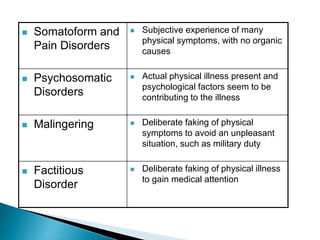
This document discusses somatization disorder, including its definition, symptoms, diagnosis, treatment, and prognosis. Somatization disorder involves a person experiencing physical symptoms that cannot be explained medically, and it affects their daily functioning. Treatment involves developing a trusting doctor-patient relationship, avoiding unnecessary medical tests, and utilizing psychotherapy and lifestyle changes like exercise to help manage stress and underlying mental health conditions. The prognosis is generally improved with a multidisciplinary treatment approach.