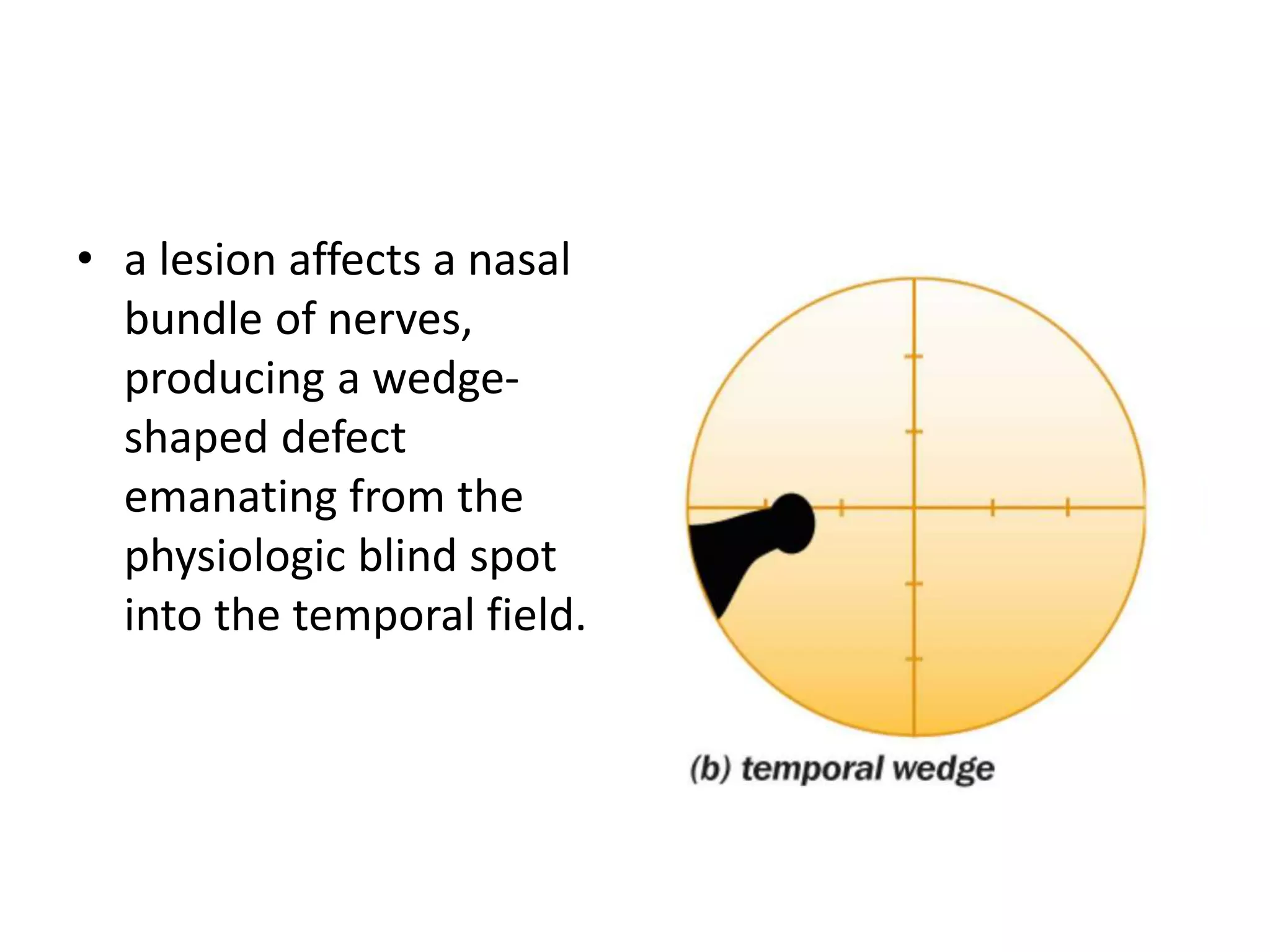
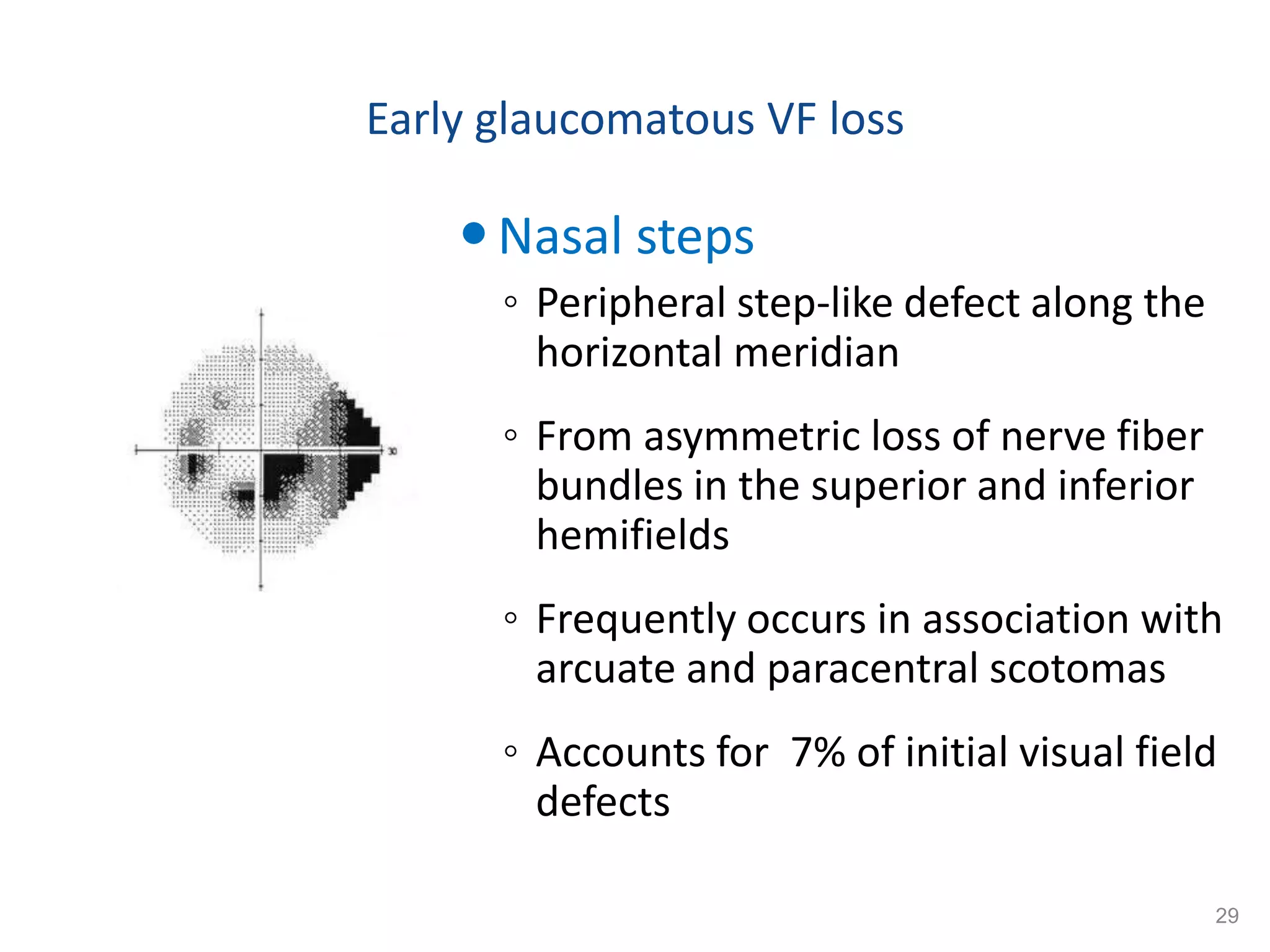
This document provides an overview of visual field assessment in glaucoma patients. It discusses the anatomy and physiology of the visual field, common visual field defects seen in glaucoma including early defects like paracentral scotomas and advanced defects like a central island of vision. It also reviews different perimetry techniques including kinetic perimetry, static perimetry like Goldmann and Humphrey perimetry, and their interpretation. Standard automated perimetry is emphasized as the gold standard for evaluating glaucoma. Characteristics of glaucomatous visual field defects and a severity grading system are also summarized.




















































![Method of Humphrey visual field (HVF)
• The machine automatically calibrates itself on start-up.
Selection of programs includes the following:
full threshold or
Swedish interactive threshold algorithm [SITA] central 30–2,
24–2, 10–2).
Suprathreshold testing (screening central 76 point, full-field
120 point,and Esterman).
Colored stimuli can also be use.](https://image.slidesharecdn.com/visualfield-190319173228/75/Visual-field-59-2048.jpg)

















