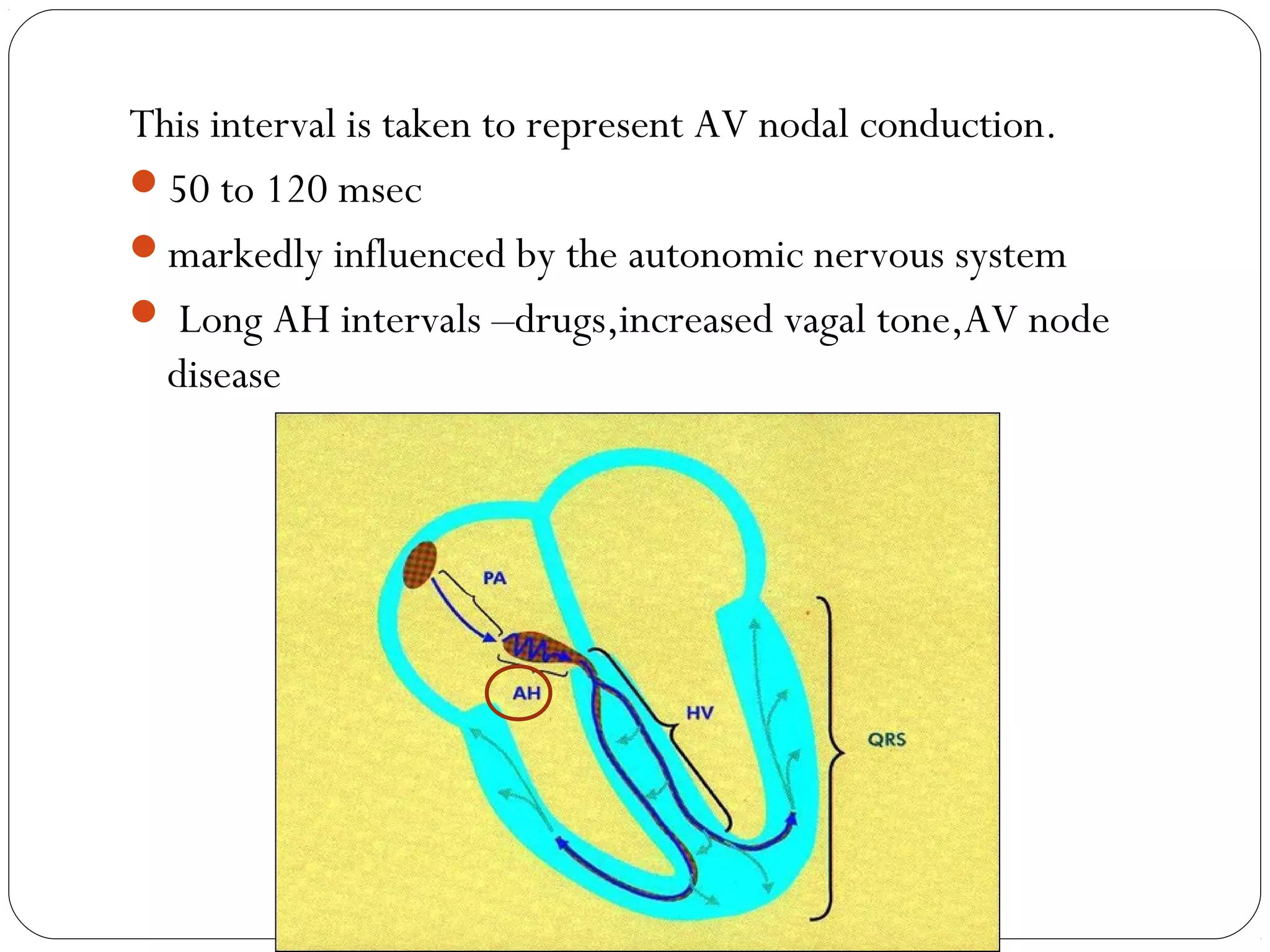
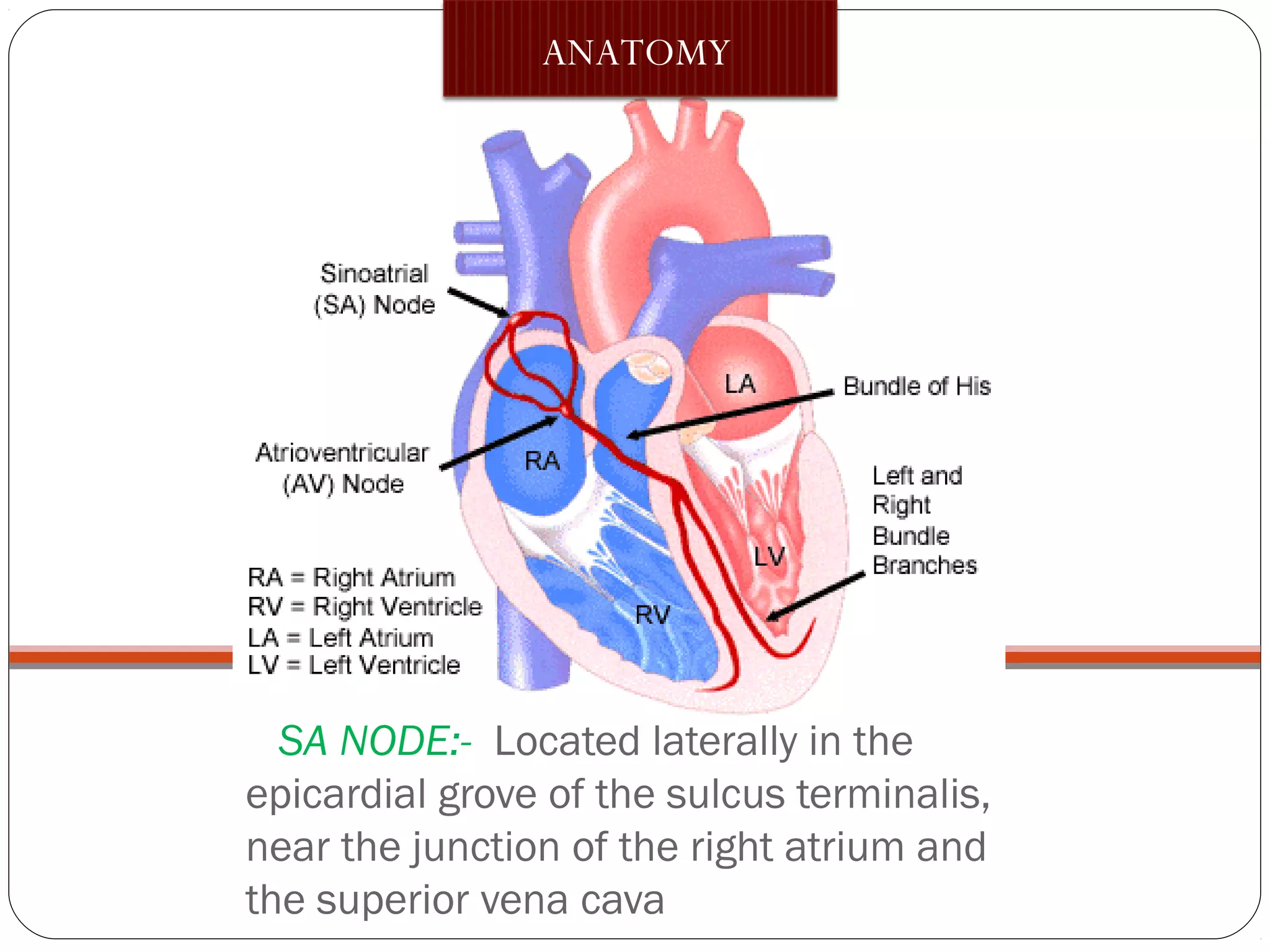
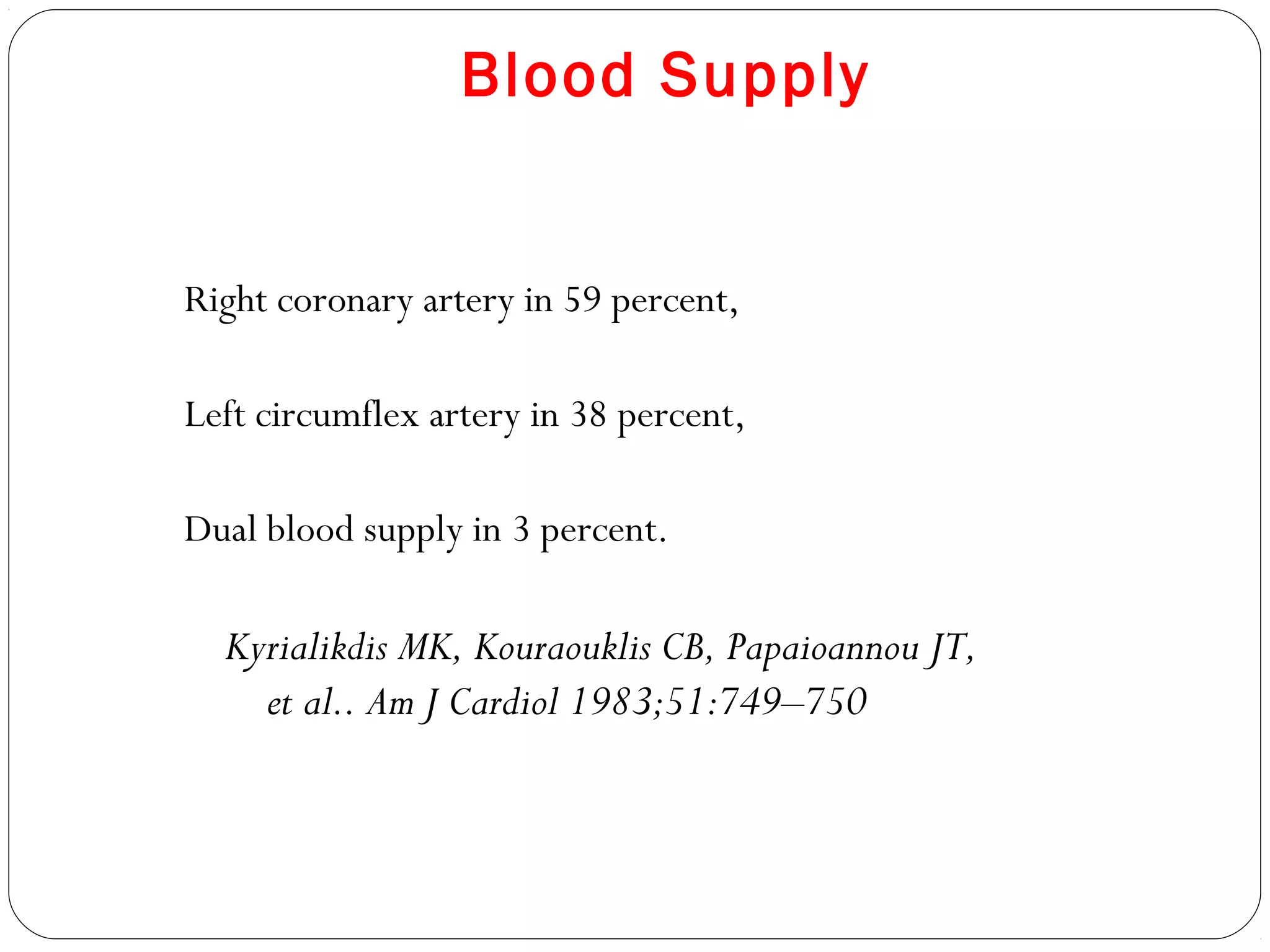
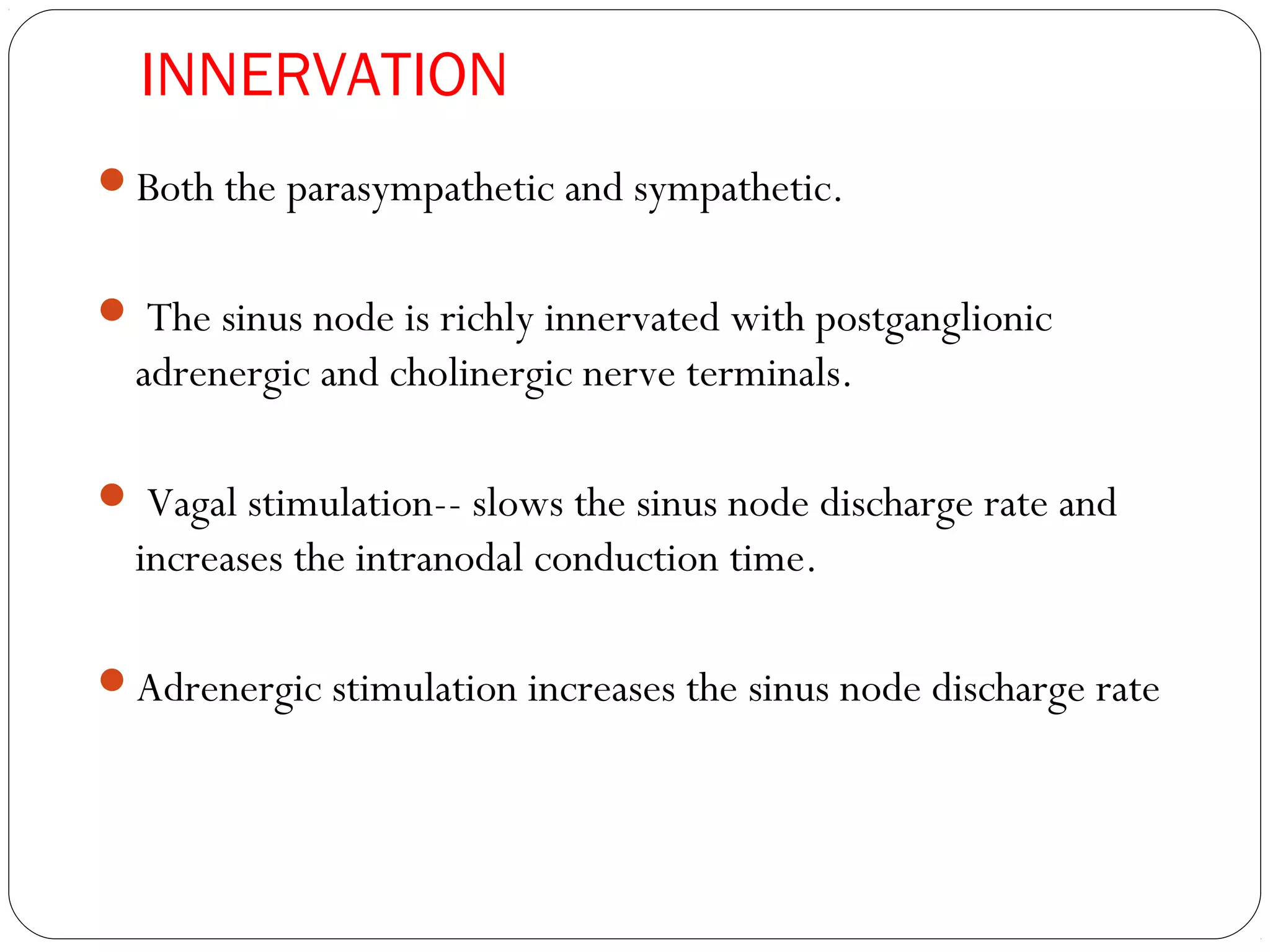
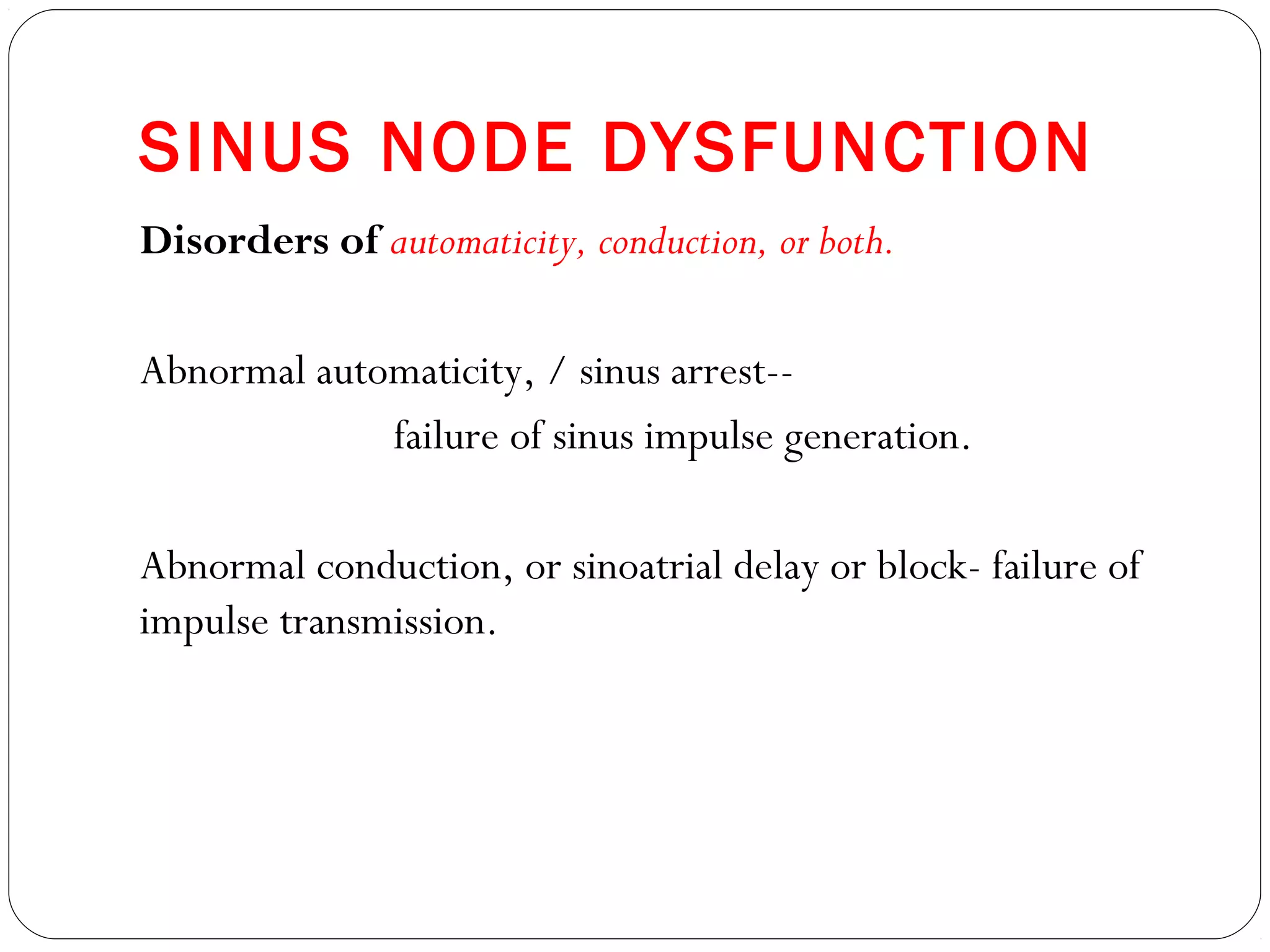
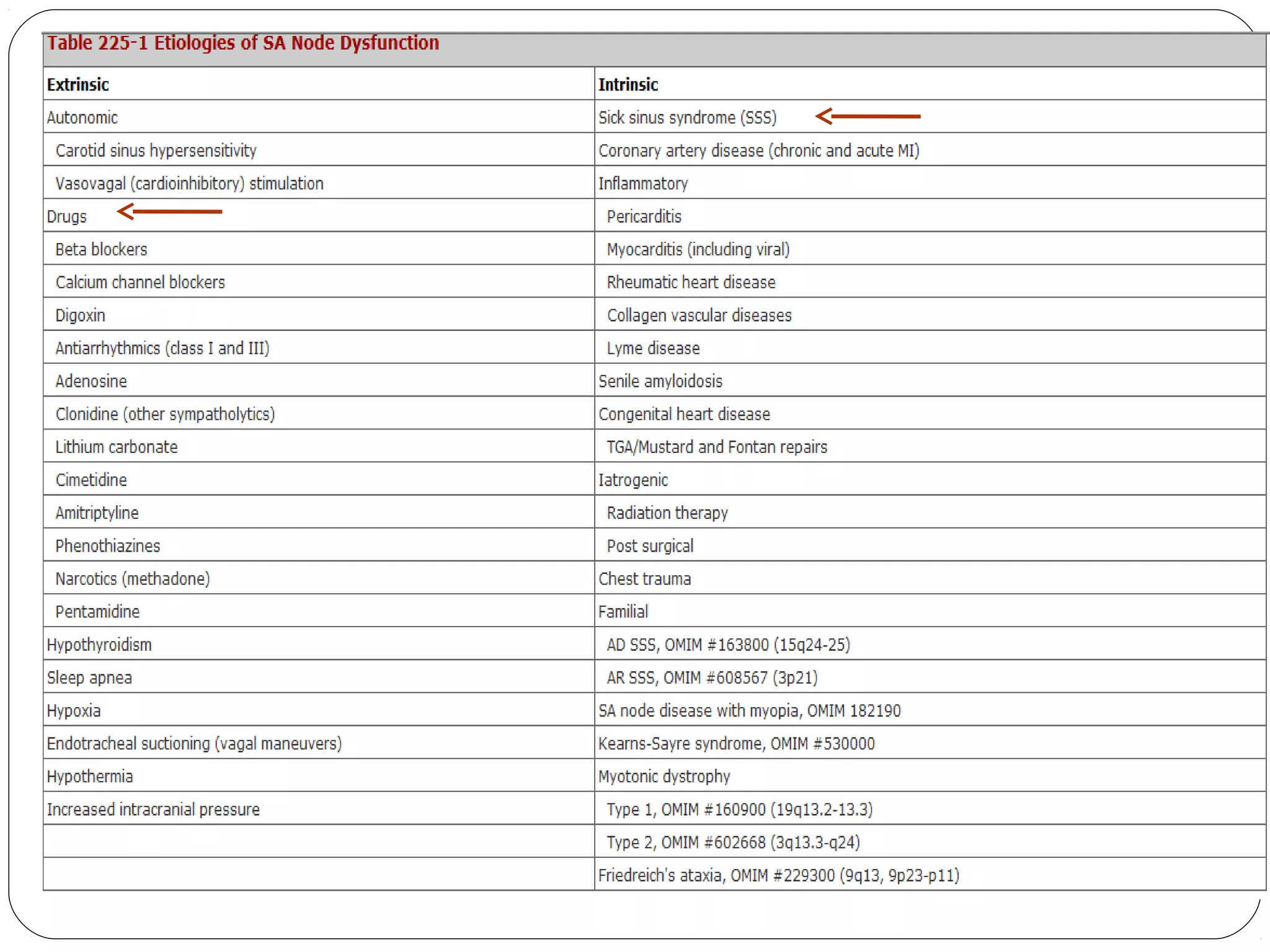
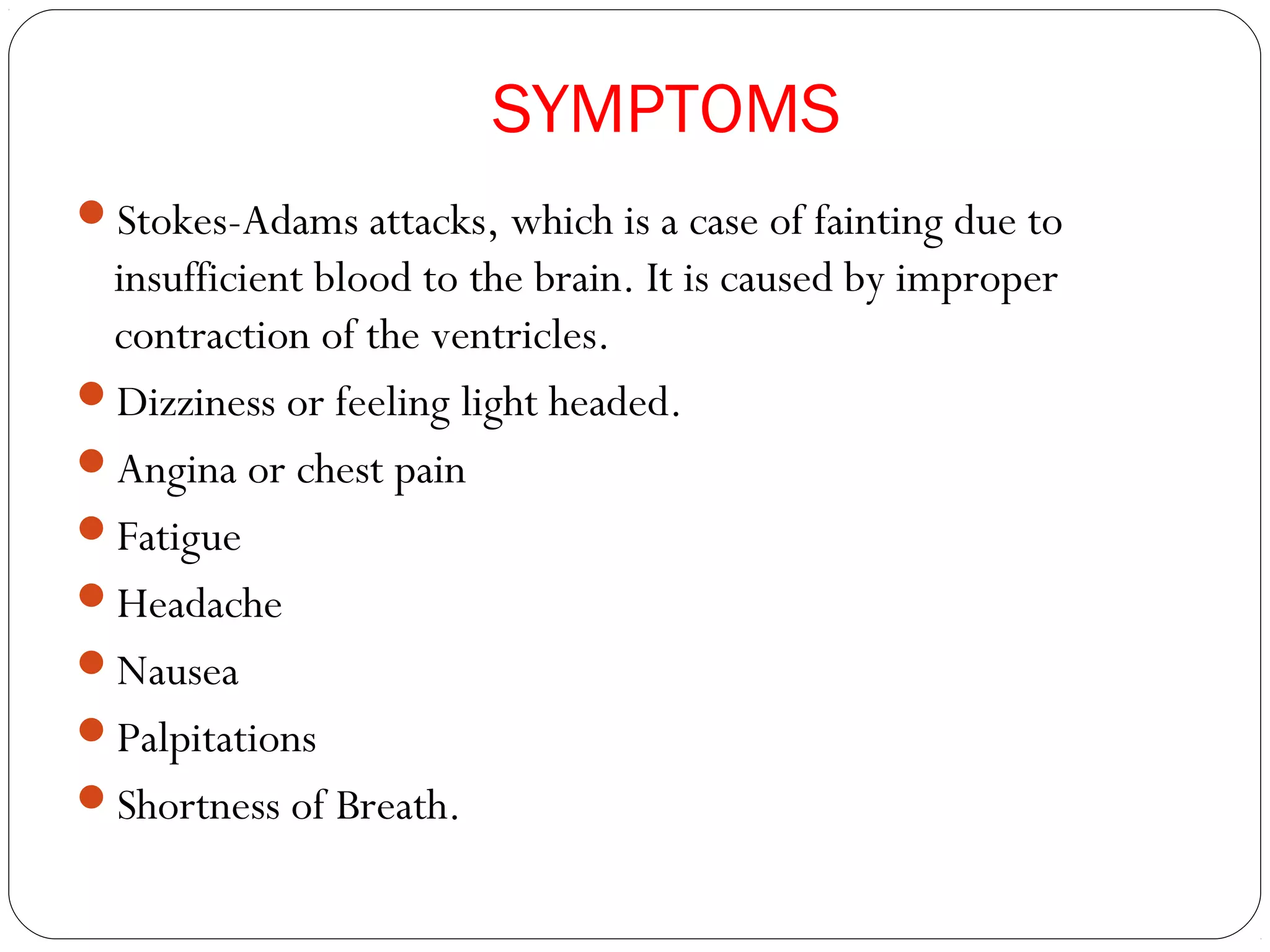
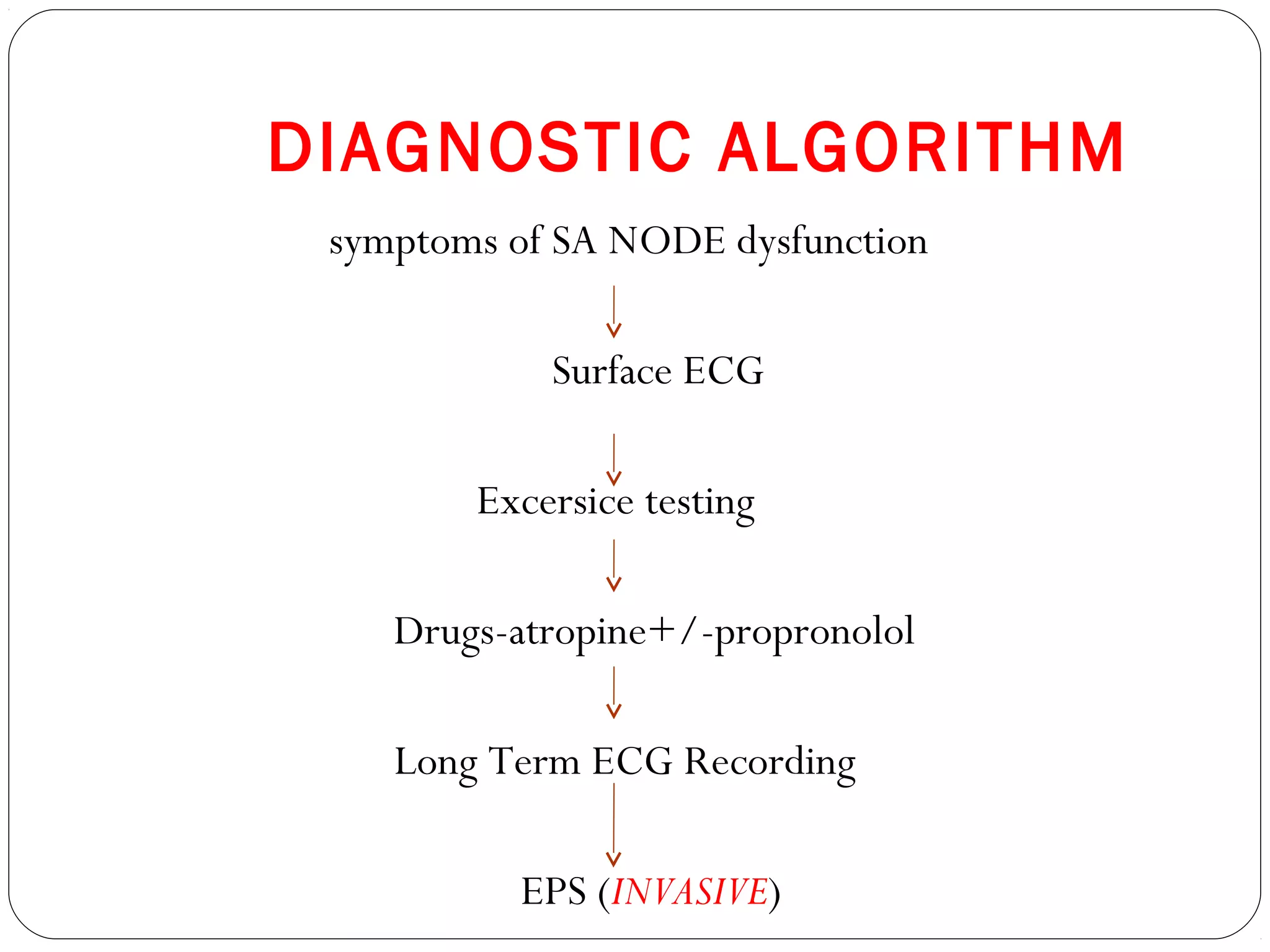
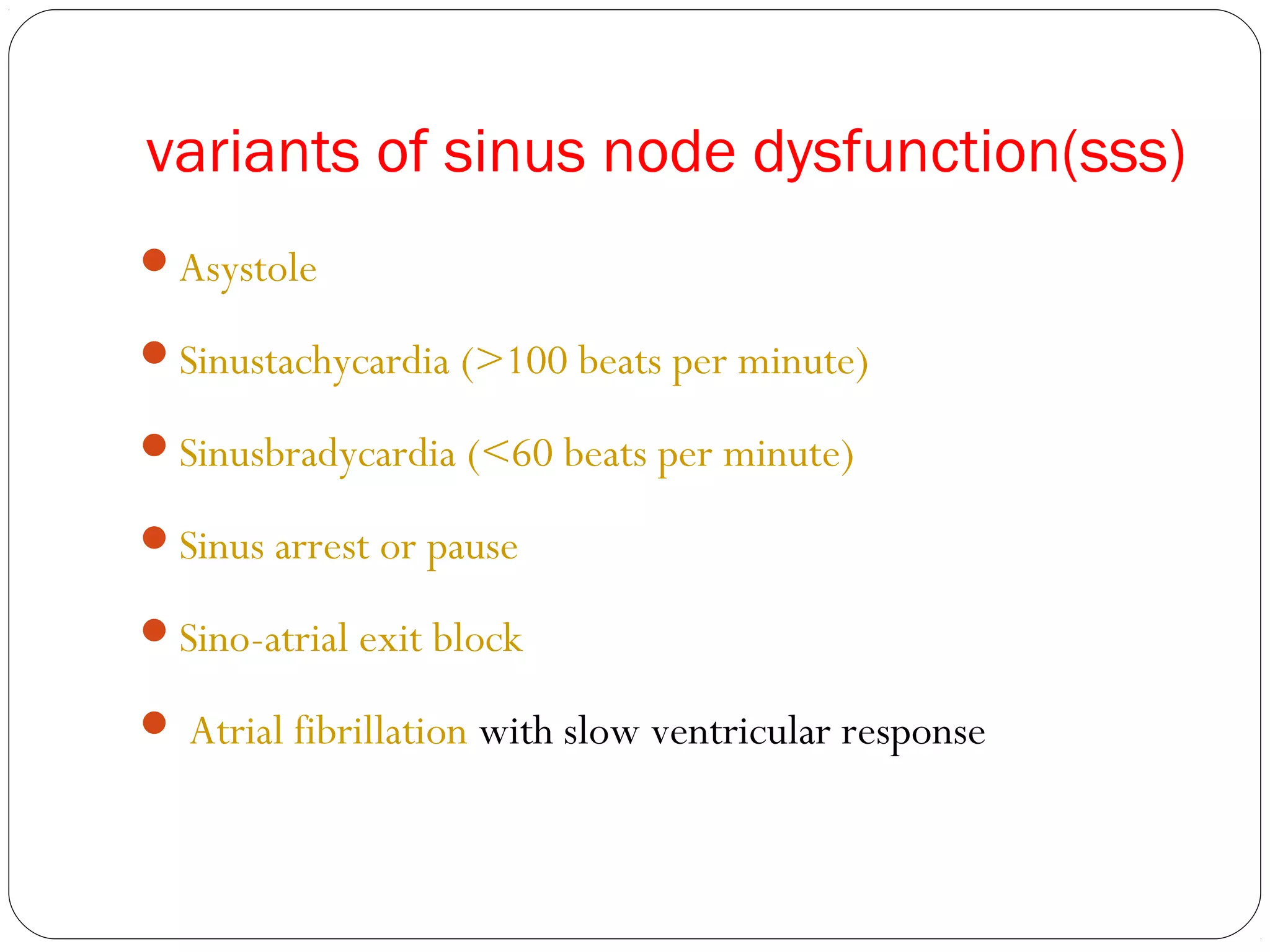
