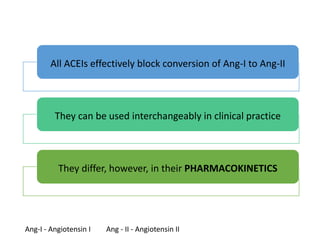
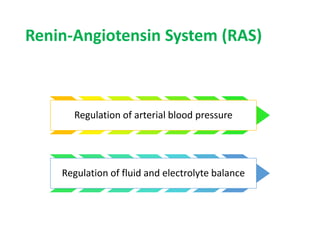
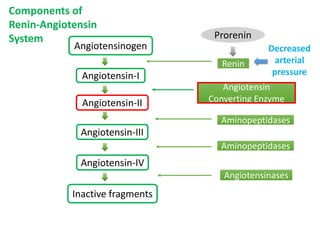
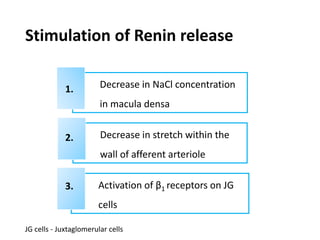
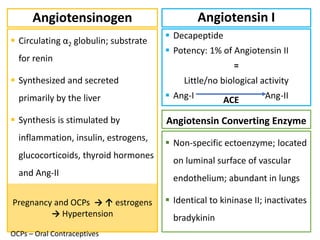
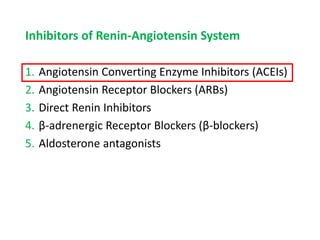
1. Angiotensin converting enzyme inhibitors (ACEIs) block the conversion of angiotensin I to angiotensin II, inhibiting the renin-angiotensin system.
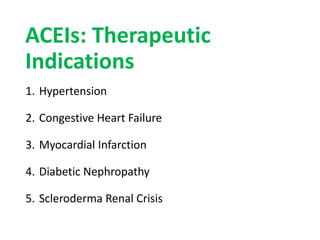
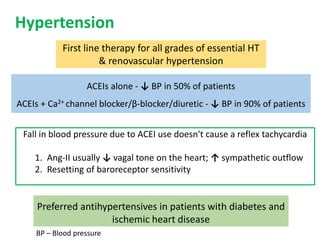
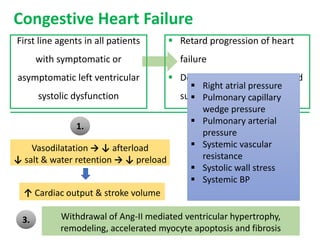
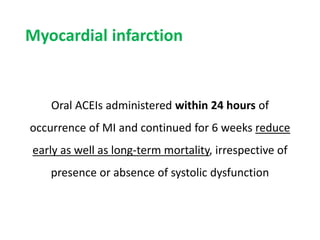
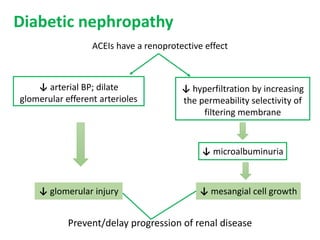
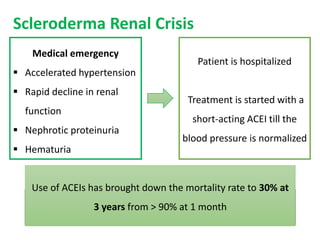
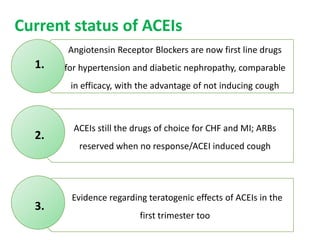
2. ACEIs are used to treat hypertension, congestive heart failure, myocardial infarction, diabetic nephropathy, and scleroderma renal crisis.
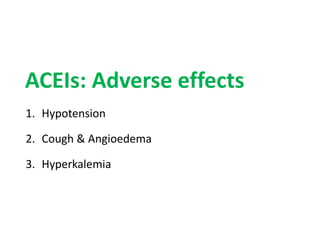
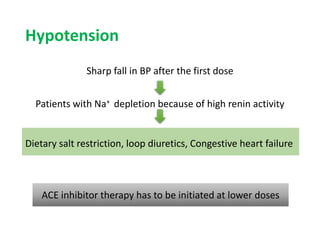
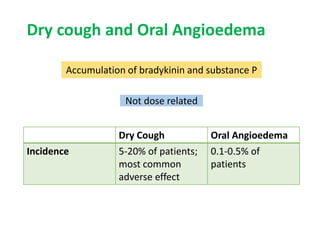
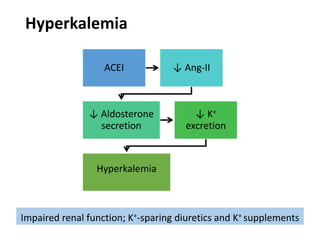
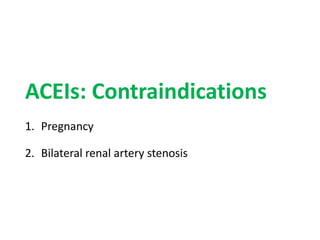
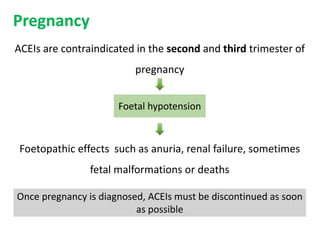
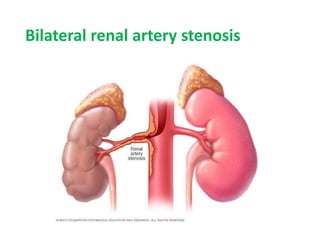
3. Common adverse effects of ACEIs include hypotension, cough, and hyperkalemia. ACEIs are contraindicated in pregnancy and bilateral renal artery stenosis due to risks of hypotension, renal failure, and fetal complications.