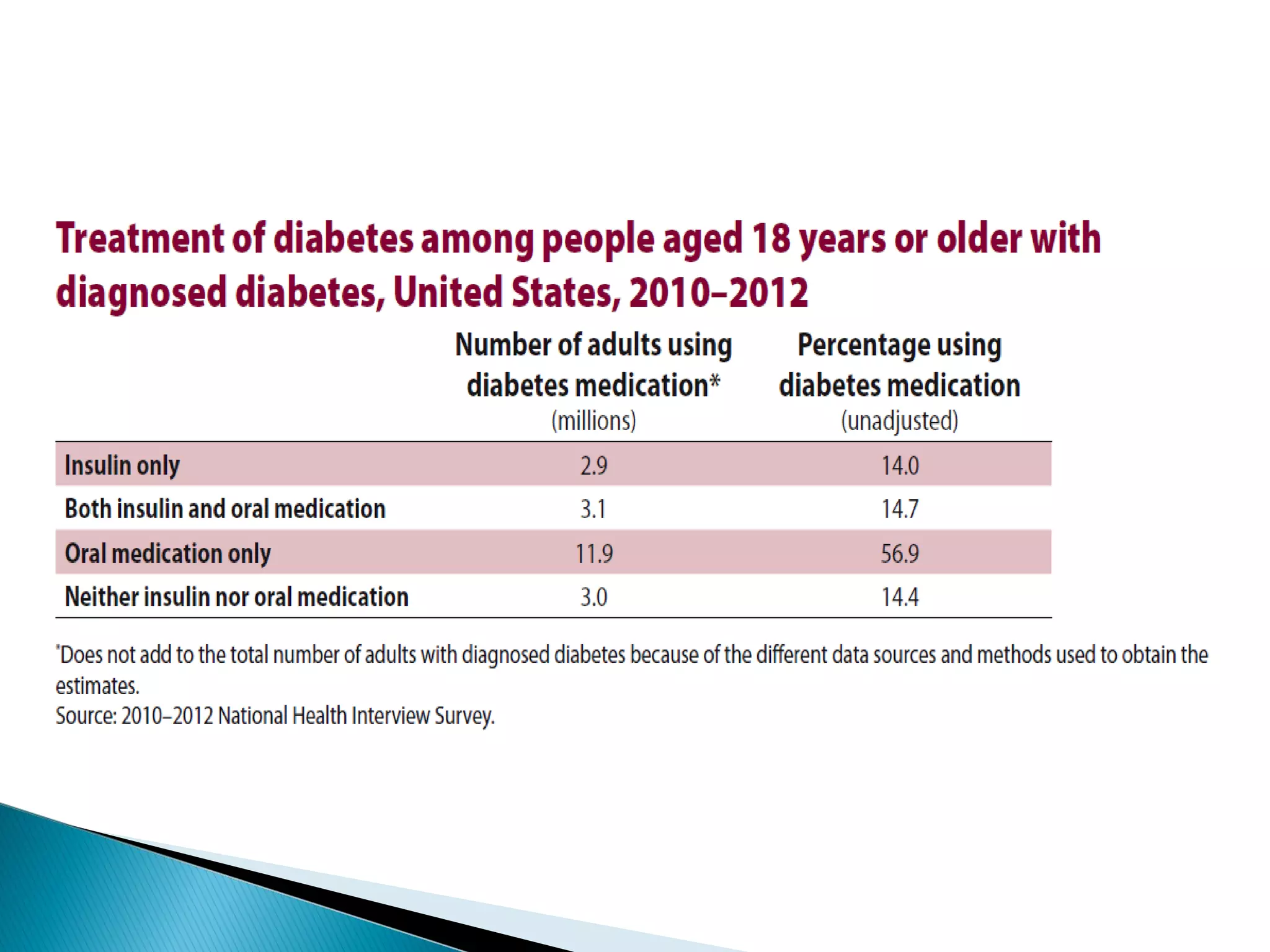