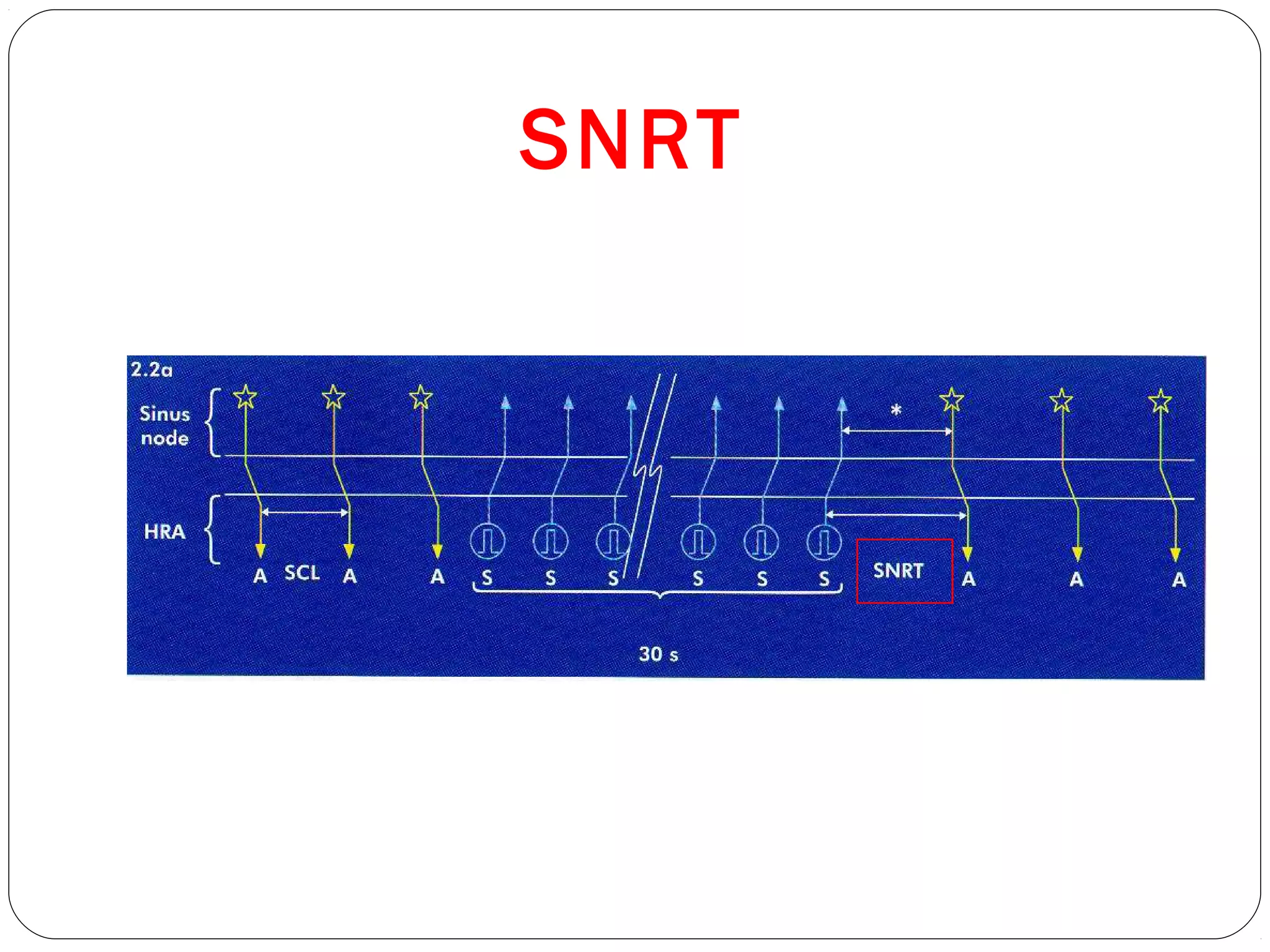
This document discusses the noninvasive and invasive assessment of the sinus node and atrioventricular node and its clinical relevance. It provides an overview of the sinus node, including its anatomy, innervation, and dysfunction. Symptoms of sinus node dysfunction are outlined. The diagnostic algorithm involves initial ECG and exercise testing, followed by drug challenges and long-term monitoring if needed. Invasive electrophysiological studies include sinus node recovery time testing and sinoatrial conduction time measurements to further evaluate patients. Correlation of these test results with ECG findings can help identify appropriate treatment options.
