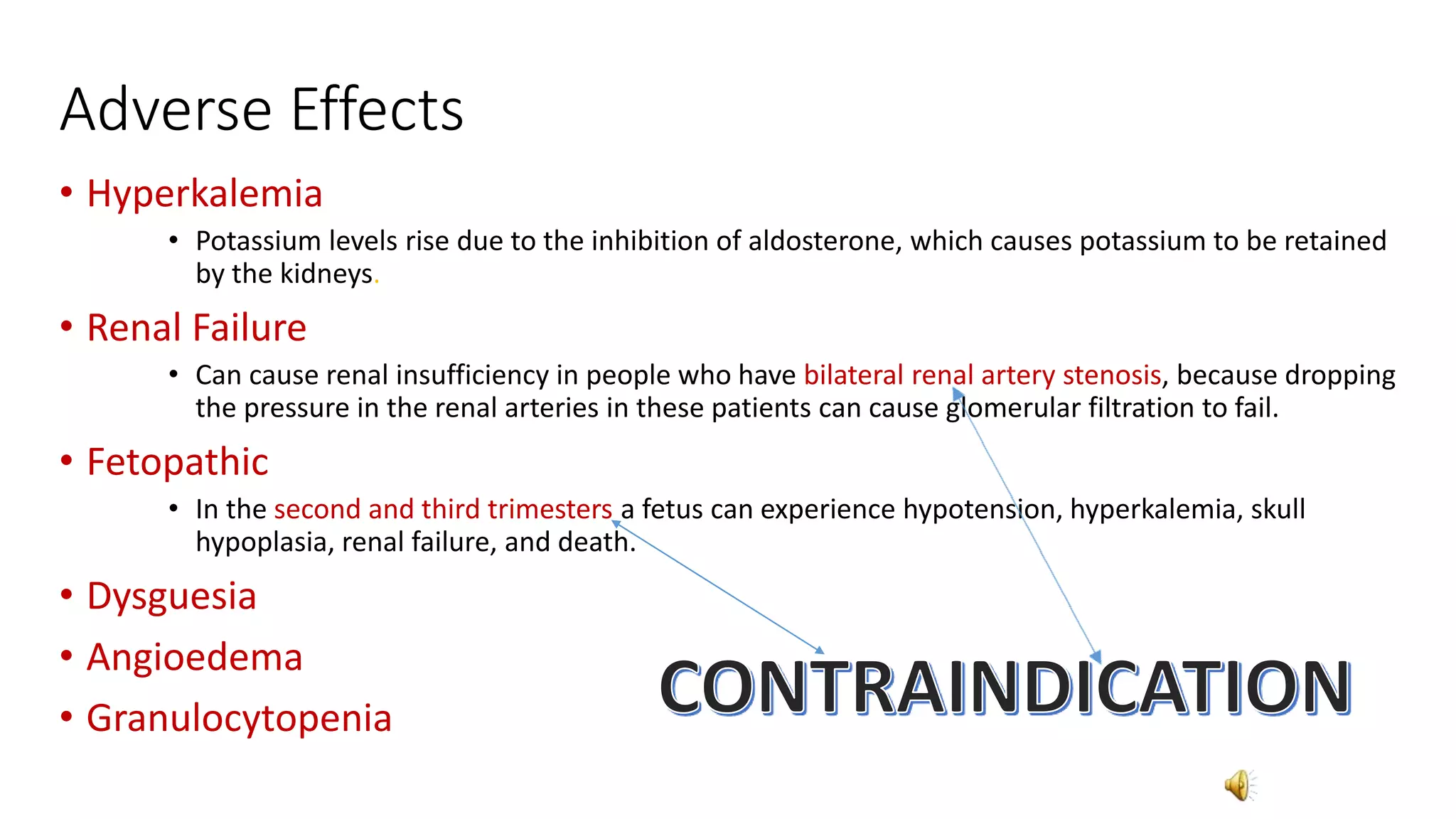
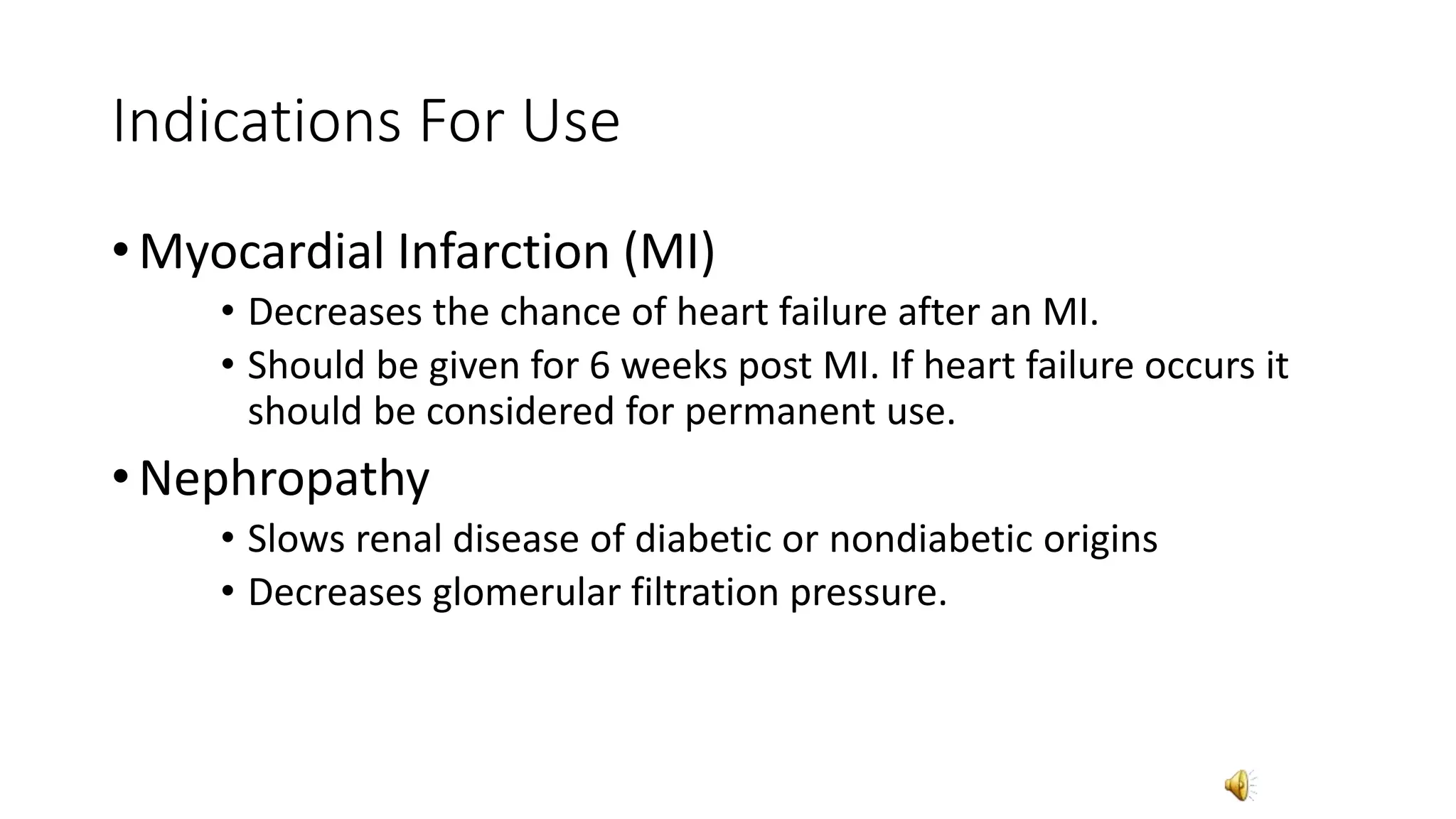
The patient in option c) would most likely be treated with an ACE inhibitor. ACE inhibitors are commonly used to treat hypertension in diabetics to help preserve renal function and reduce cardiovascular risk. Option a) would not be treated during pregnancy due to risk of fetal injury. Option b) has multiple issues including renal failure where ACE inhibitors could further impair renal function. Option d) has septic shock where ACE inhibitors could worsen hypotension.
The lab value in option b) of potassium 5.6 would be a contraindication for taking an ACE inhibitor as it could cause potentially fatal hyperkalemia by inhibiting aldosterone. Options a), c), and d) have normal or non-concerning lab values.


