The document provides an overview of the Advanced Trauma Life Support (ATLS) program. It describes how ATLS was developed in the 1970s by Dr. James Styner after a plane crash left him realizing the need for standardized trauma care. The summary describes the goals of ATLS to provide a systematic approach to trauma resuscitation and management. It also summarizes the primary and secondary survey process in ATLS which focuses on rapid assessment and stabilization of airway, breathing, circulation, disability and exposure followed by a full head-to-toe examination.


![ External hemorrhage is identified and controlled during the primary survey.
Direct manual pressure
Tourniquet: carry a risk of ischemic injury
Do NOT do Blind clamping.
Internal hemorrhage; Four More
Physical examination and imaging;
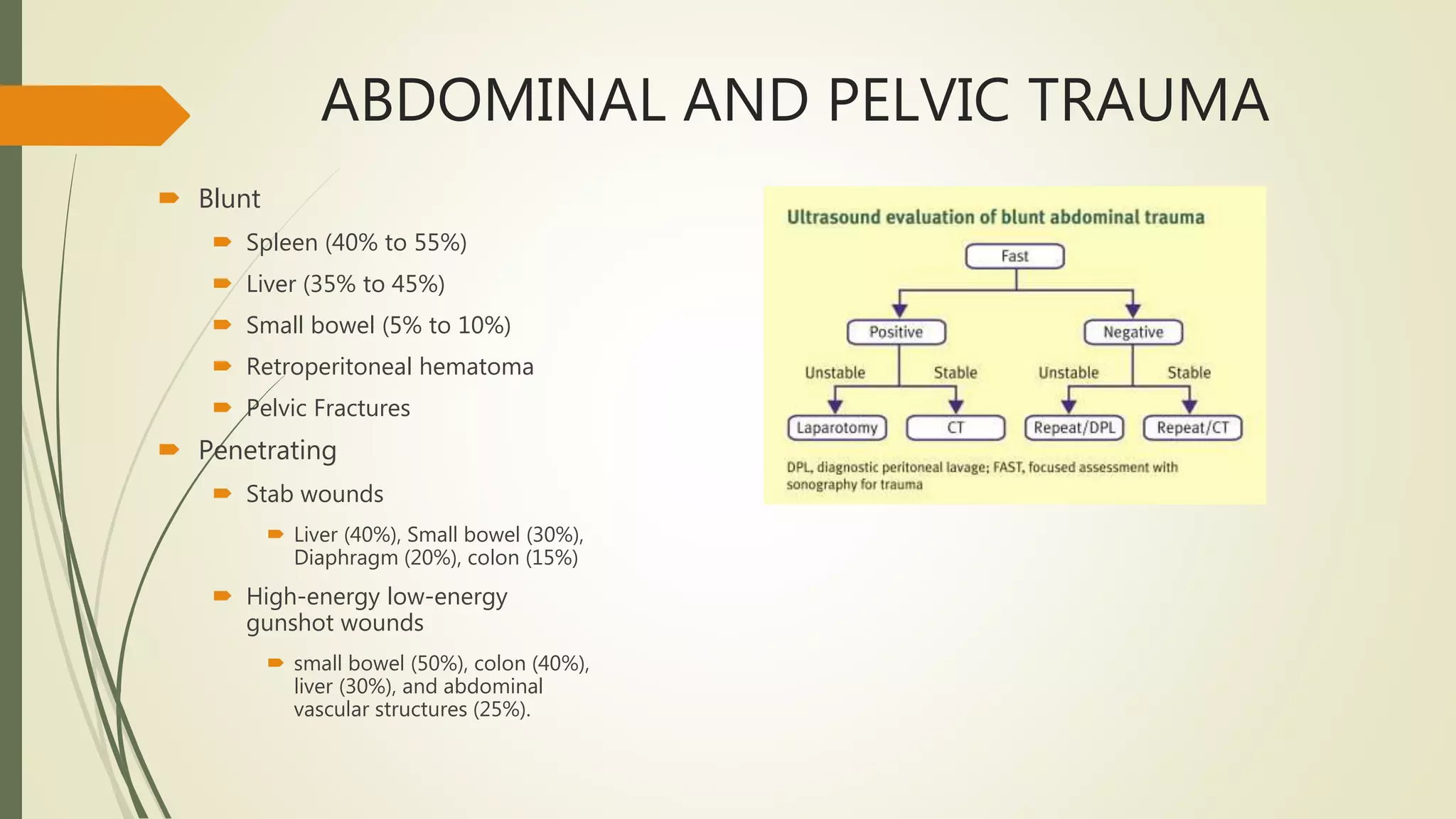
Chest x-ray, Pelvic x-ray, focused assessment with sonography for trauma [FAST], or diagnostic
peritoneal lavage [DPL].
Chest decompression, and application of a pelvic stabilizing device and/ or extremity splints.
Definitive management may require surgical or interventional radiologic treatment and pelvic and
long-bone stabilization.
Definitive bleeding control is essential, along with appropriate replacement of intravascular](https://image.slidesharecdn.com/atls00-220316200224/75/Atls-Advanced-Trauma-Life-Support-12-2048.jpg)