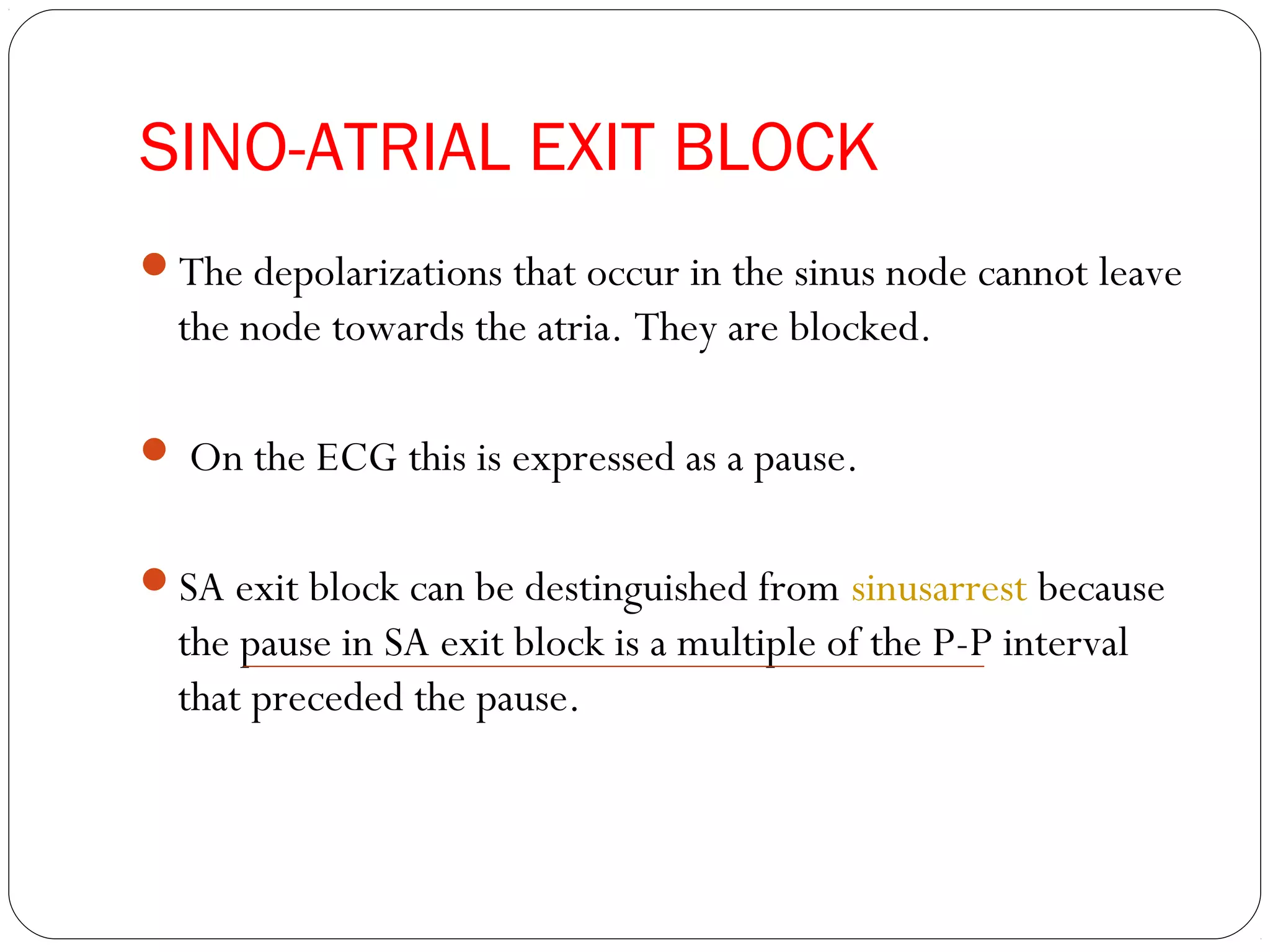
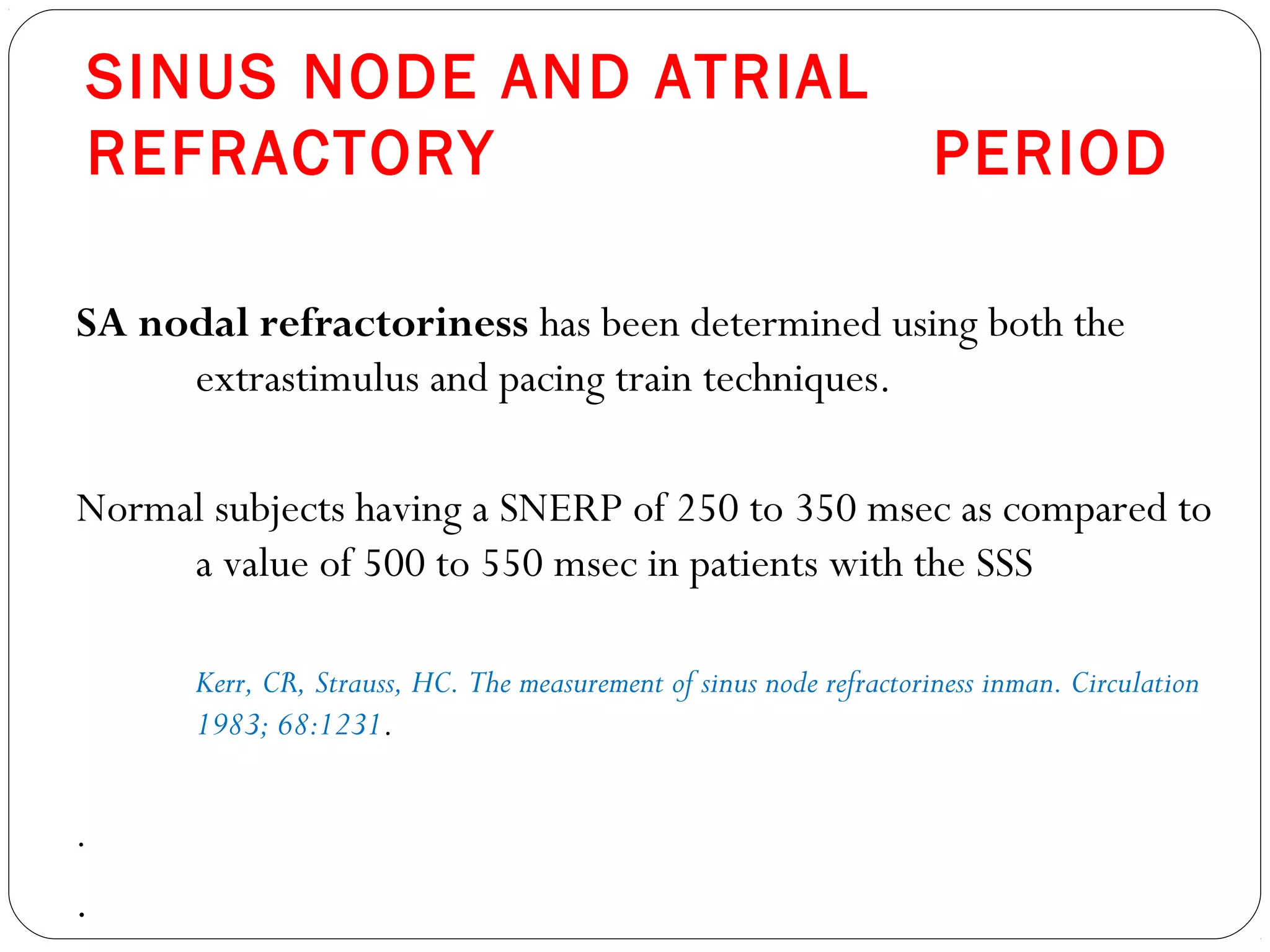
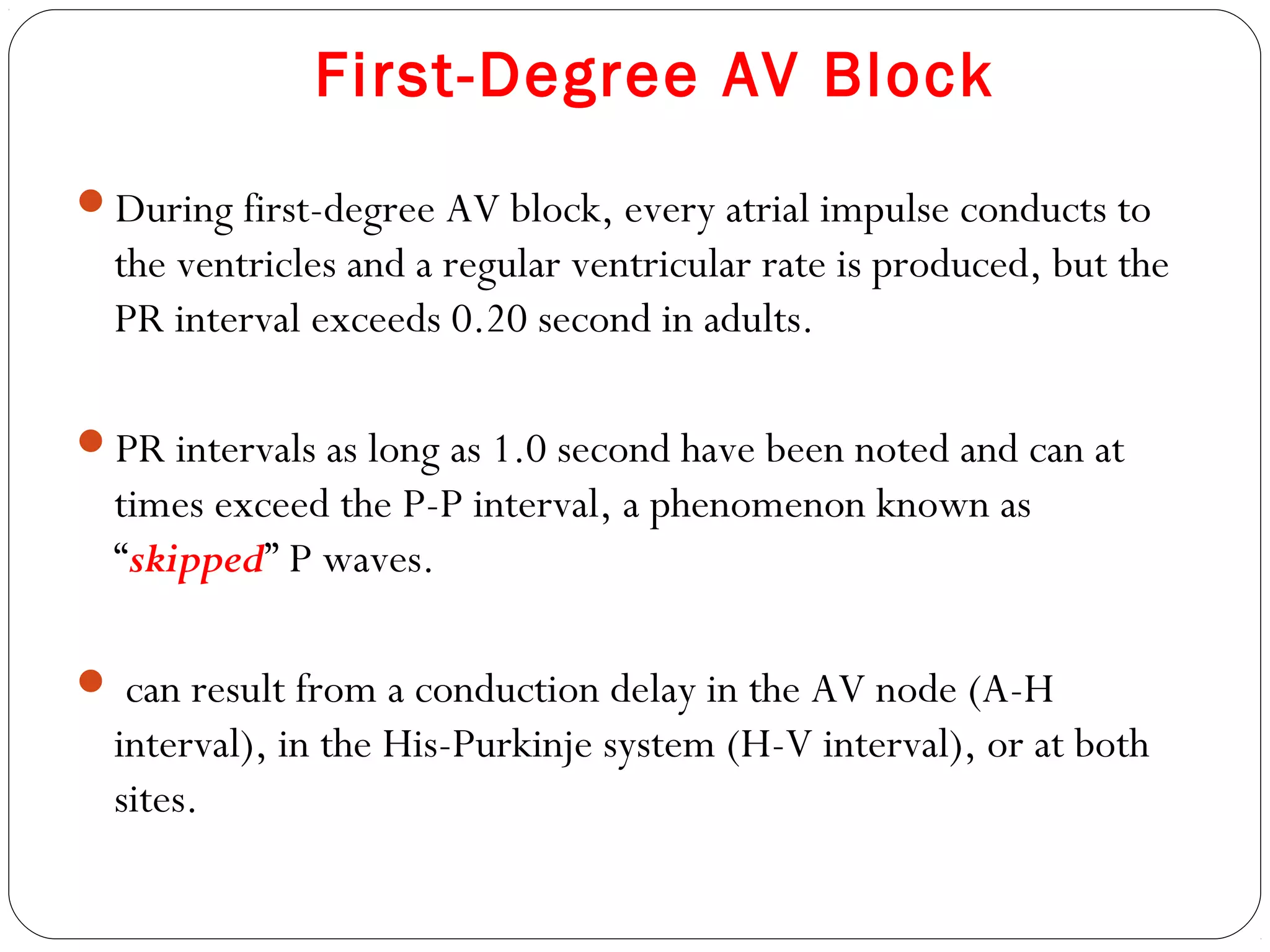
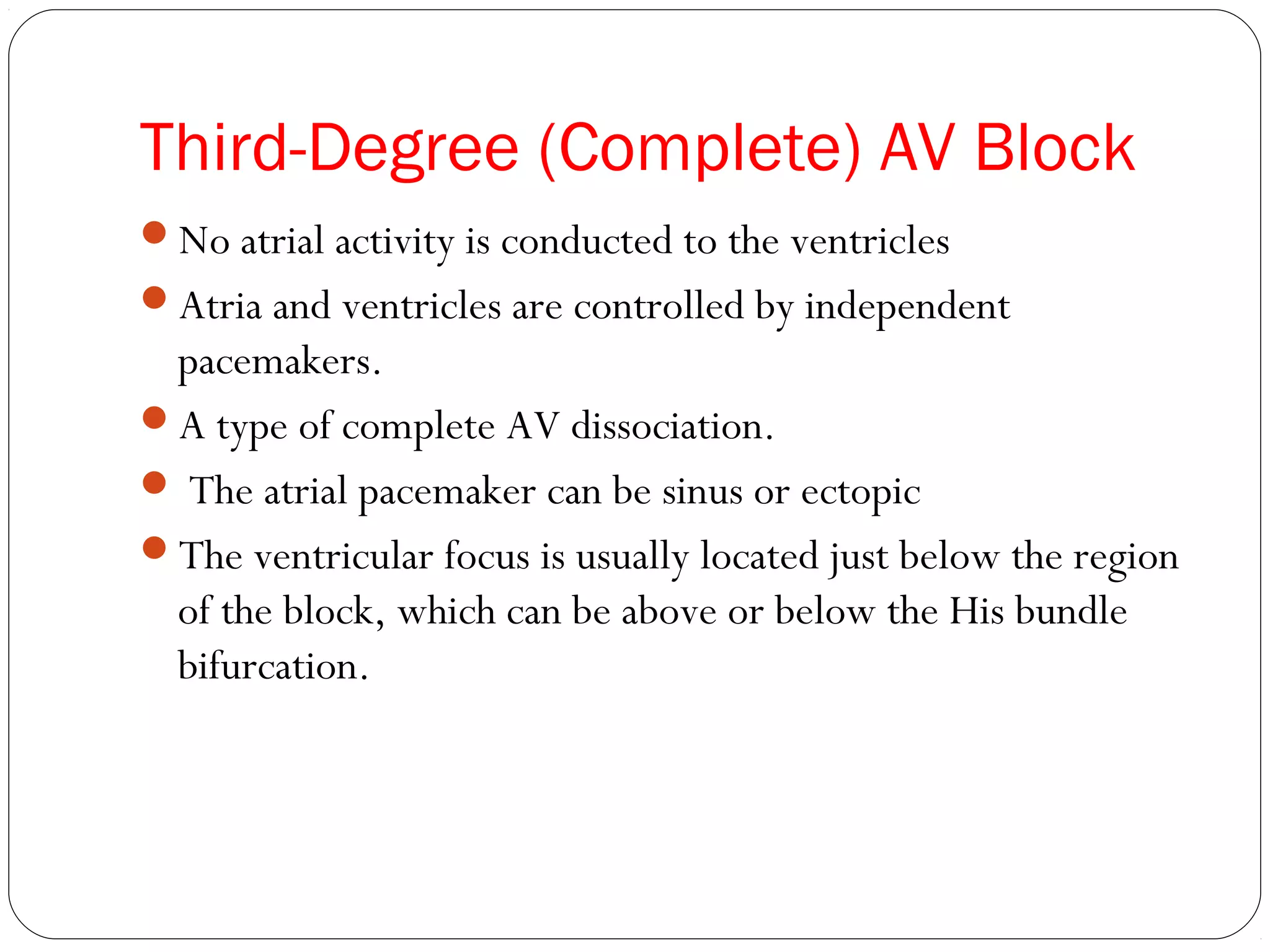
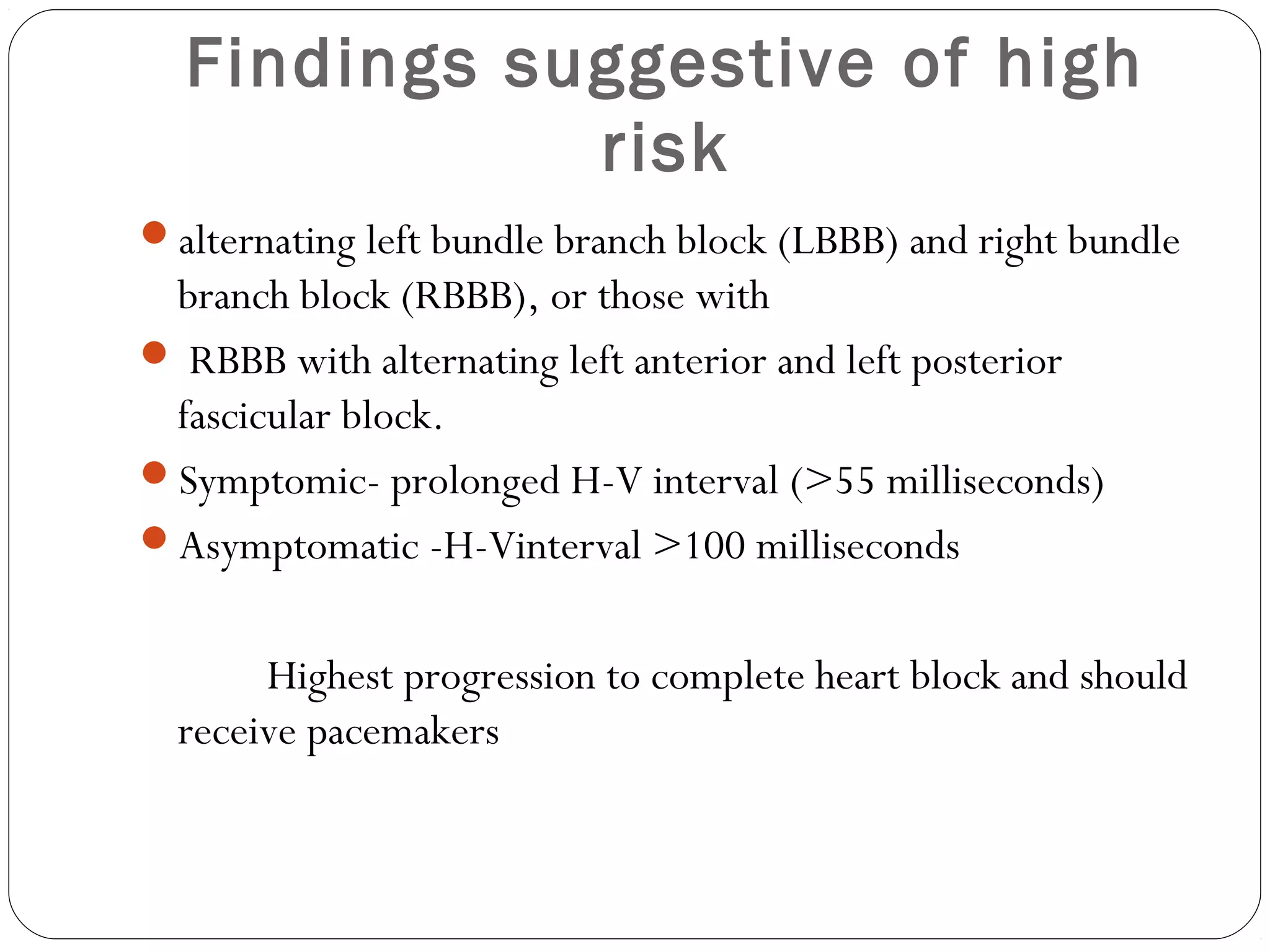
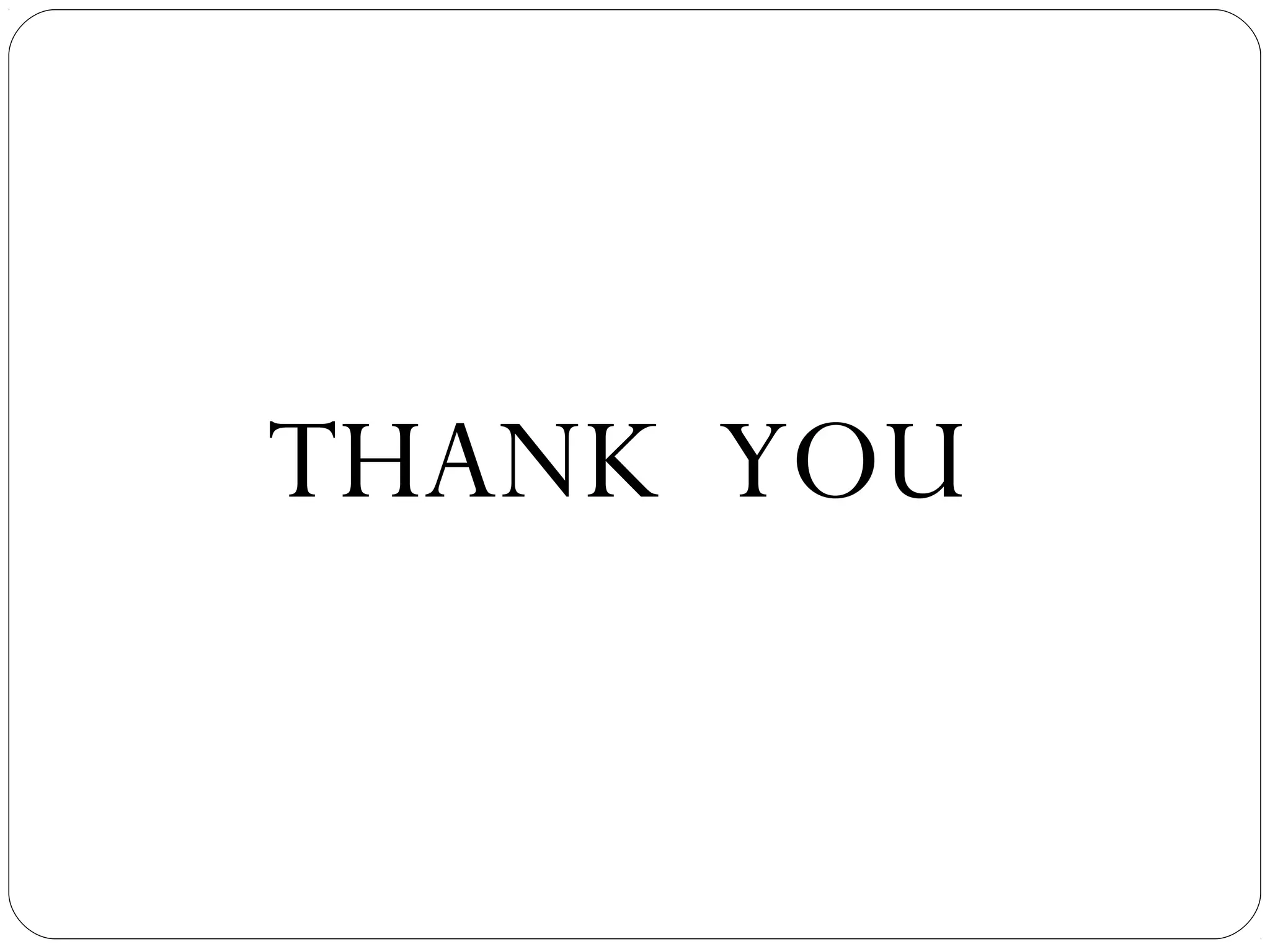
![PHARMACOLOGICAL
DENERVATION
Intrinsic heart rate — Atropine (0.04 mg/kg) and
propranolol (0.2 mg/kg)
Heart rate at 30 minutes is called the (IHR) .
