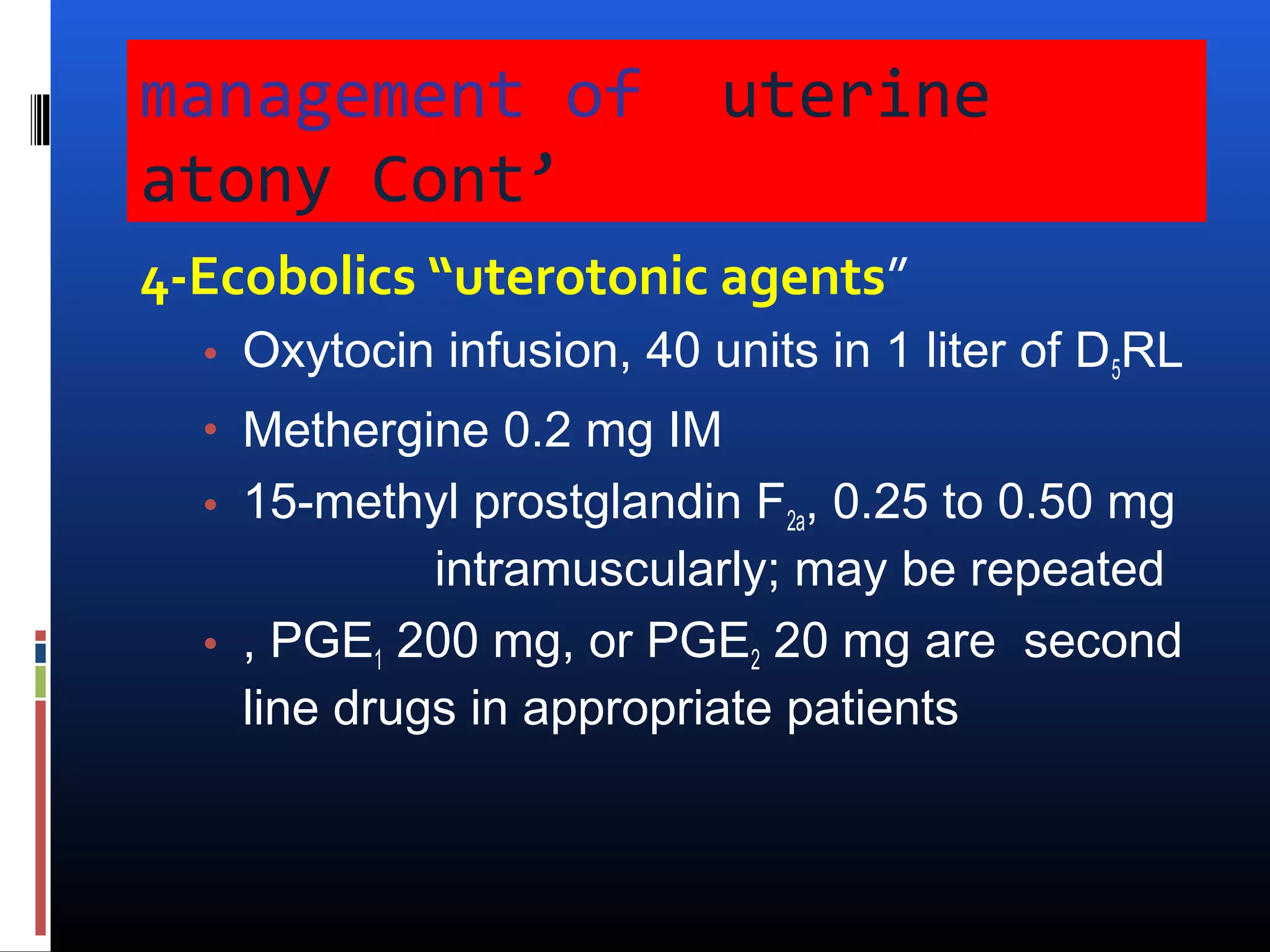
Postpartum hemorrhage (PPH) is defined as blood loss exceeding 500 ml after vaginal delivery and 1000 ml after cesarean, significantly contributing to maternal mortality. Key causes include uterine atony, trauma, tissue retention, and coagulation defects, with effective management emphasizing accurate blood loss measurement and timely interventions. Prevention strategies include administering oxytocin and appropriate uterine massage, with worsening cases requiring surgical options if medical management fails.