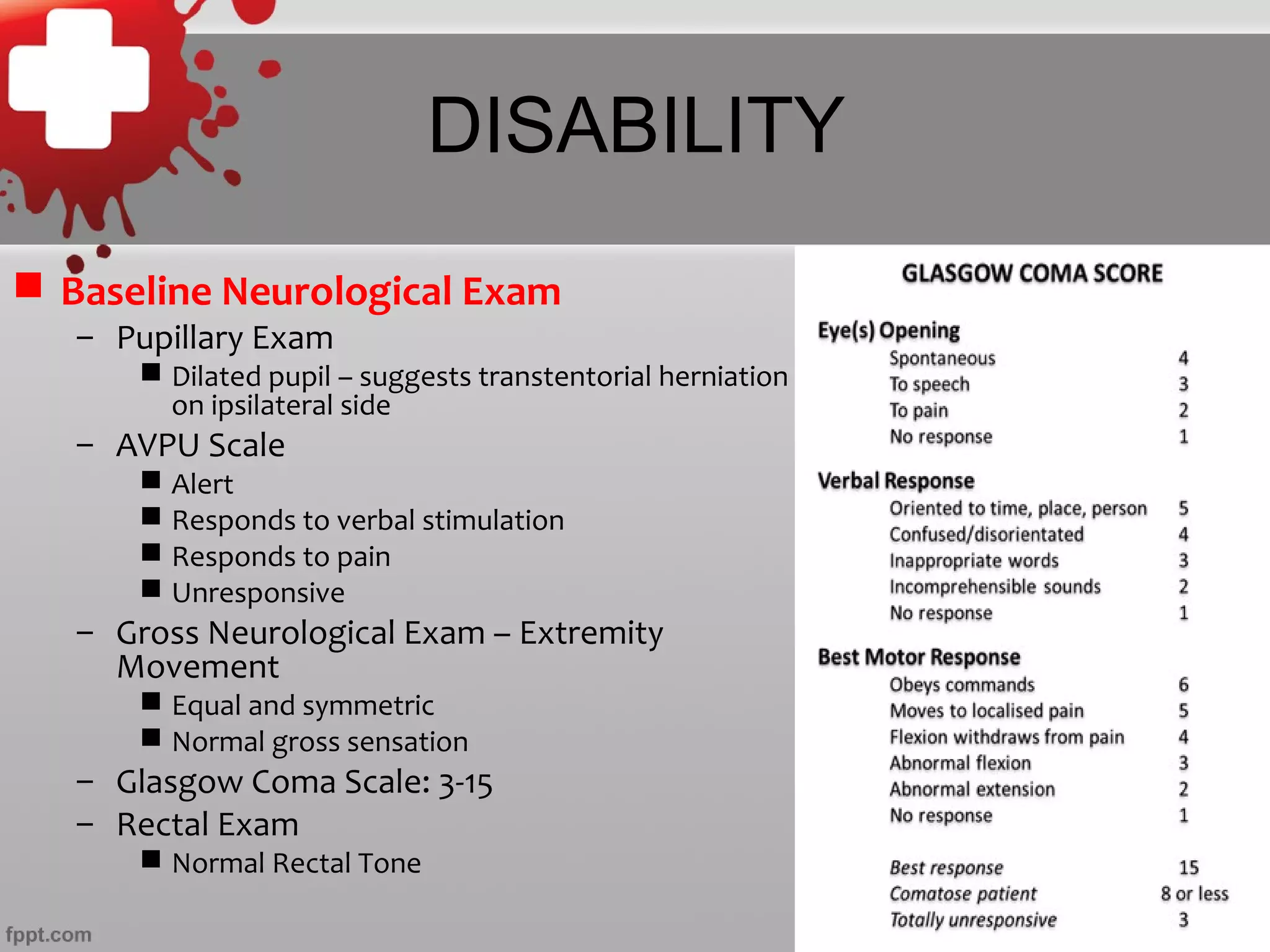
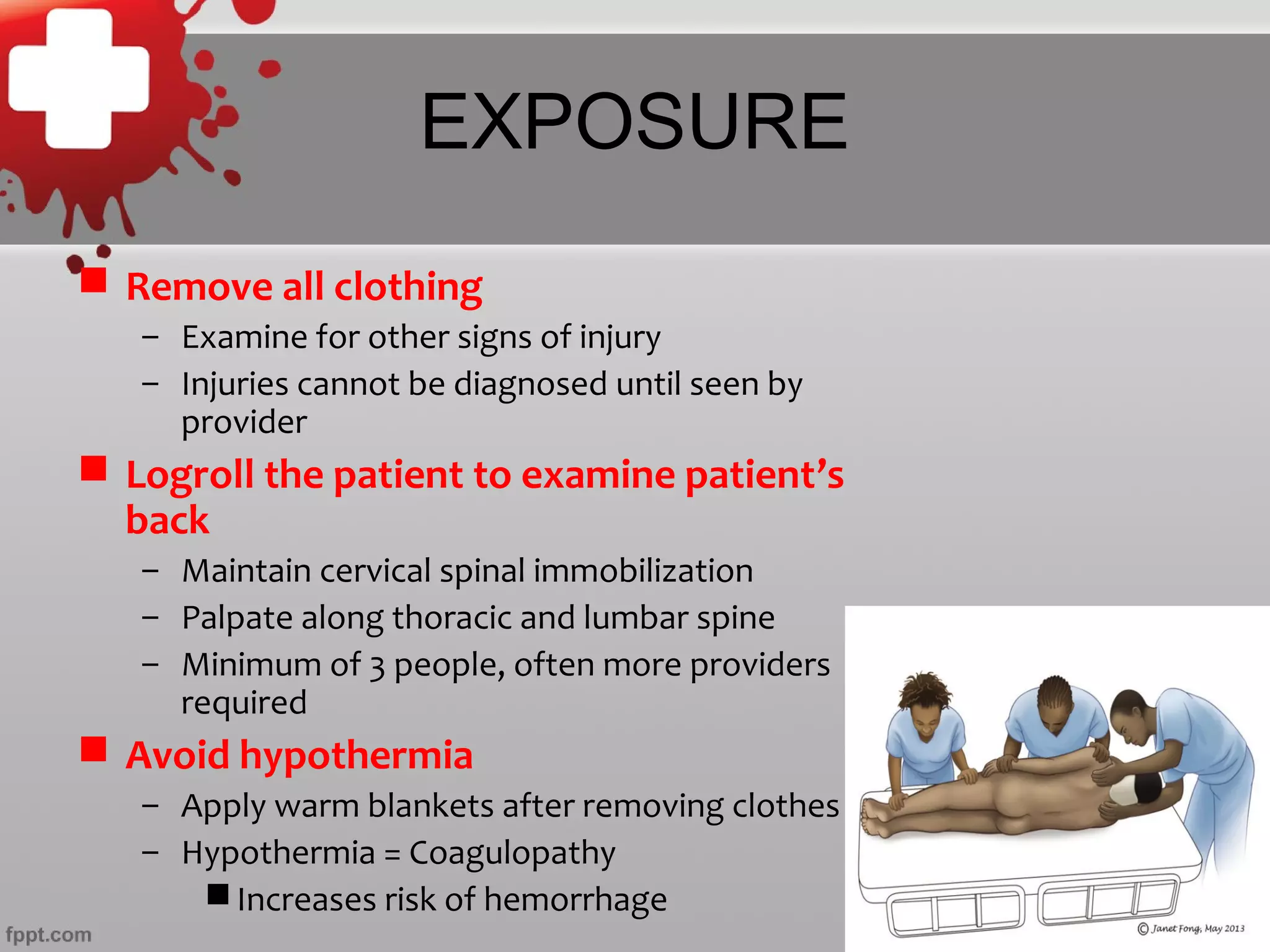
3. Key components of the Primary Survey include assessing the airway, identifying tension pneumothorax and hemorrhage, and providing spinal immobilization, followed by full exposure to identify all injuries.