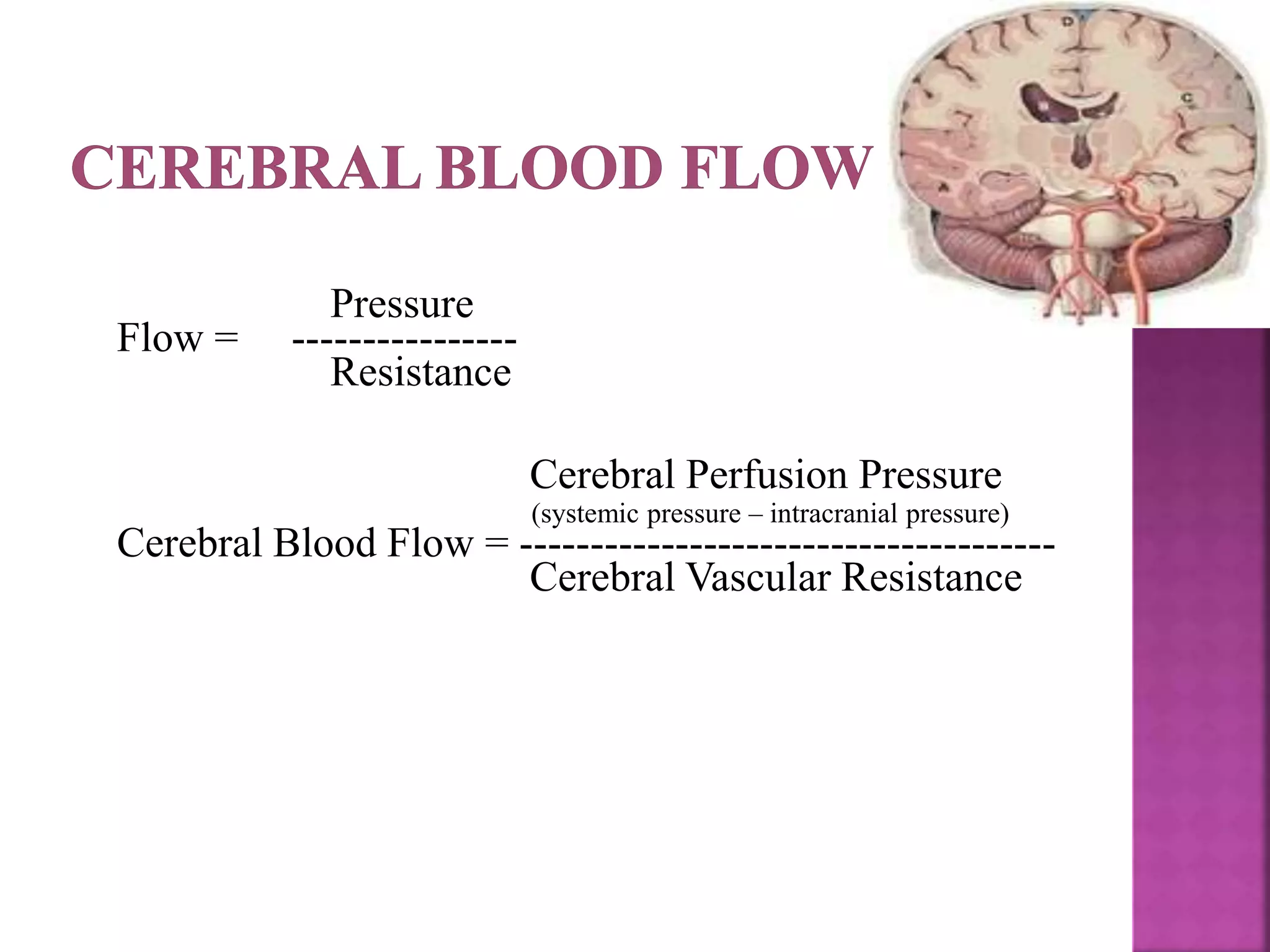
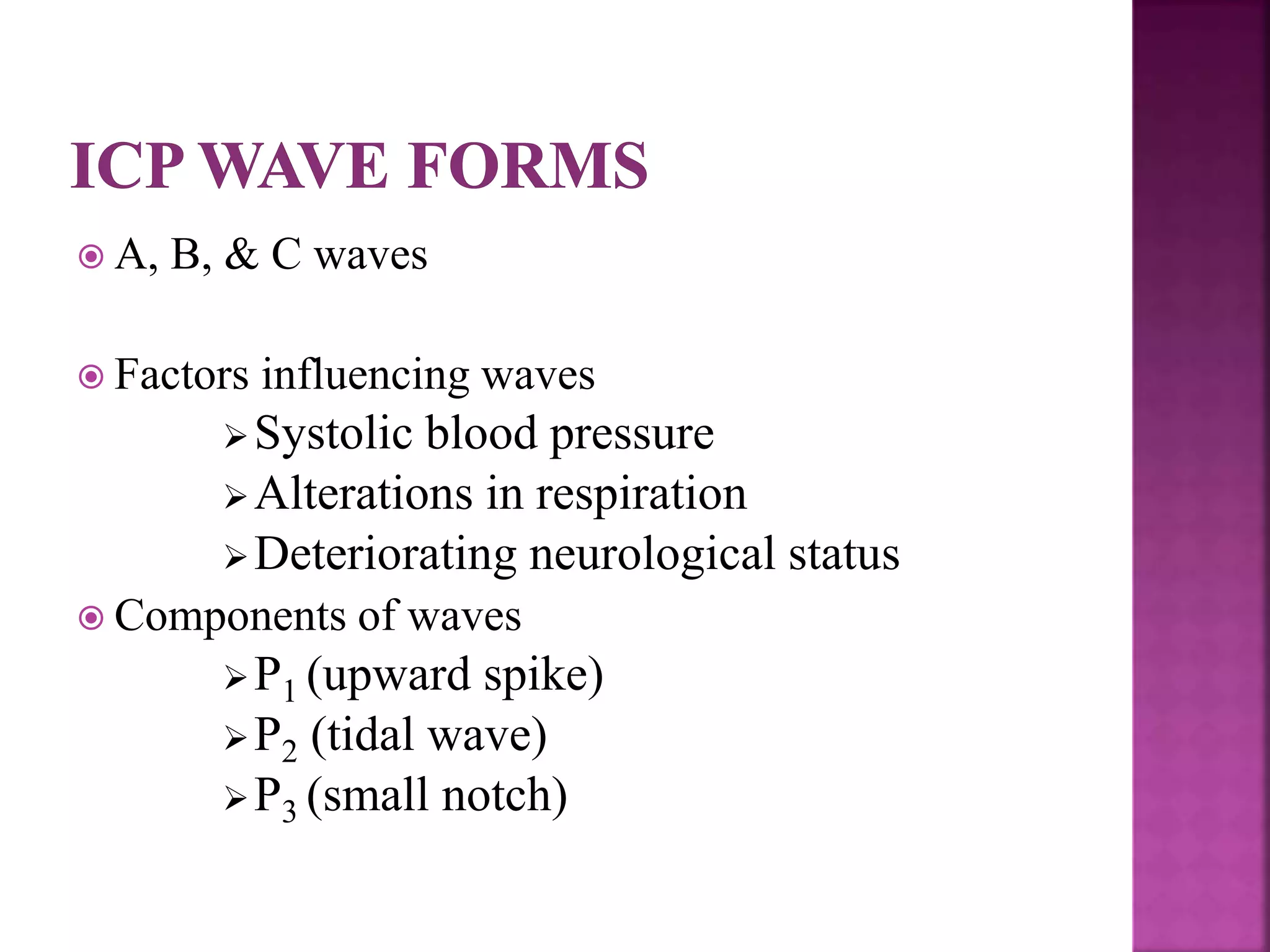
The document discusses intracranial pressure (ICP) monitoring in patients with severe traumatic brain injury. There are invasive and non-invasive methods for measuring ICP. Invasive methods include intraventricular catheters and subarachnoid bolts to directly measure pressure. Non-invasive methods attempt to indirectly measure ICP through techniques like transcranial Doppler ultrasonography and tympanic membrane displacement. Nursing care for patients with increased ICP focuses on airway maintenance, ventilation, fluid balance, positioning, and environmental control to reduce intracranial pressure.