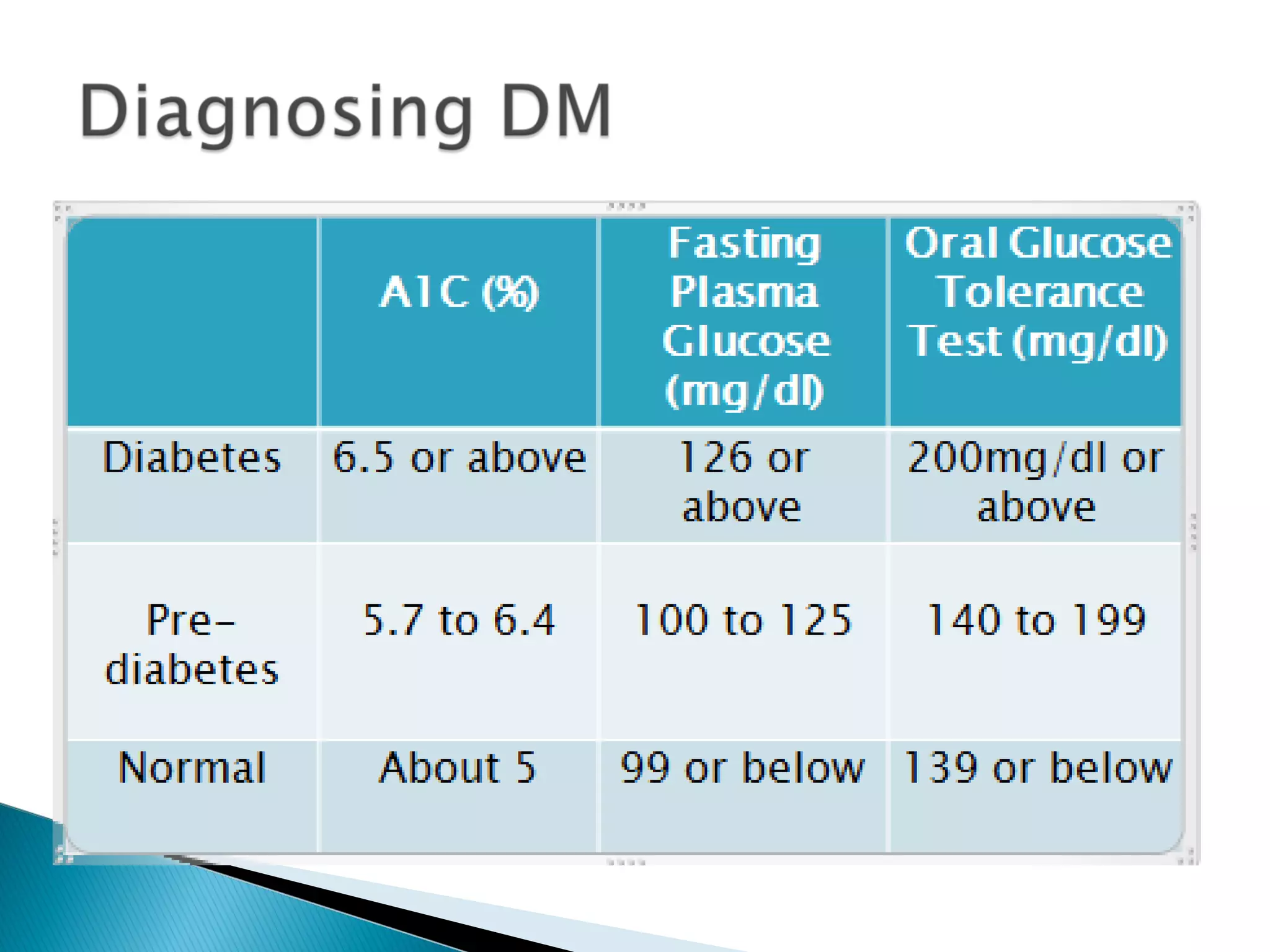
