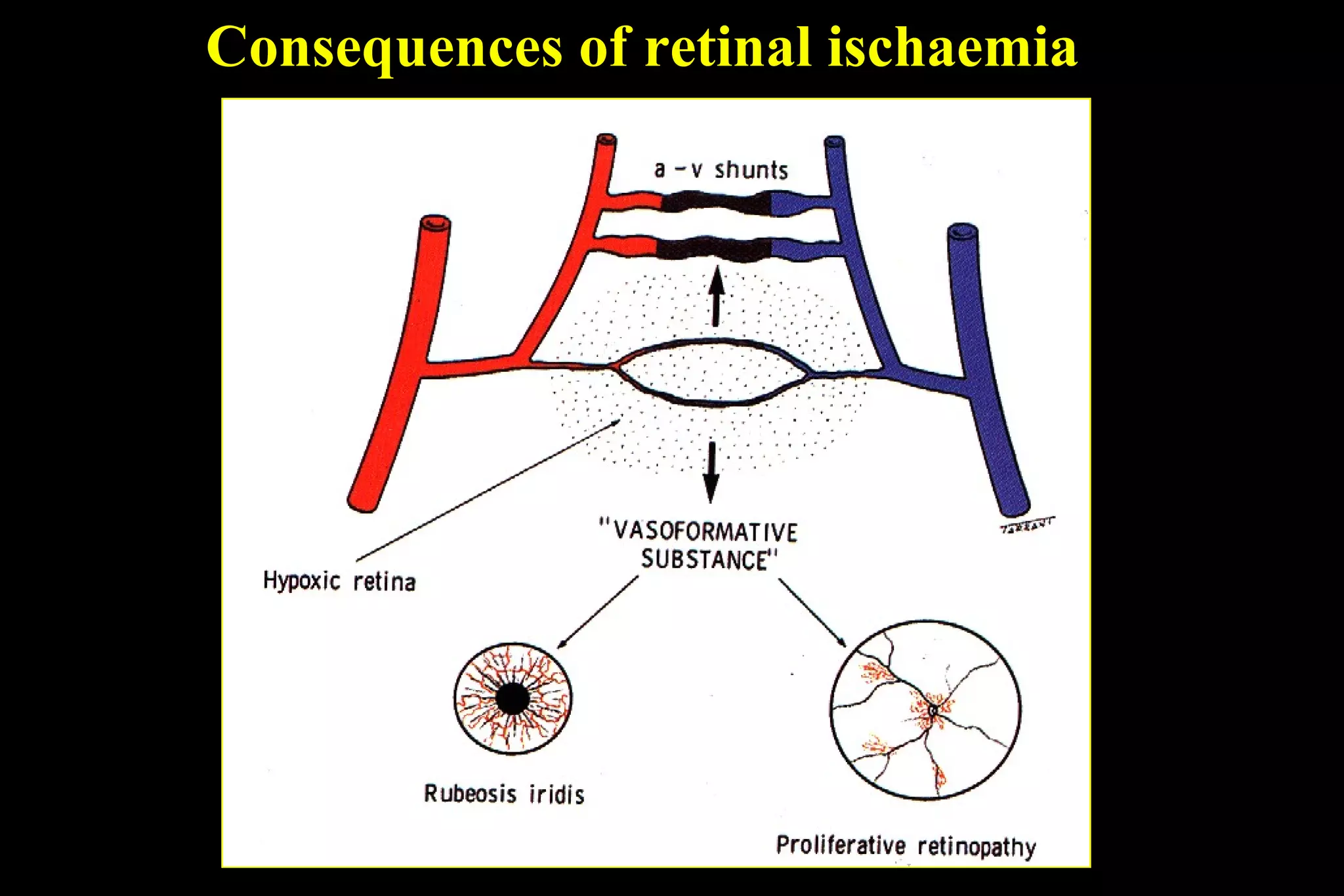
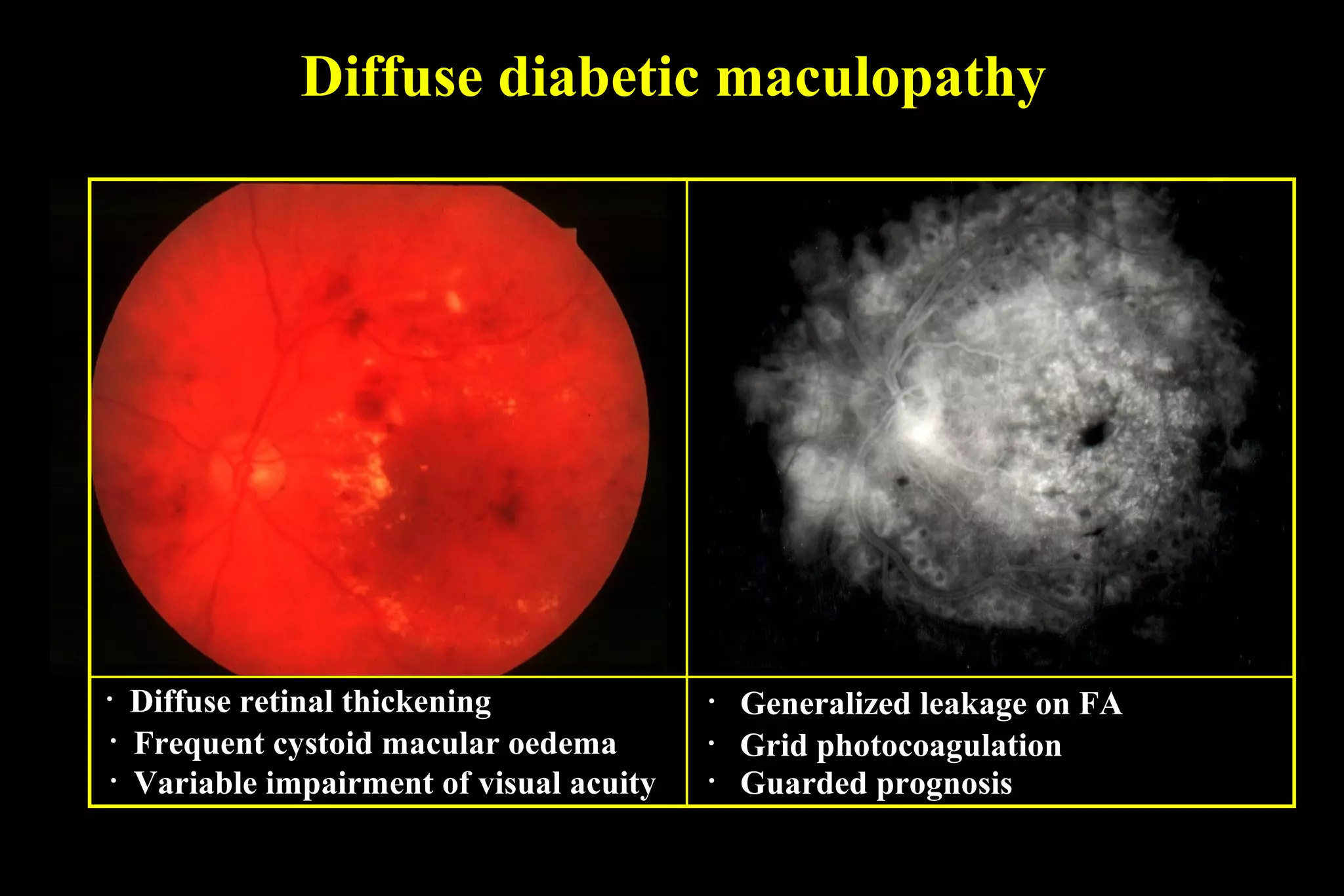
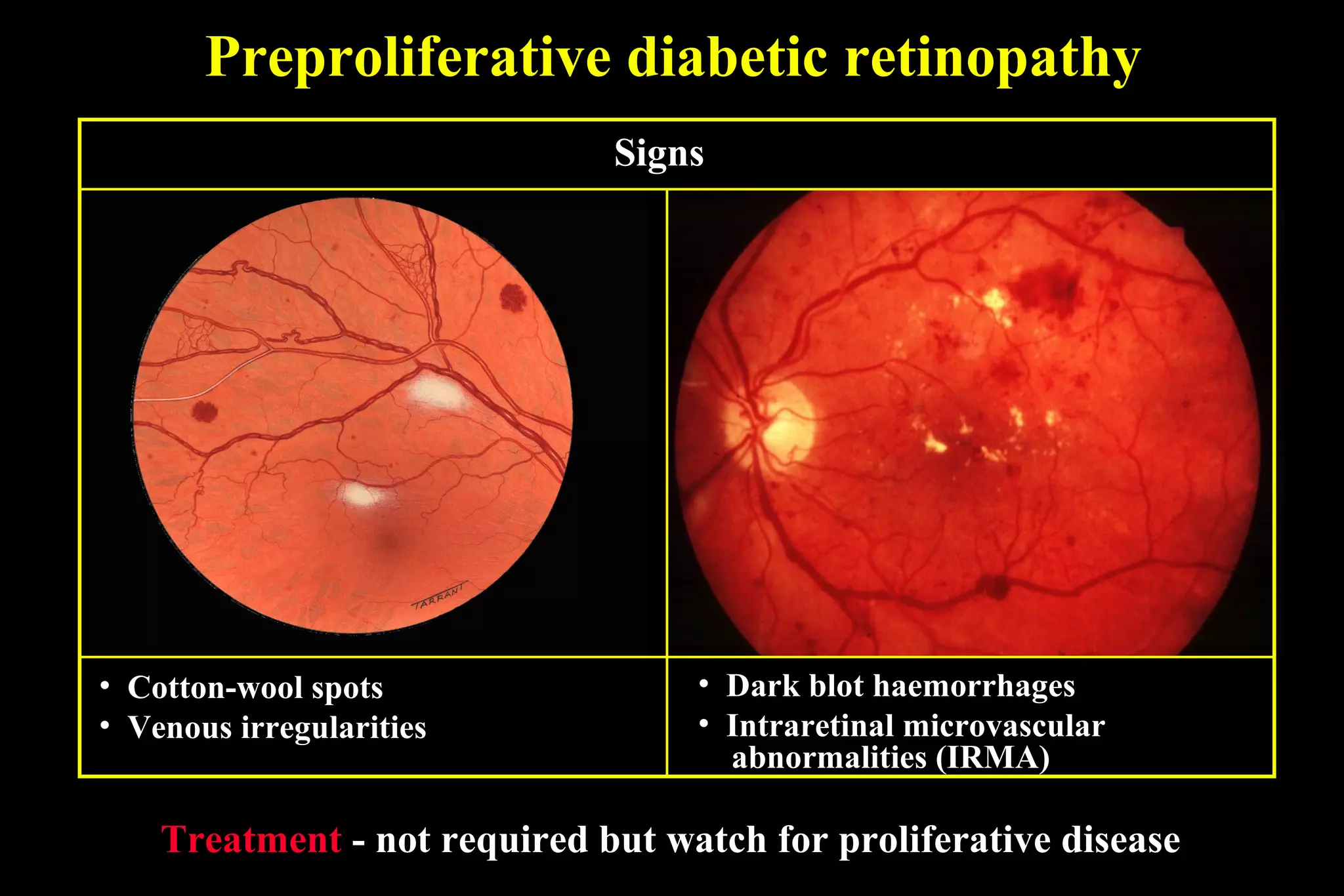
