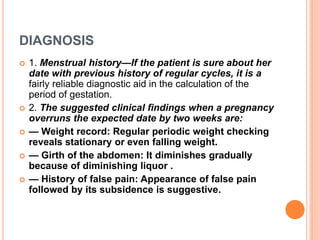
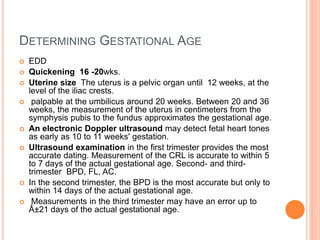
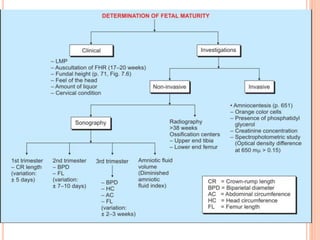
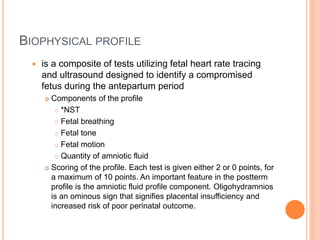
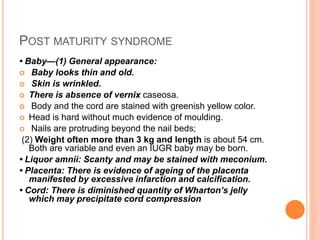
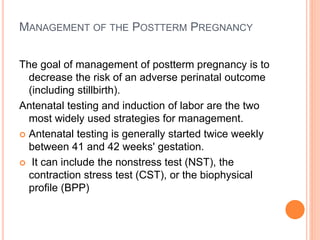
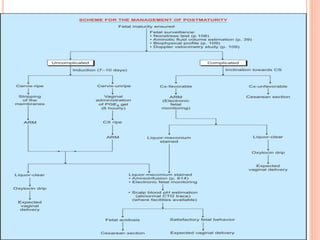
This document discusses postterm pregnancy, defined as any pregnancy exceeding 42 weeks. The incidence is 3-10% and increases with a history of prolonged pregnancy. Dates may be unreliable if last menstrual period is uncertain or contraception was recently used. Causes include incorrect dates, hereditary factors, and maternal or fetal issues. Diagnosis involves menstrual history, weight changes, ultrasound, and biophysical profile testing. Risks to the baby include meconium aspiration, respiratory distress, and hypoglycemia. Management involves antenatal testing starting at 41-42 weeks and potential induction of labor to reduce complications.