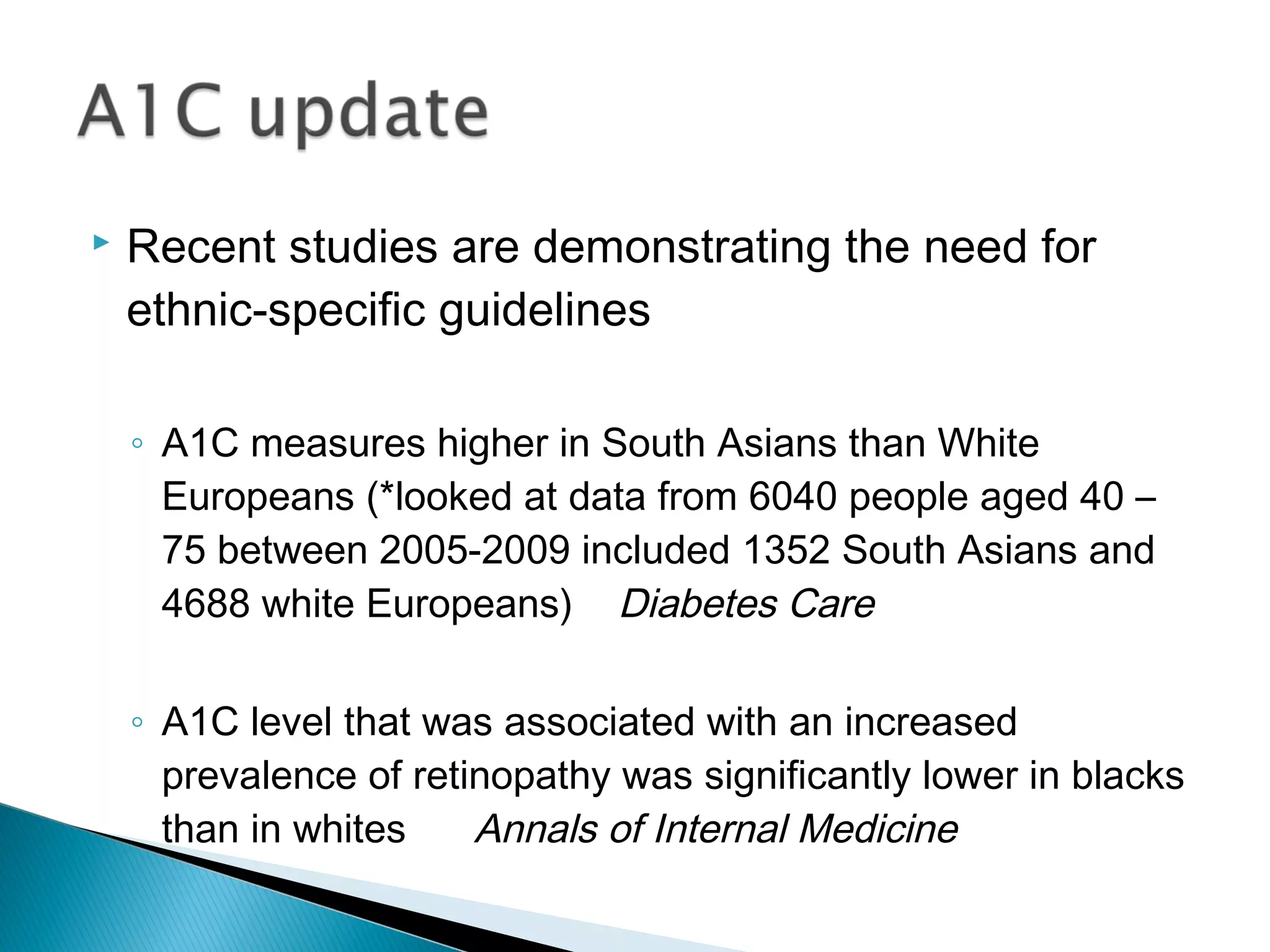