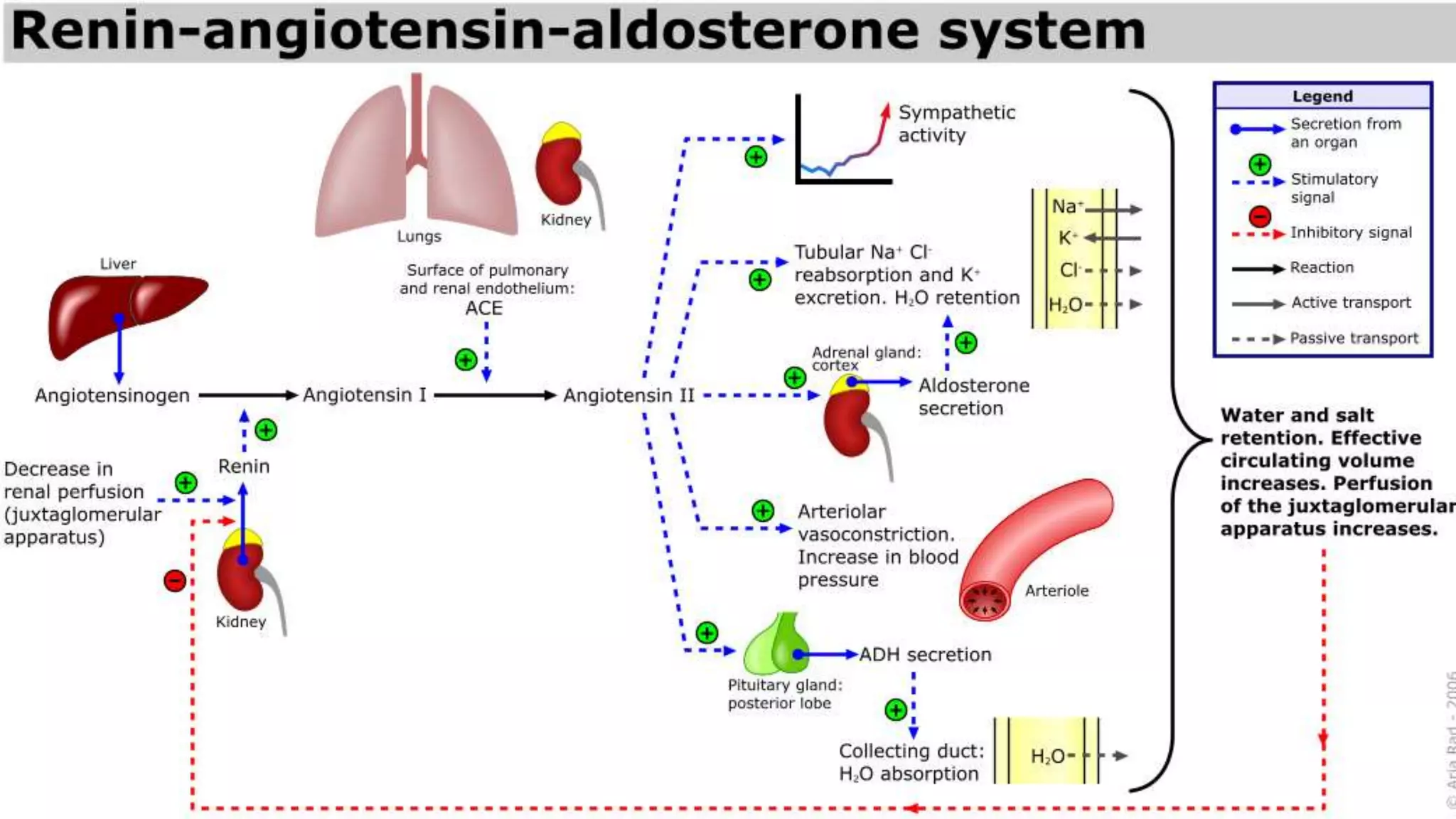


![• AII has several very important functions:
• Constricts resistance vessels (via AII [AT1] receptors) thereby
increasing systemic vascular resistance andarterial pressure
• Stimulates sodium transport (reabsorption) at several renal tubular
sites, thereby increasing sodium and water retention by the body
• Acts on the adrenal cortex to release aldosterone, which in turn acts
on the kidneys to increase sodium and fluid retention](https://image.slidesharecdn.com/ace-160506040136/75/Ace-6-2048.jpg)