The IHR is a function of age
IHR, in beats/min = 117.2 - [0.53 x age]
IHR separates intrinsic SSS from extrinsic SSS
Intrinsic SSS is presumed to be present if the sinus rate does not
exceed the predicted IHR after atropine.](https://image.slidesharecdn.com/assessmentofsanodeandavnode-dr-150621174919-lva1-app6891/75/Assessment-of-sa-node-and-av-node-dr-i-tammi-raju-28-2048.jpg)
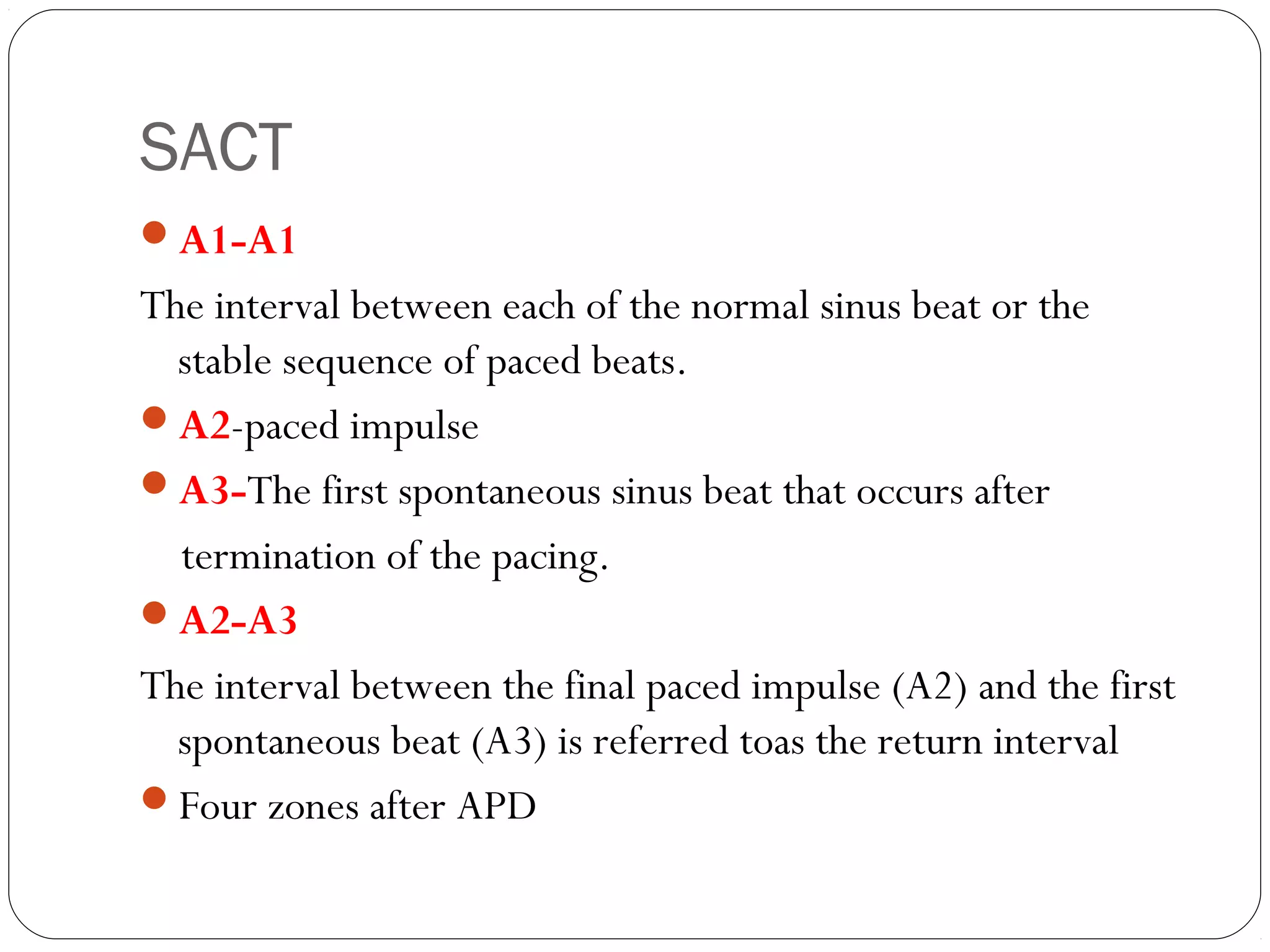
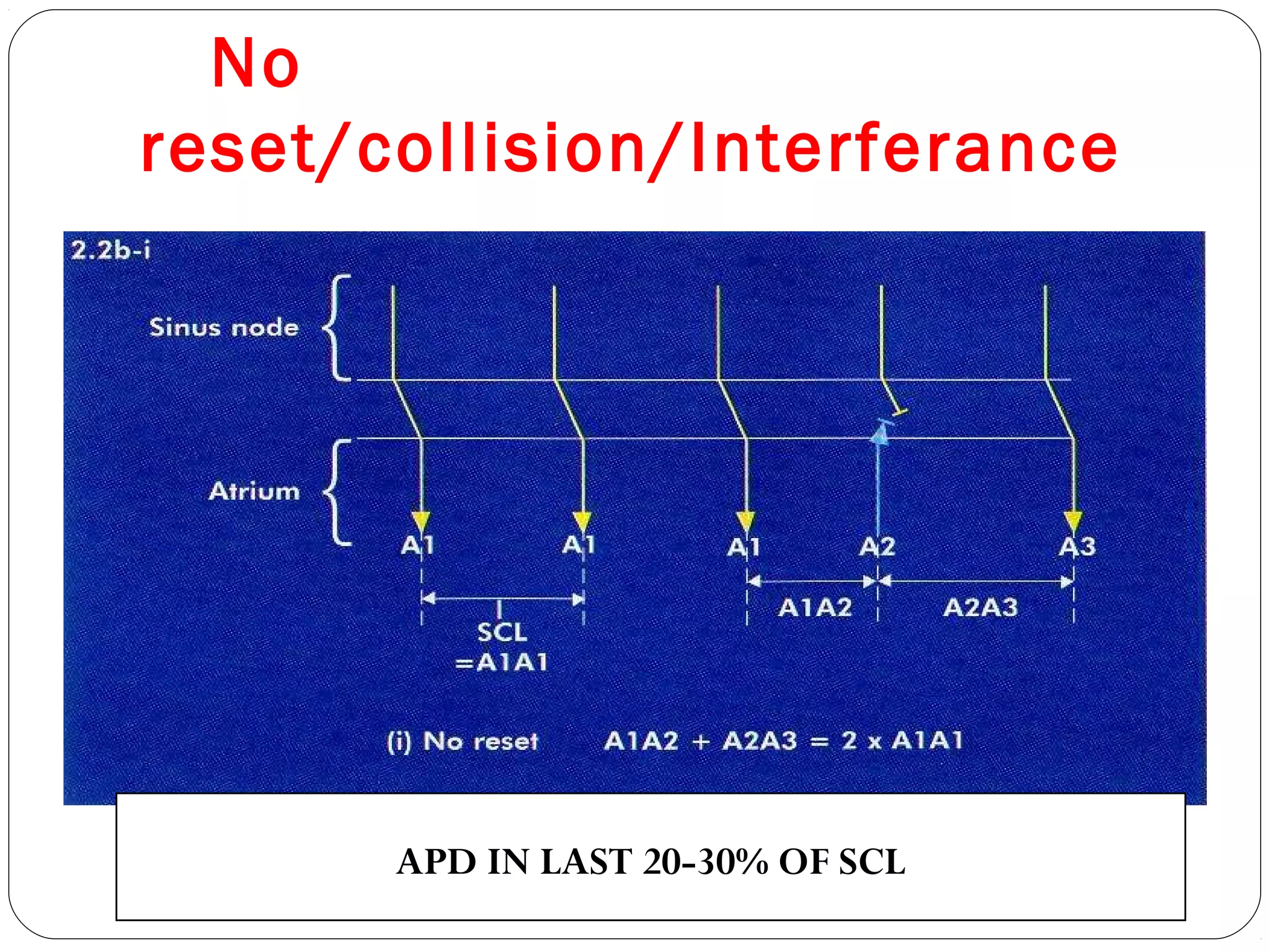
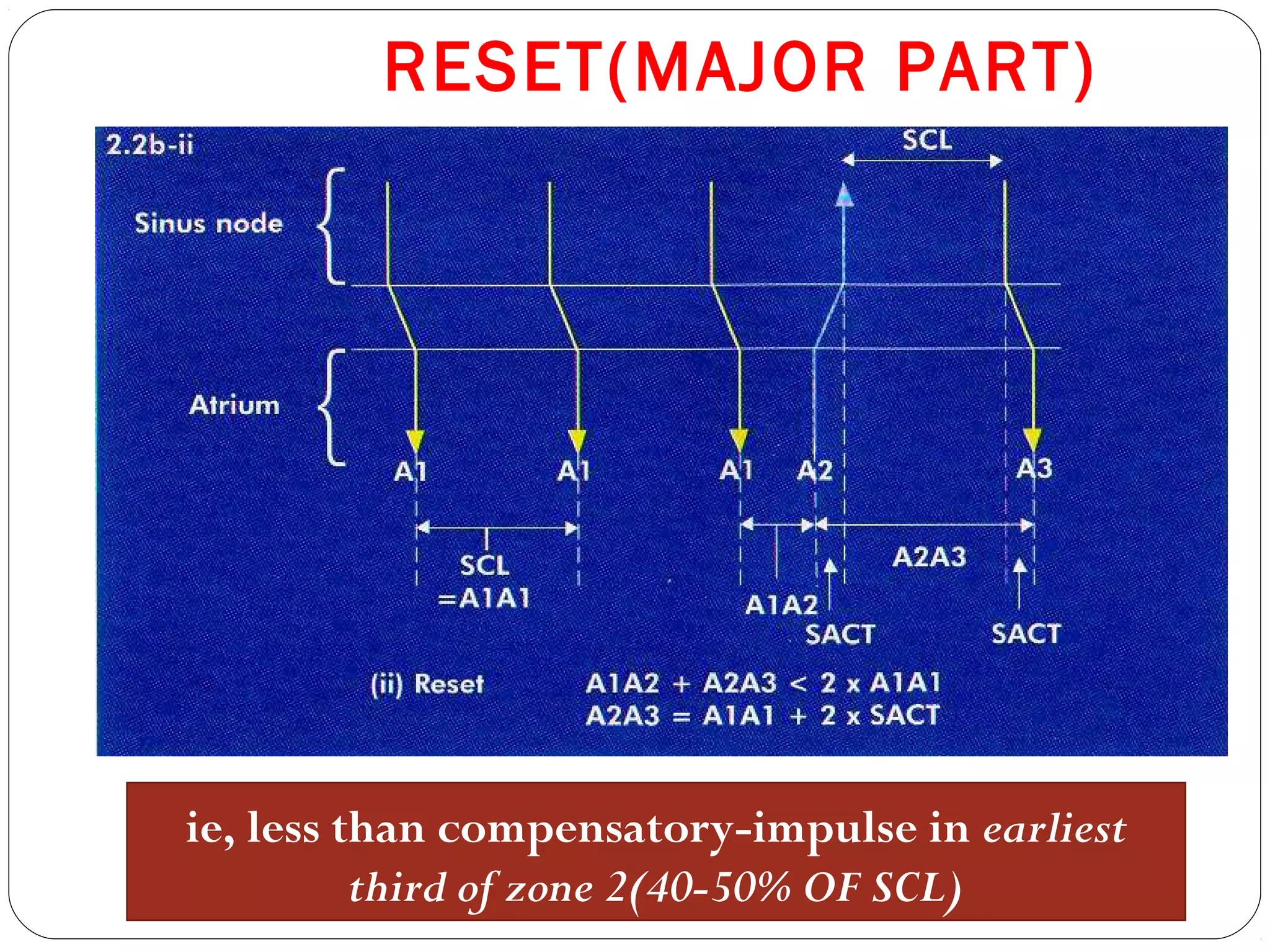
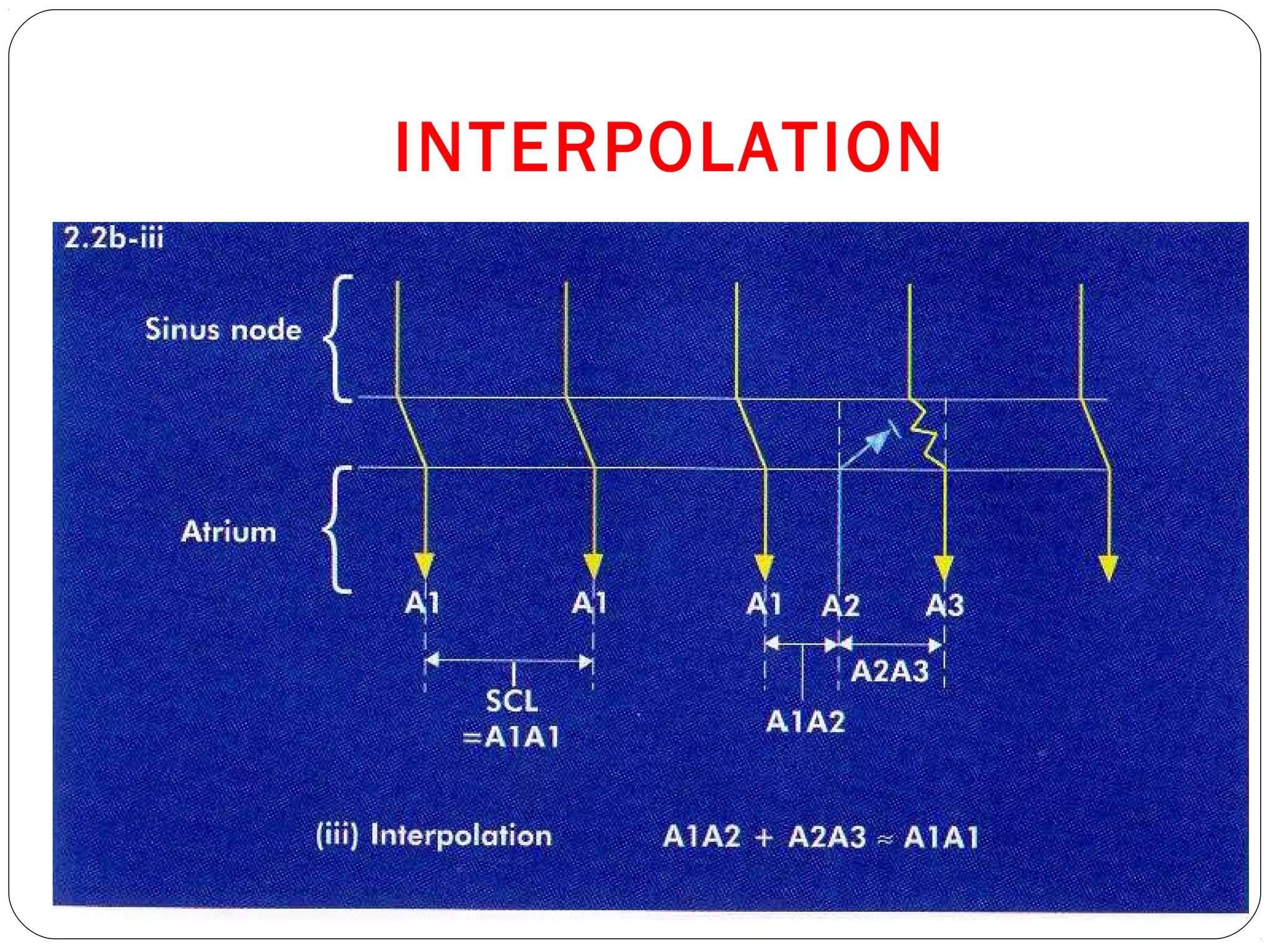
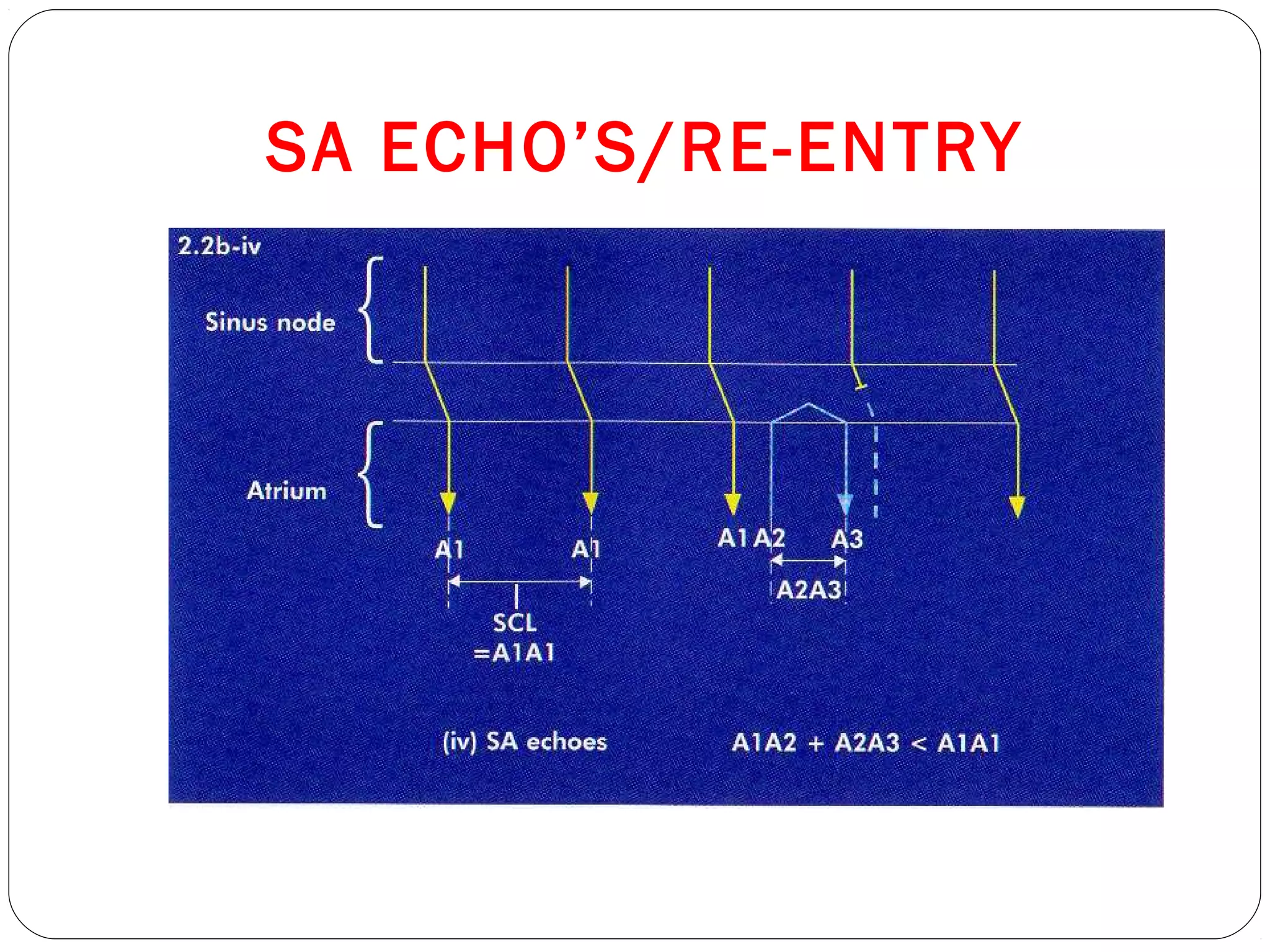
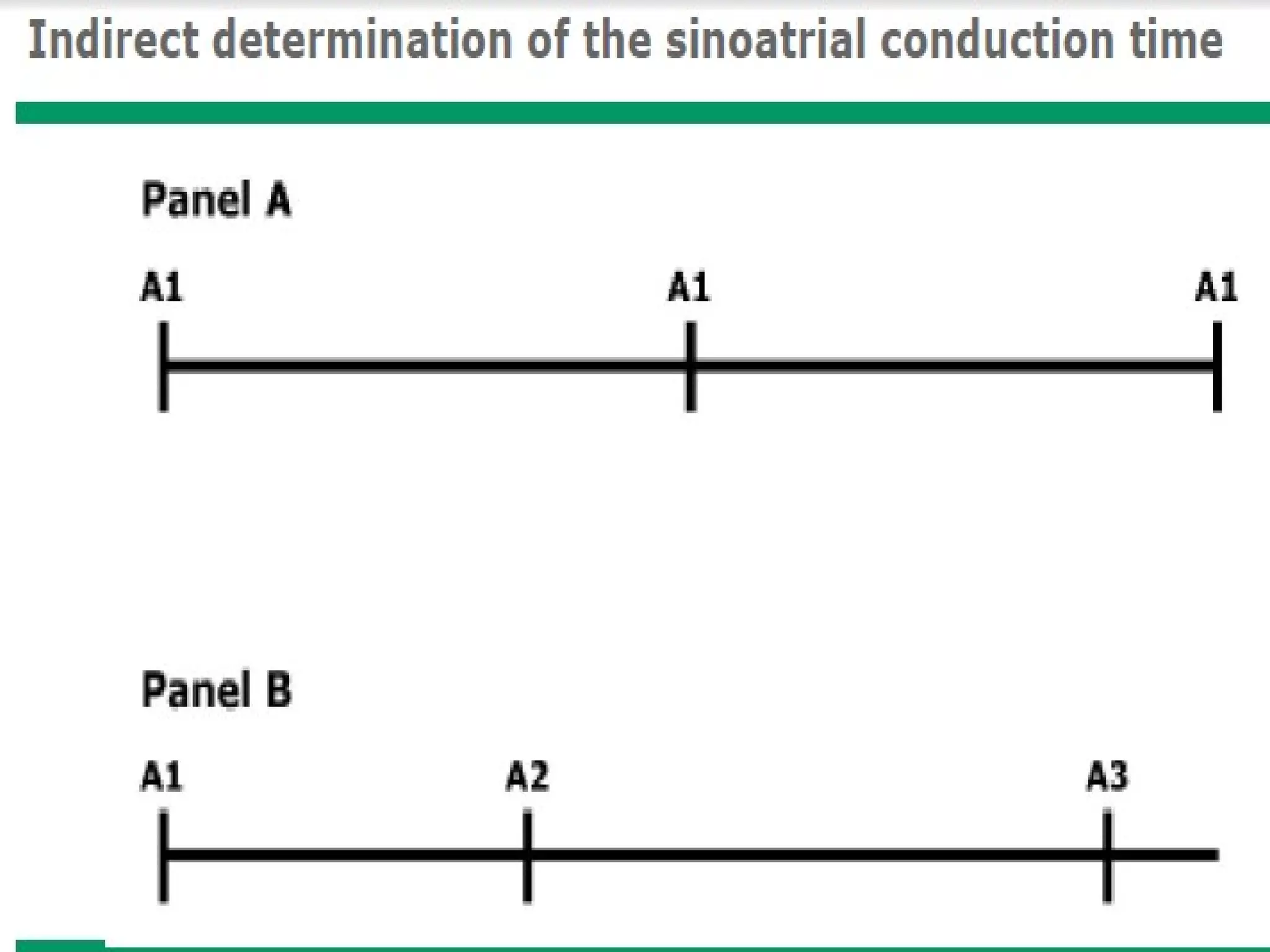
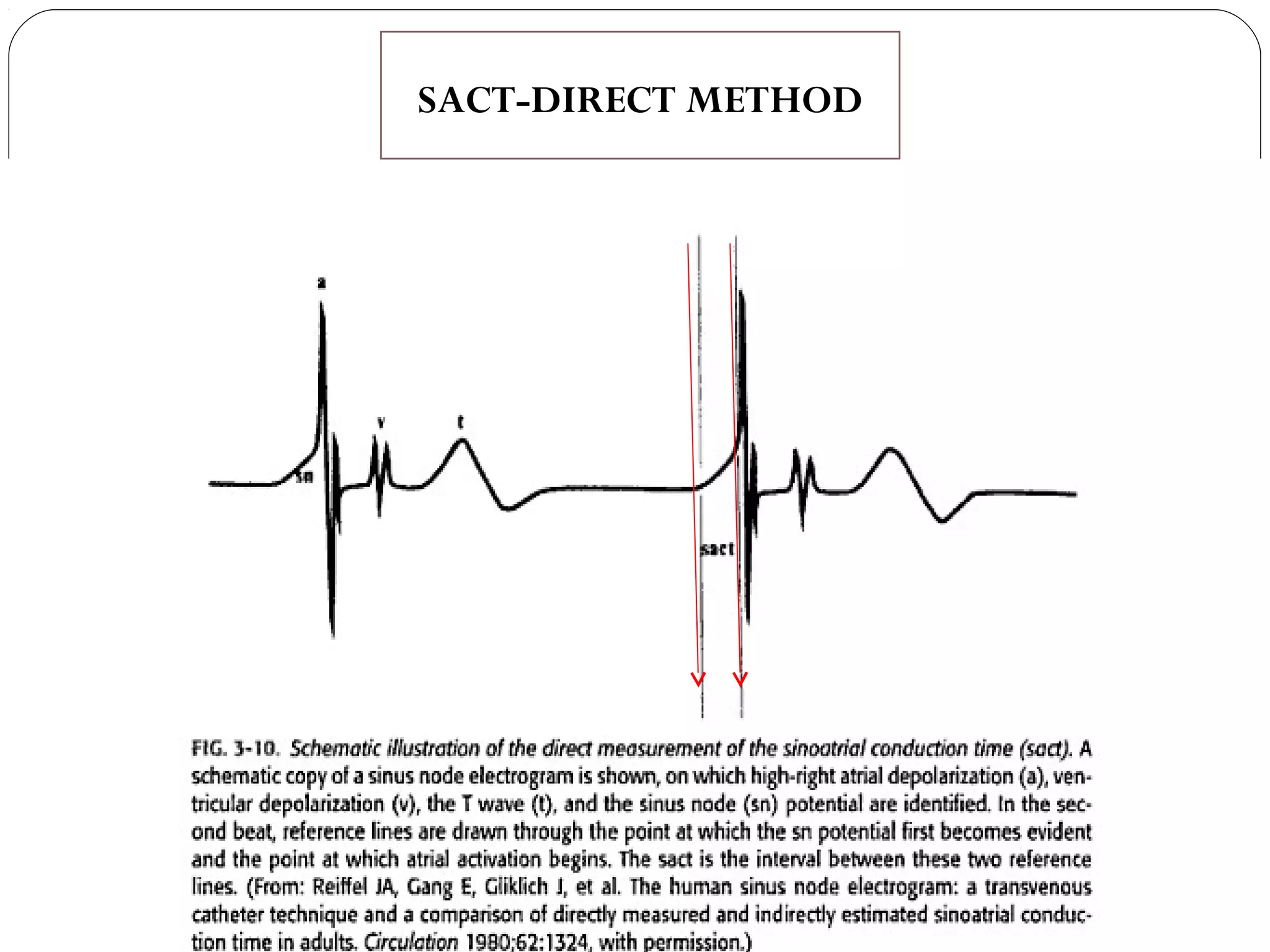
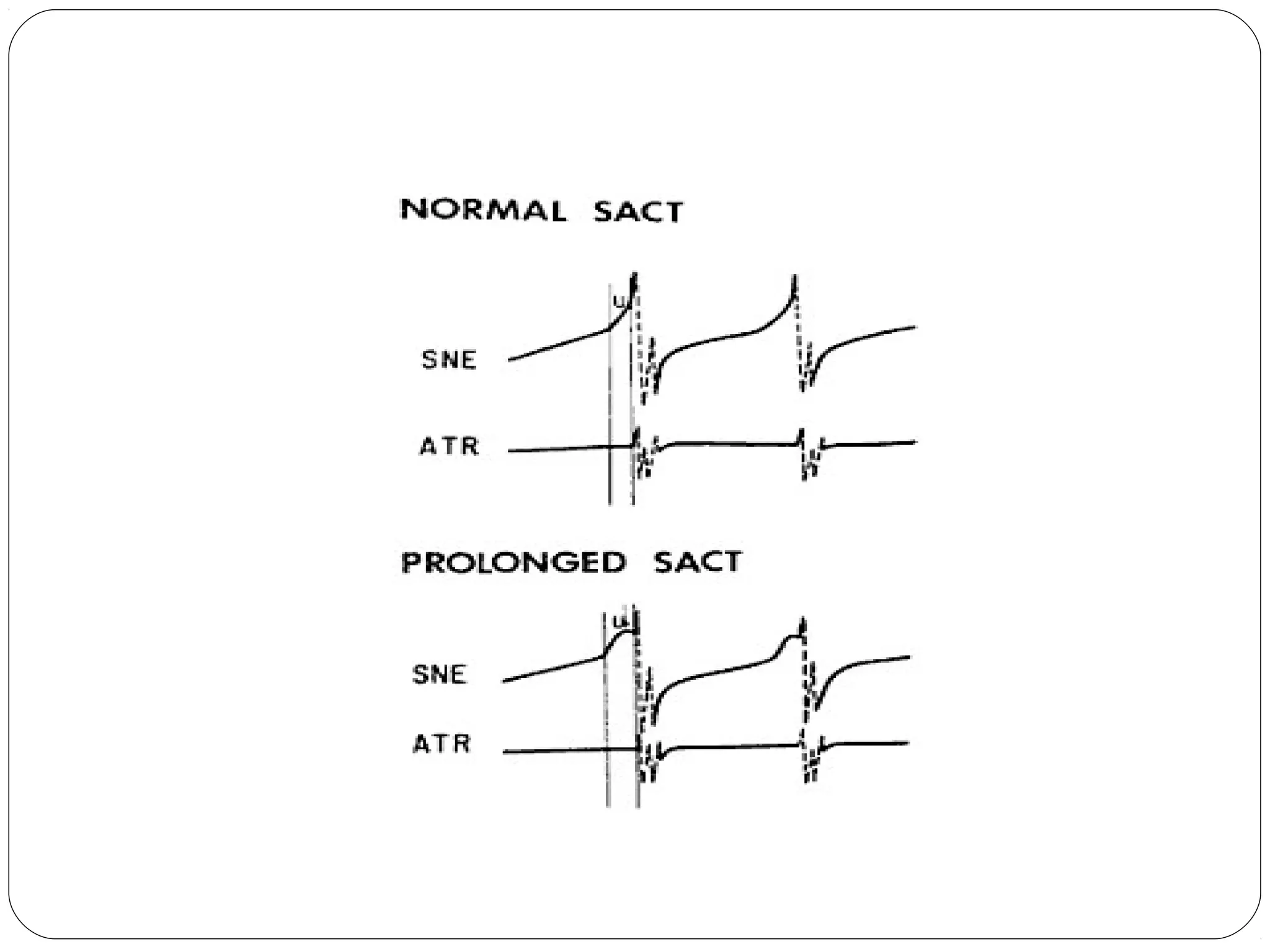
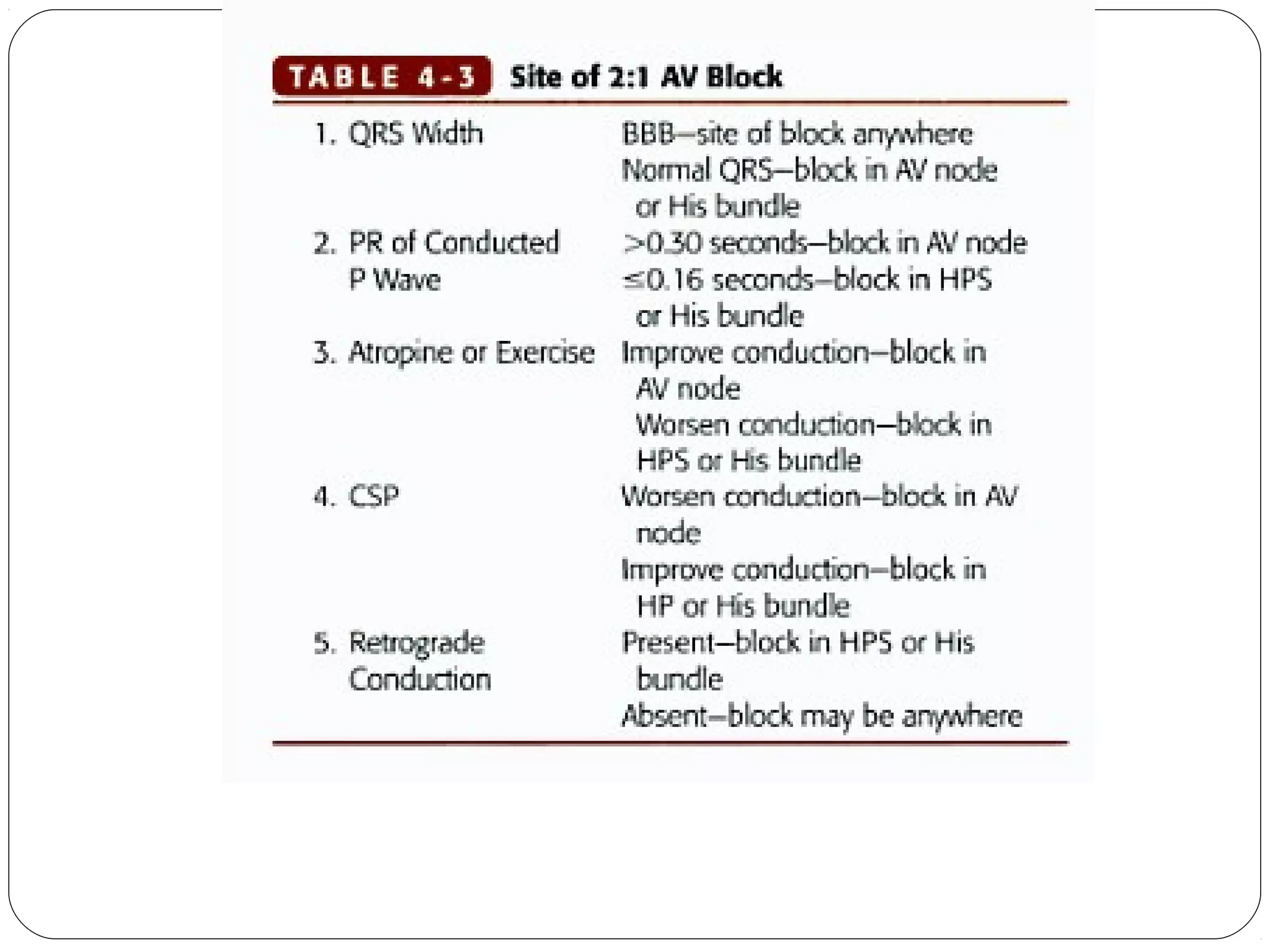