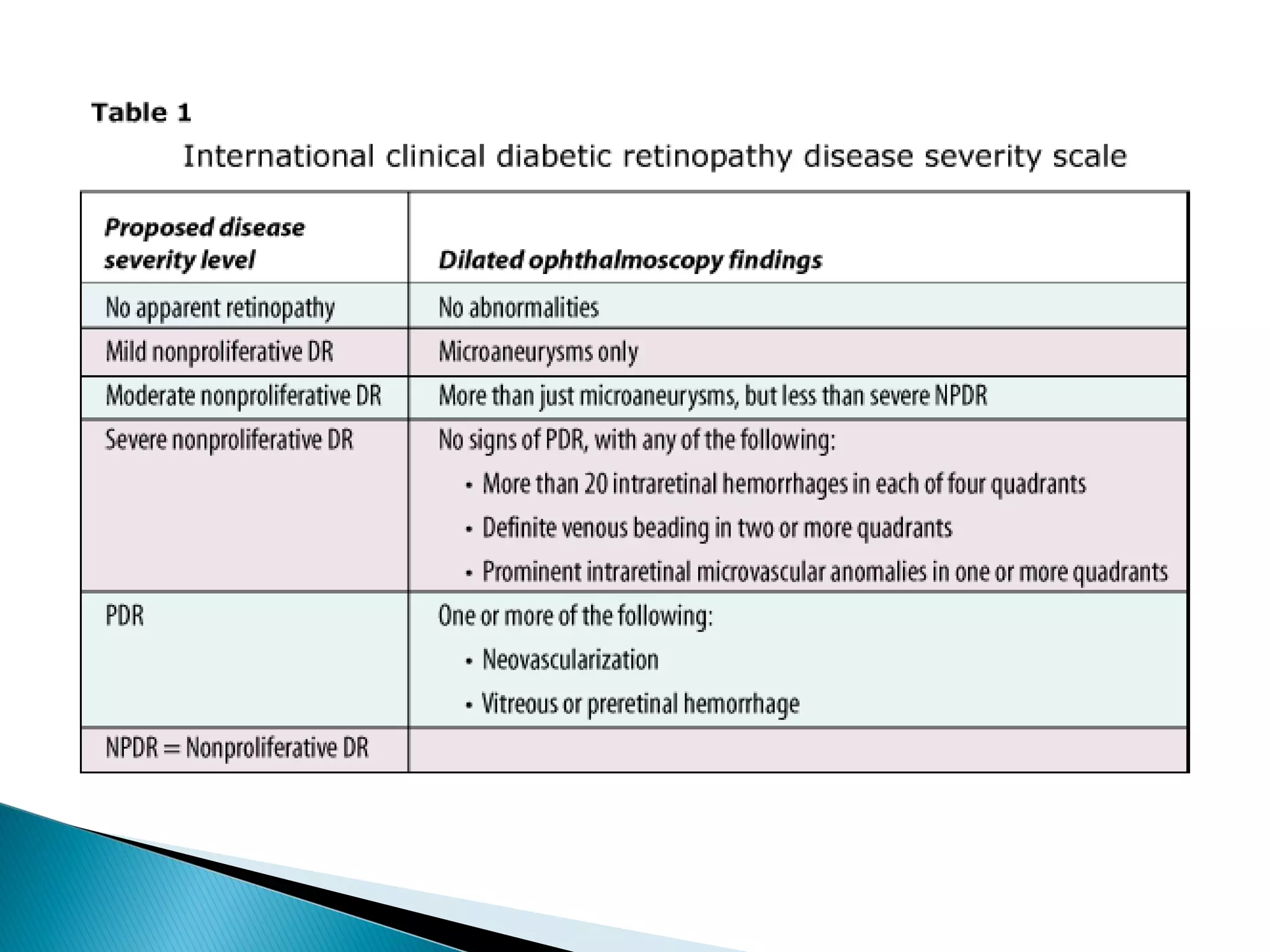
