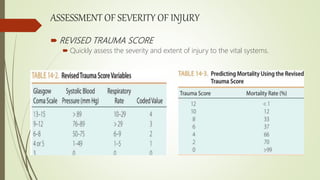
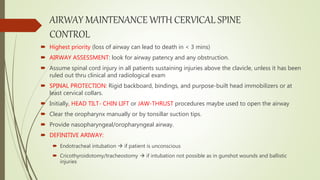
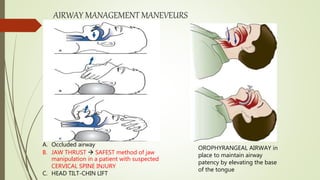
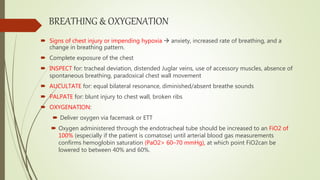
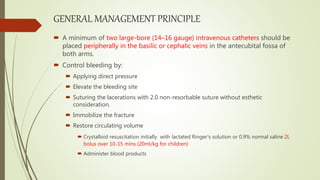
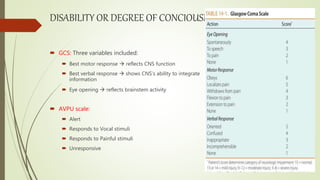
This document outlines the principles of Advanced Trauma Life Support (ATLS) for treating trauma patients. It describes the primary and secondary surveys which involve assessing and stabilizing the ABCDEs (airway, breathing, circulation, disability, exposure). The primary survey focuses on life-threatening injuries through rapid evaluation of airway/breathing, circulation, disability, and exposure. The secondary survey involves a full physical exam and history to identify all injuries and guide further care. The goal of ATLS is to prevent avoidable deaths through systematic initial management within the critical golden hour after trauma.