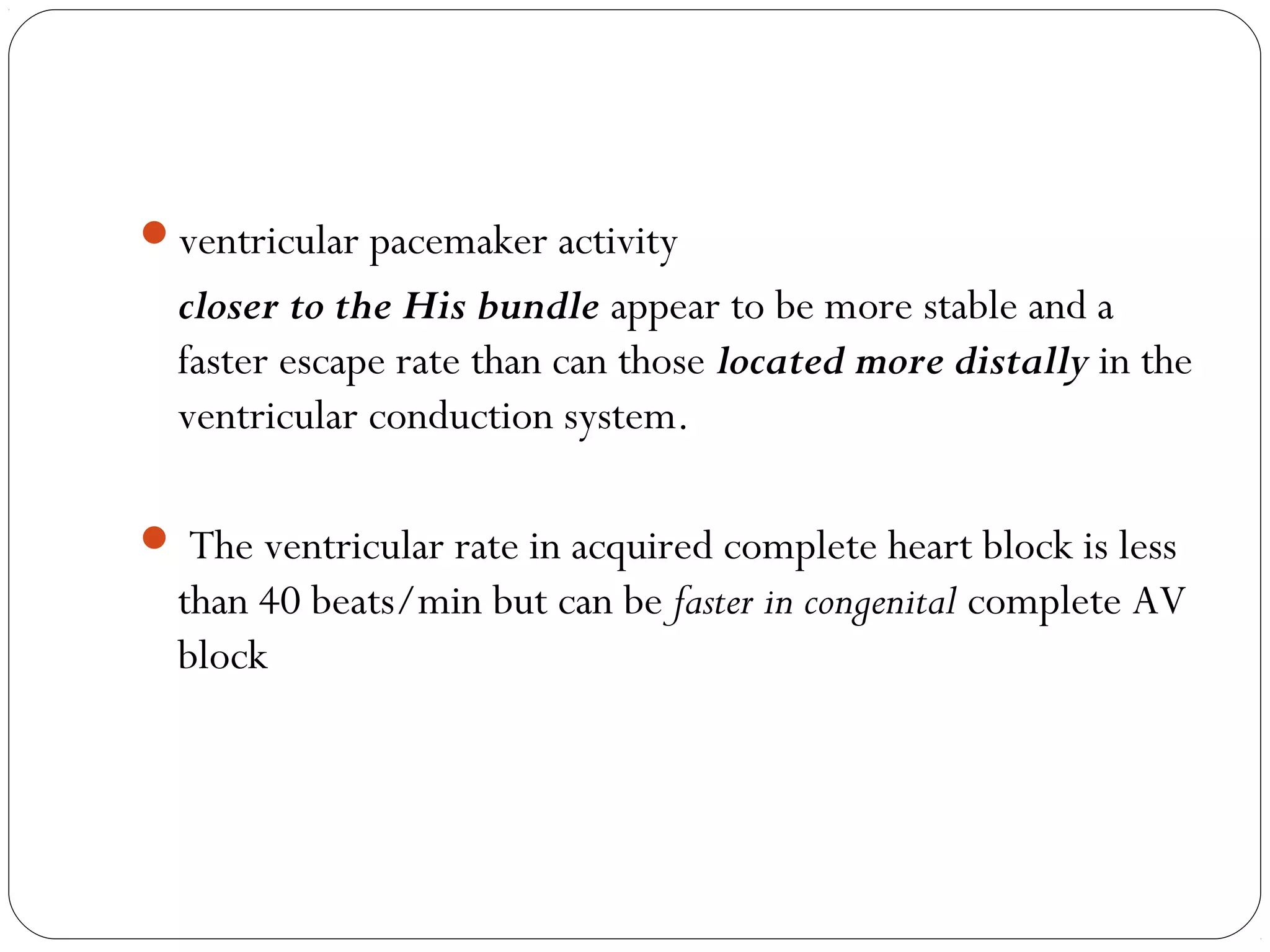
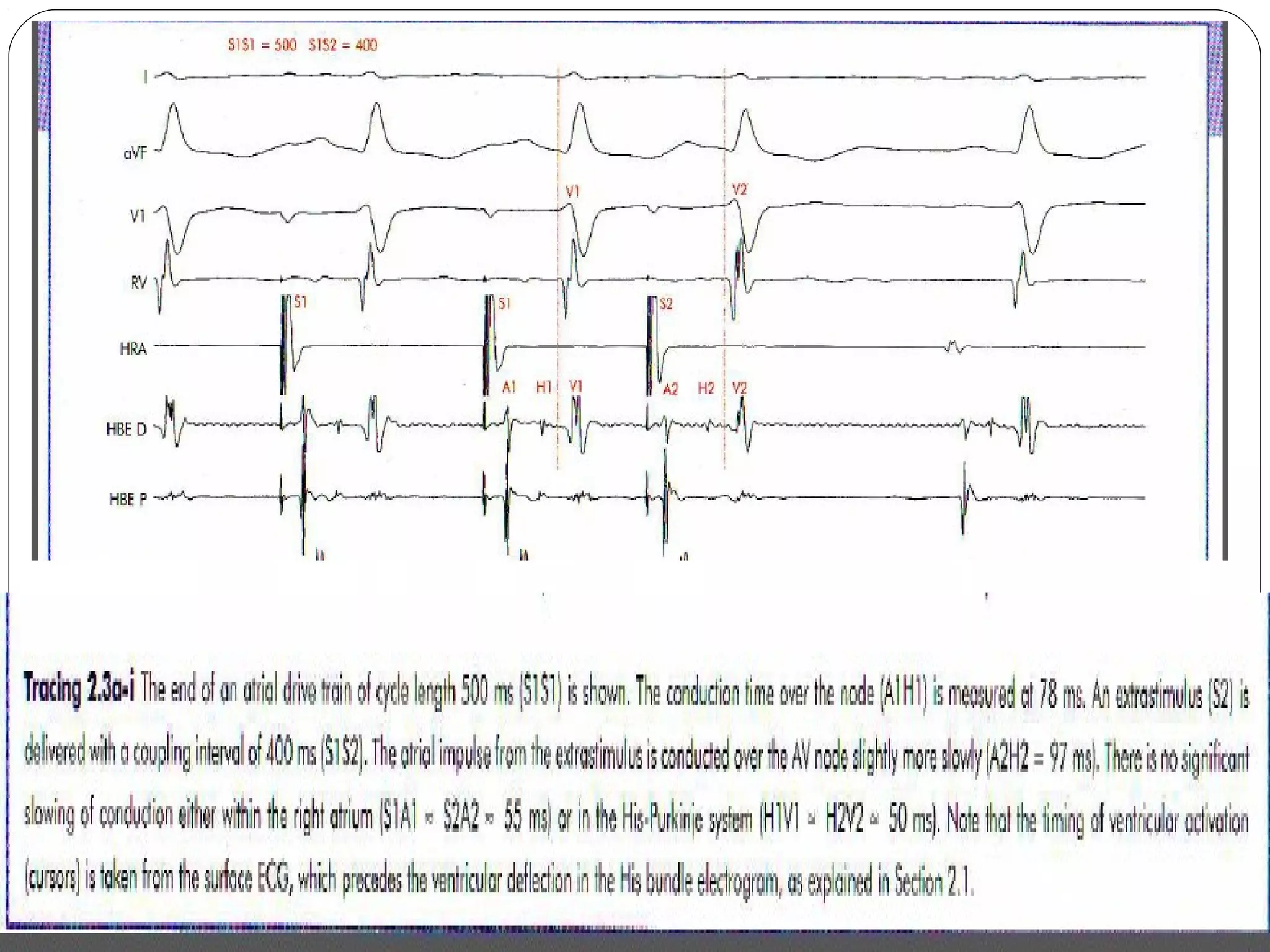
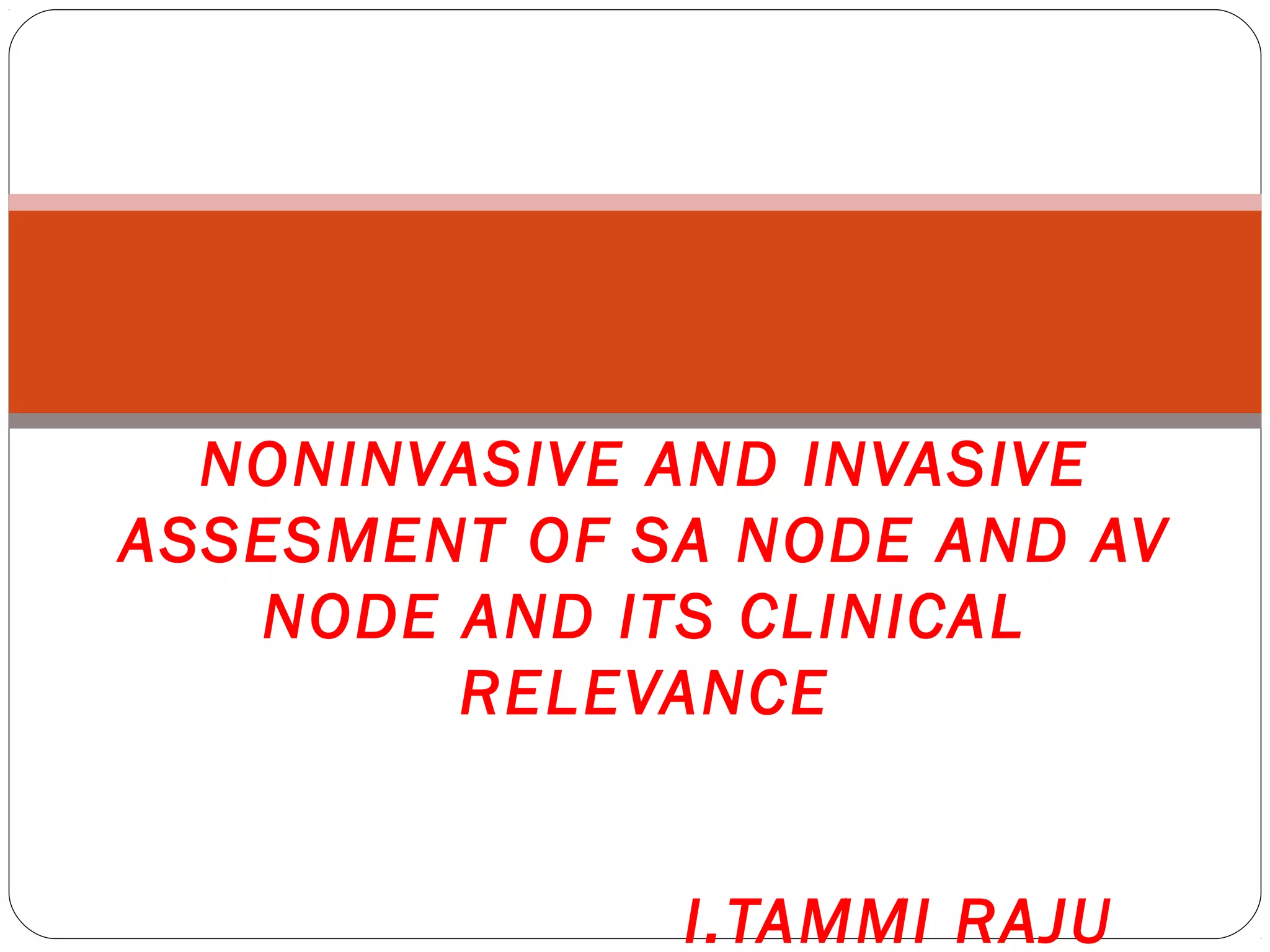
![SACT
The A1-A1 interval
Time required to generate a sinus impulse., conduction time
does not contribute to A1-A1.
A2-A3 (Because A2 resets the SN, the return cycle length) =
generation of the next sinus beat (reflecting SNautomaticity)
+
conduction of the impulse into and out of SN tissue.
(A2-A3) –(A1-A1) =
Total time it takes to enter and exit the SN tissue.
This number represents twice the SACT
SACT = [(A2-A3) – (A1-A1)] / 2
Normal SACT times generally range from 40 to 150 milliseconds](https://image.slidesharecdn.com/assessmentofsanodeandavnode-dr-150621174919-lva1-app6891/75/Assessment-of-sa-node-and-av-node-dr-i-tammi-raju-56-2048.jpg)