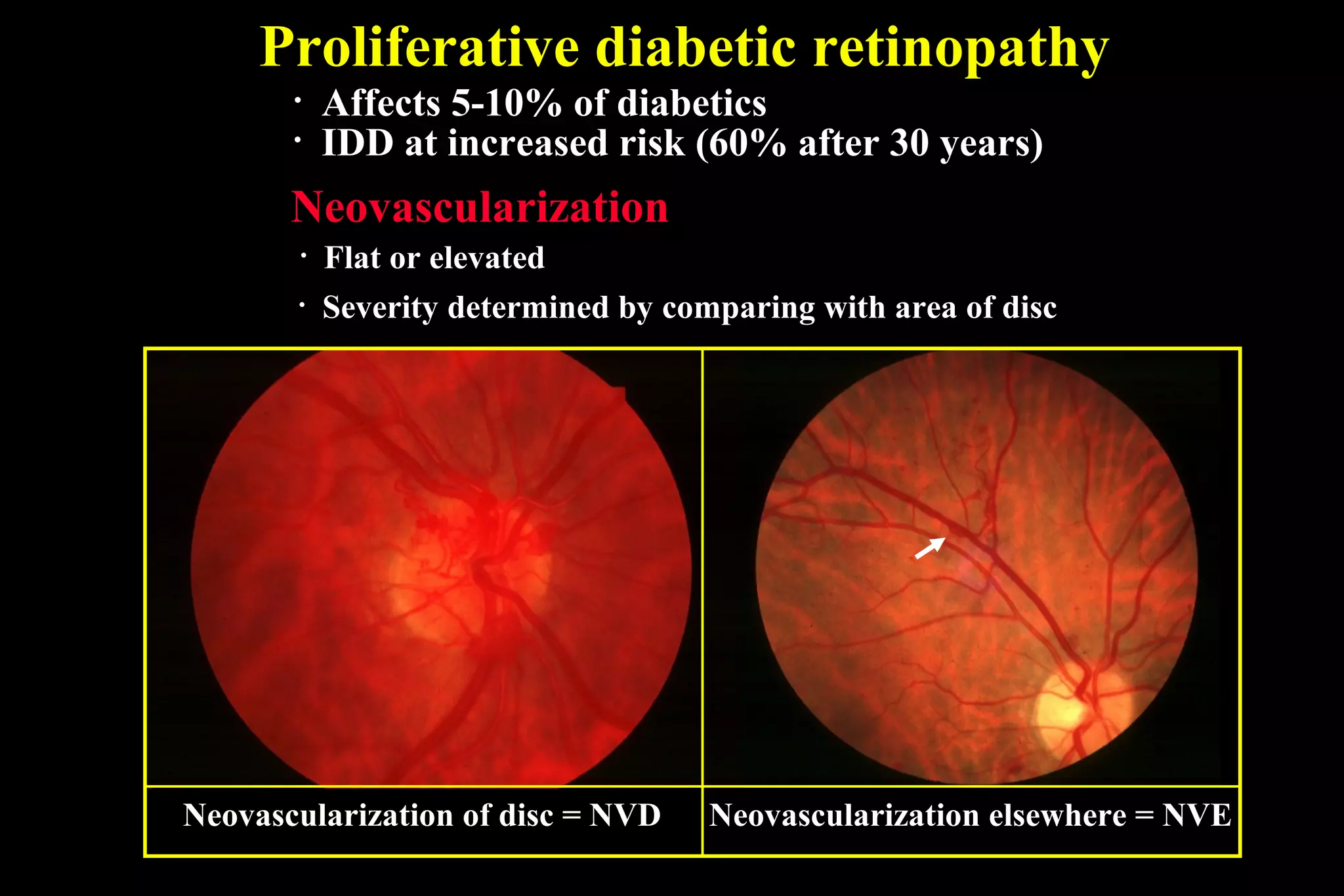
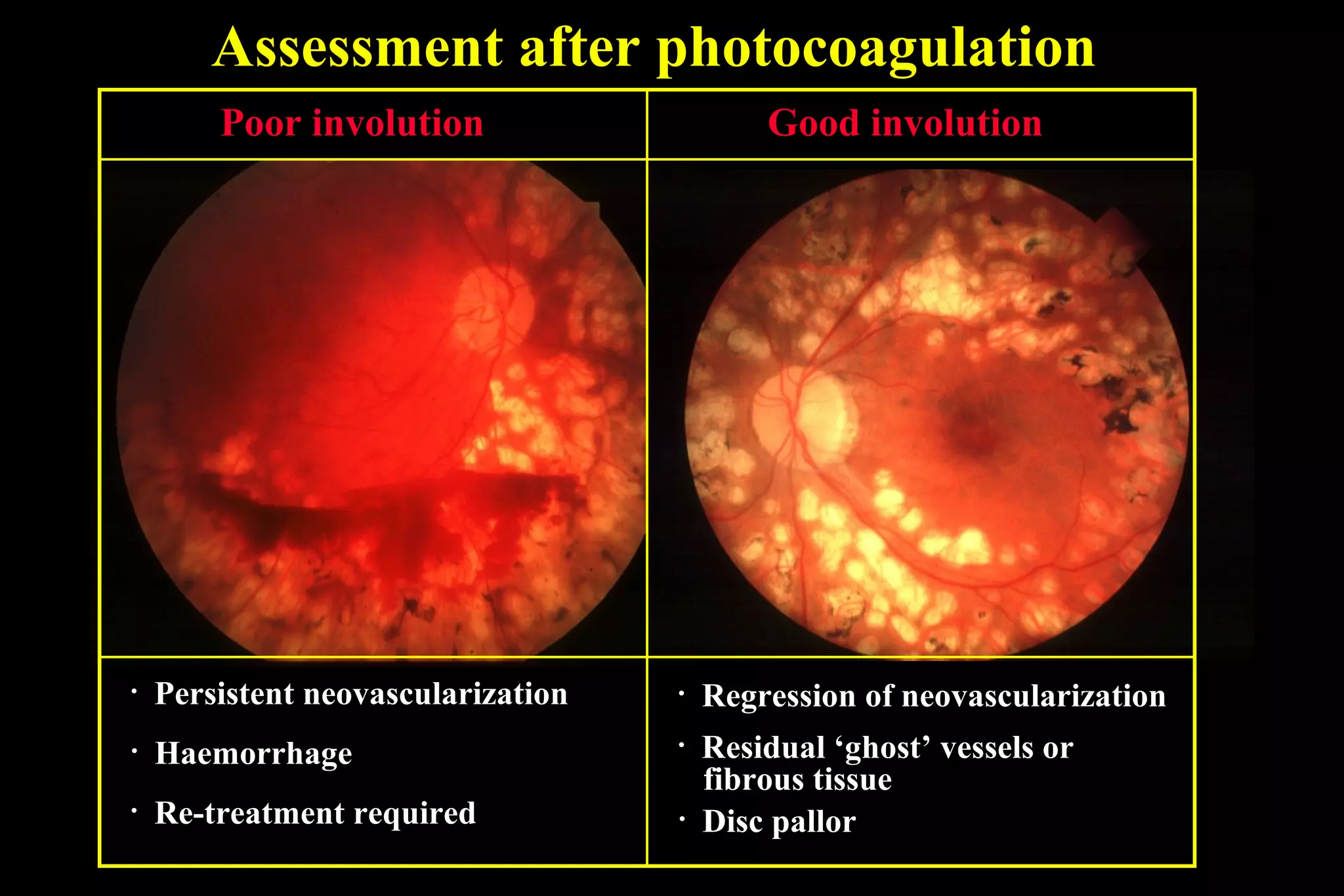
This document discusses diabetic retinopathy, beginning with risk factors like long diabetes duration and poor control. It describes the progression from early background changes to preproliferative then proliferative stages. Clinically significant macular edema is defined and treated initially with laser, while proliferative disease requires panretinal photocoagulation or sometimes surgery. The stages, treatments, and goals of managing this complication of diabetes are outlined.