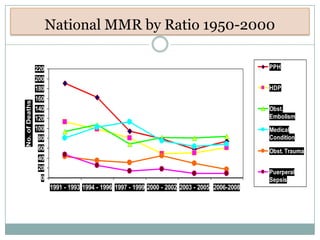
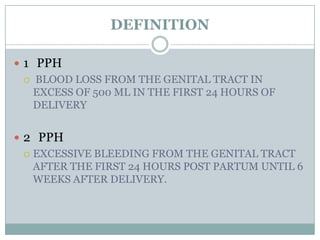
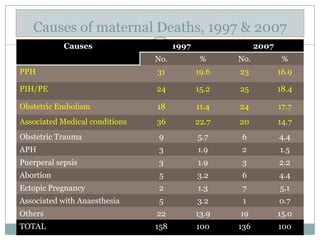
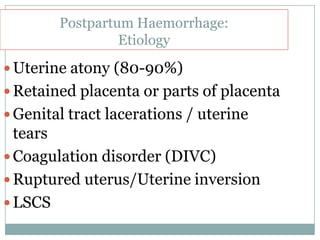
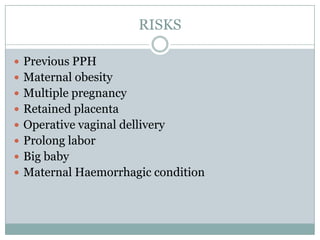
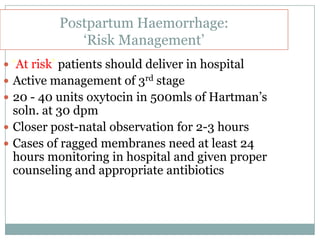
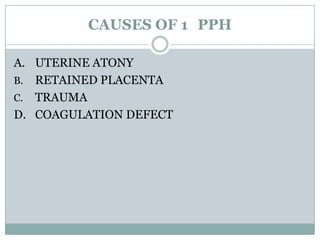
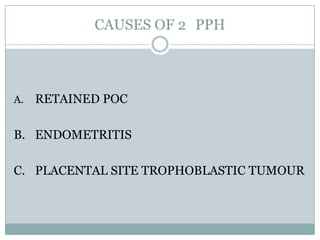
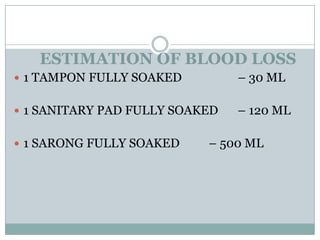
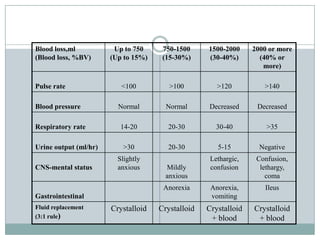
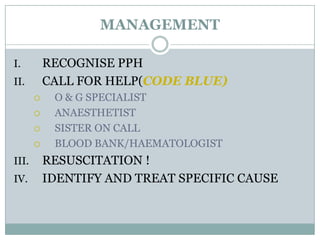
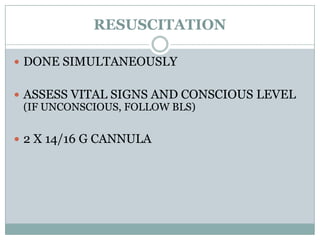
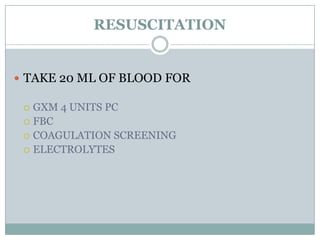
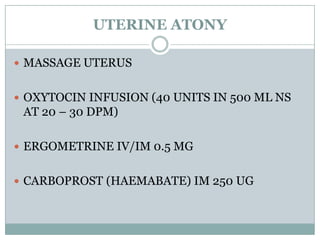
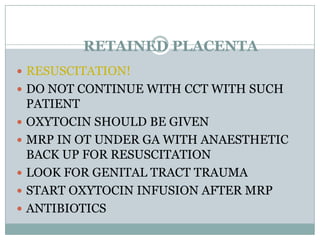
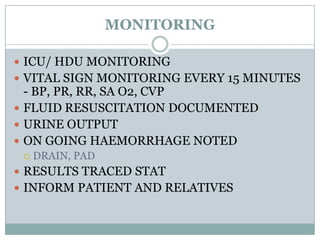
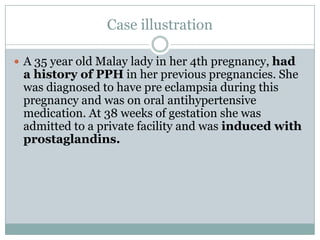
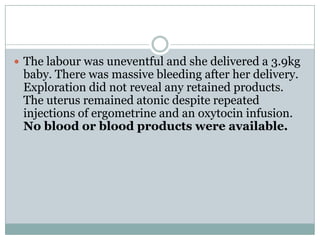
Postpartum haemorrhage (PPH) is still a major cause of maternal mortality, responsible for 20-25% of deaths. It can be caused by uterine atony, retained placenta, genital tract trauma, or coagulation disorders. Risk factors include previous PPH, obesity, multiple pregnancy, and operative delivery. Proper management of PPH involves early recognition, resuscitation with IV fluids and blood transfusion, identifying and treating the cause, and close monitoring in ICU. Delays in management and transportation significantly increase mortality.