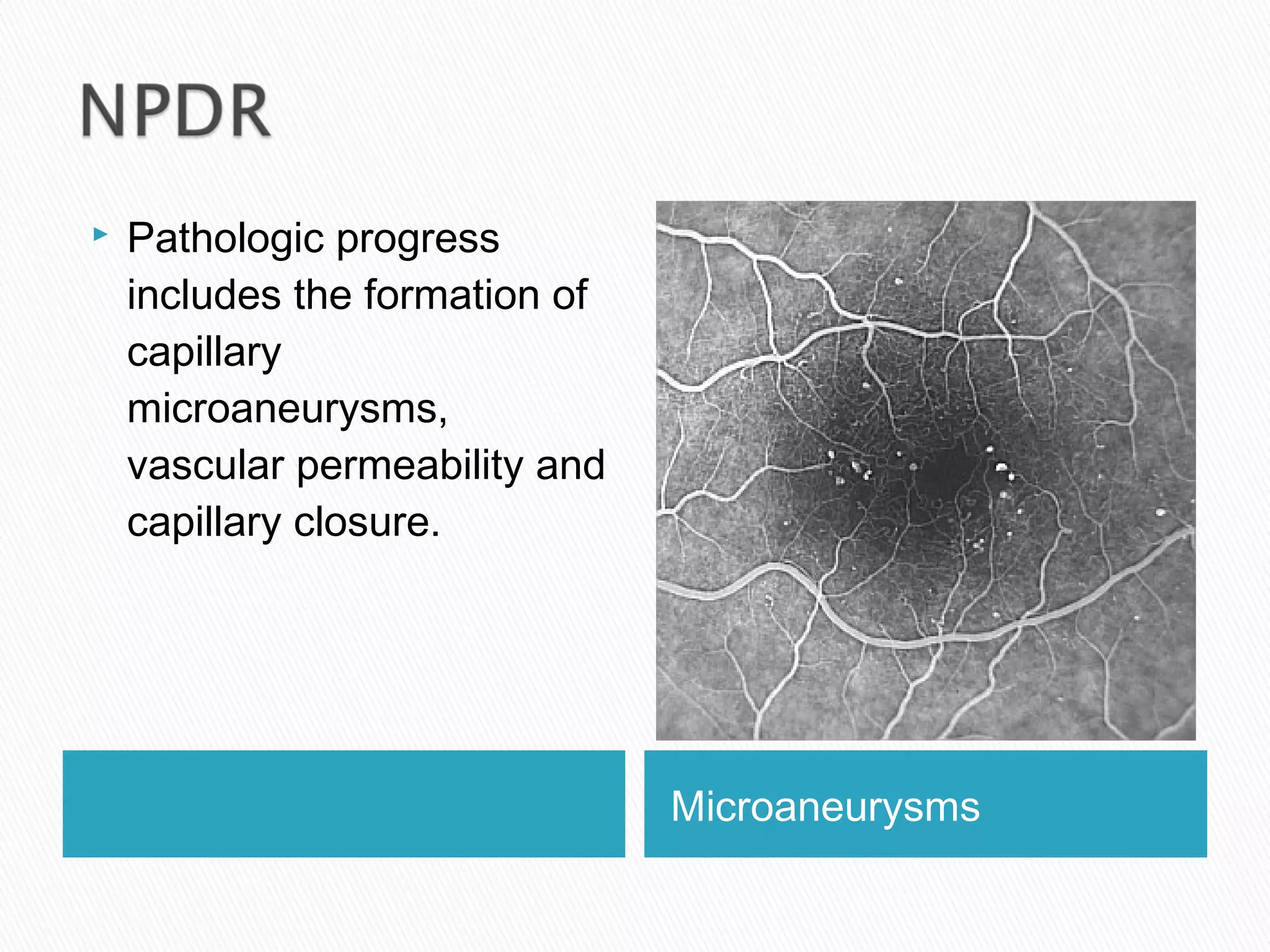
