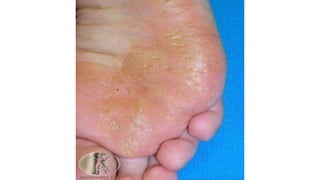
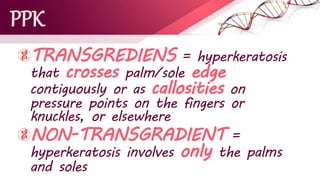
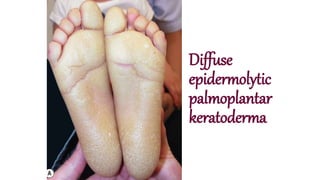
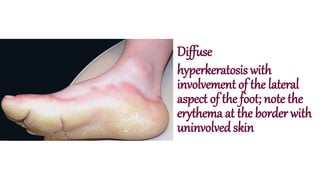
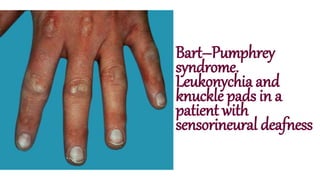
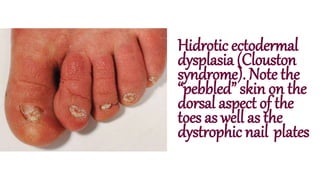
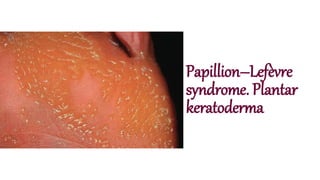
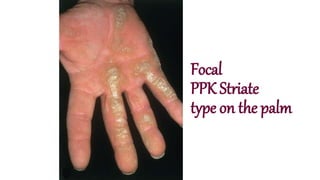
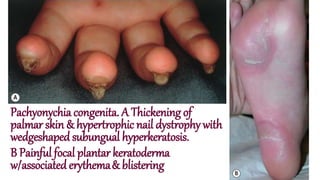
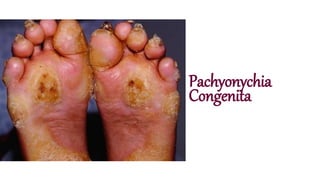
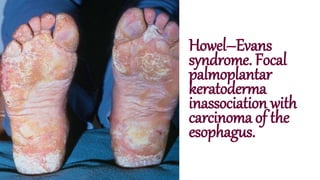
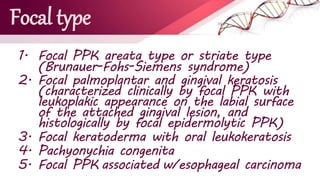
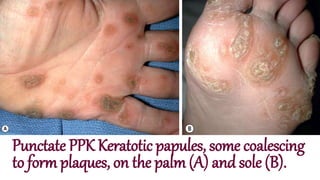
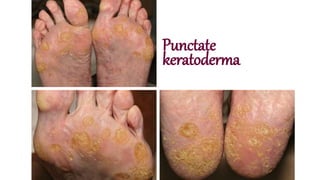
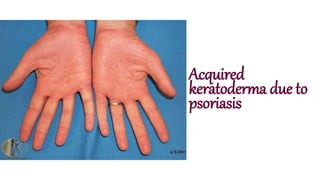
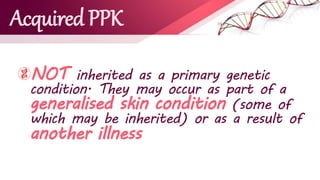
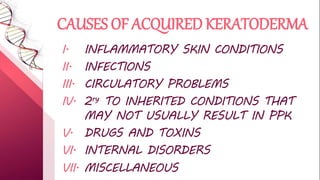
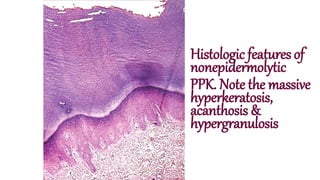
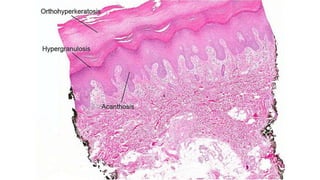
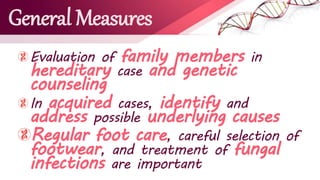
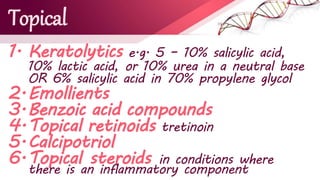
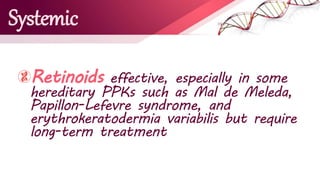
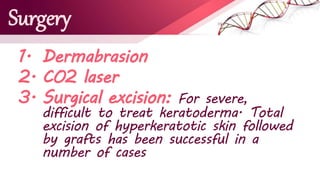
Palmoplantar keratodermas are inherited or acquired skin conditions characterized by chronic hyperkeratosis of palms and soles, requiring comprehensive dermatological examination. They are classified into diffuse, focal, and punctate types, with various hereditary syndromes associated with specific genetic mutations. Treatment options include topical and systemic therapies, but successful management can be challenging and often leads to only short-term relief.