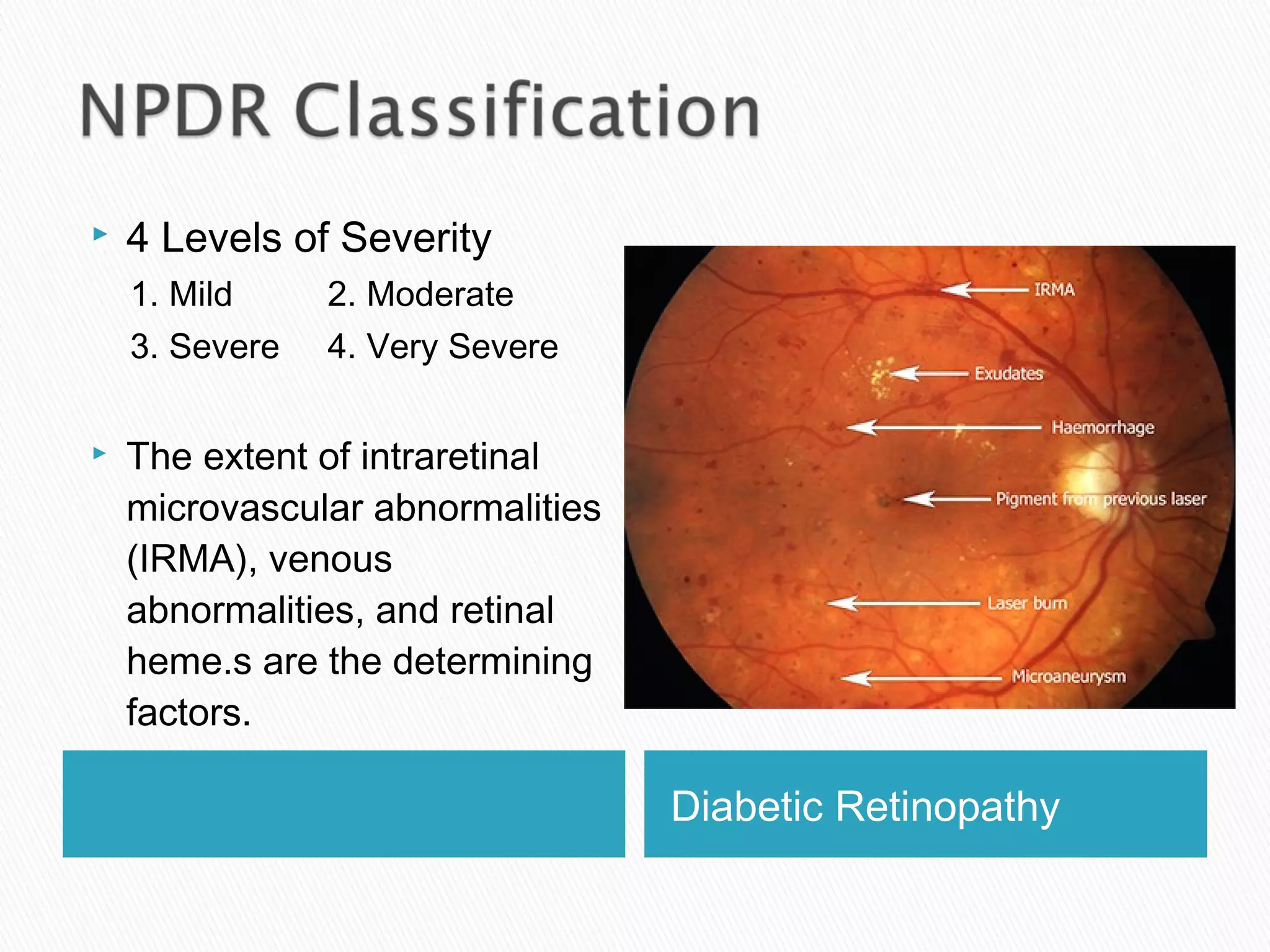
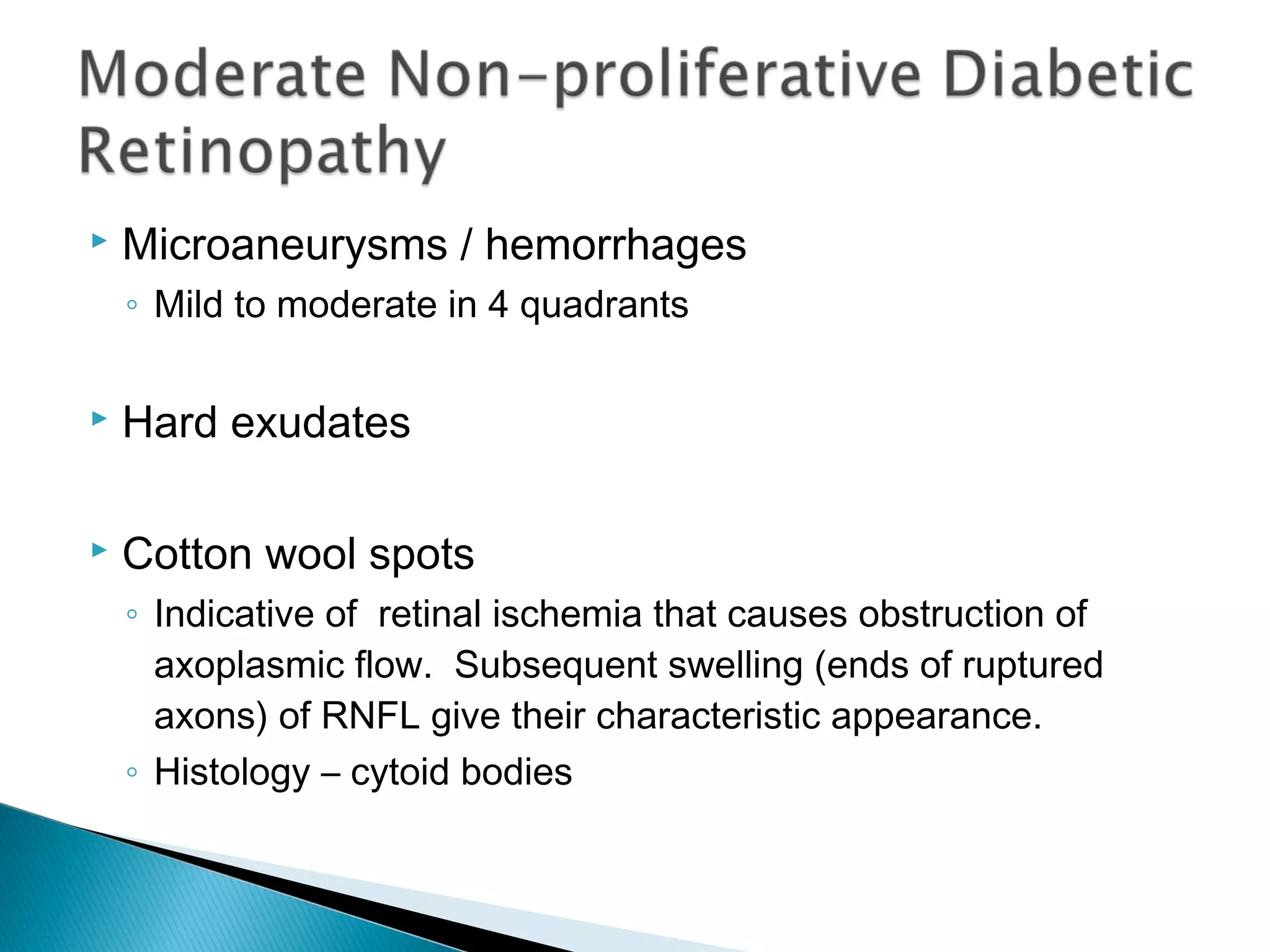
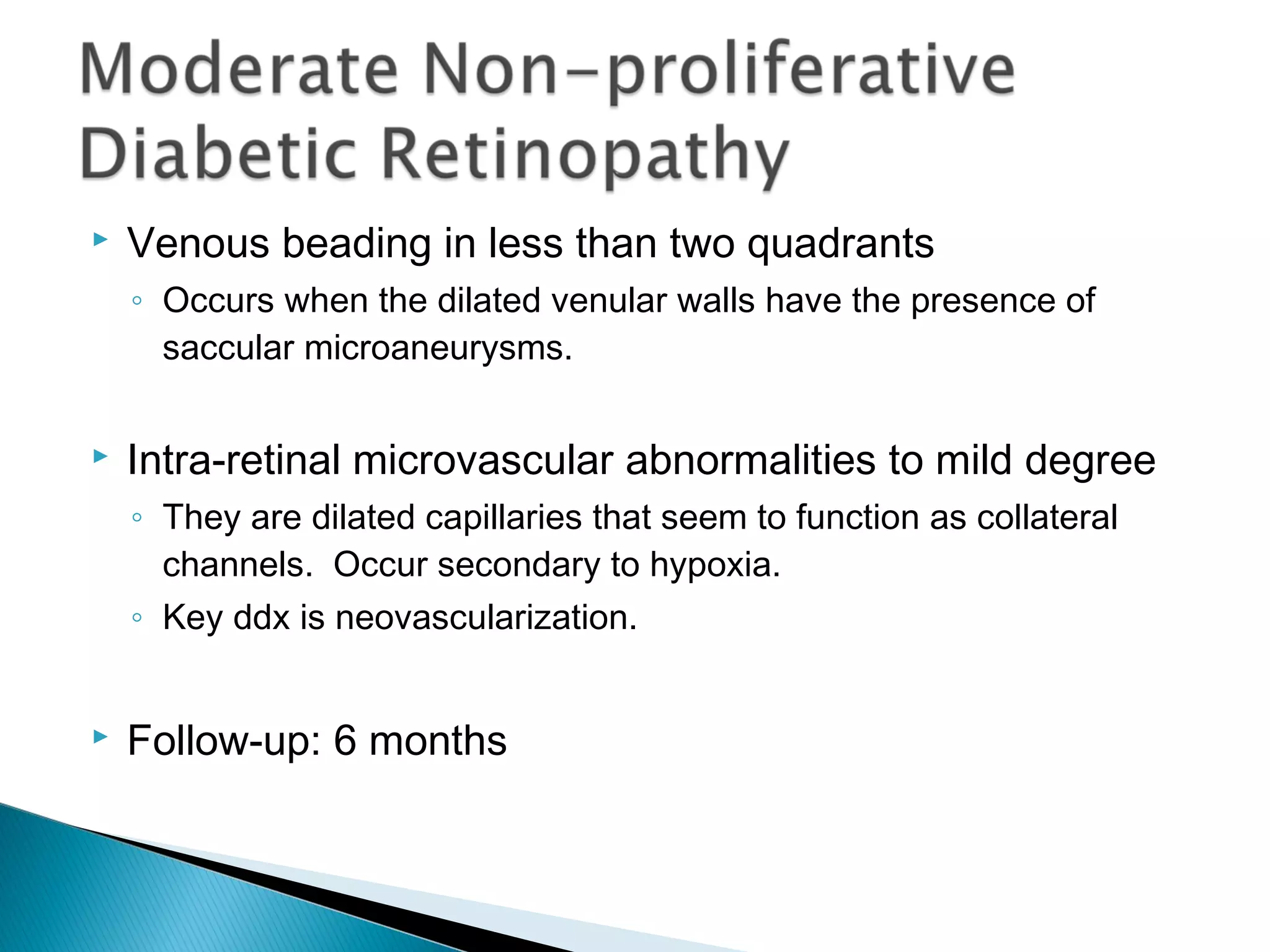
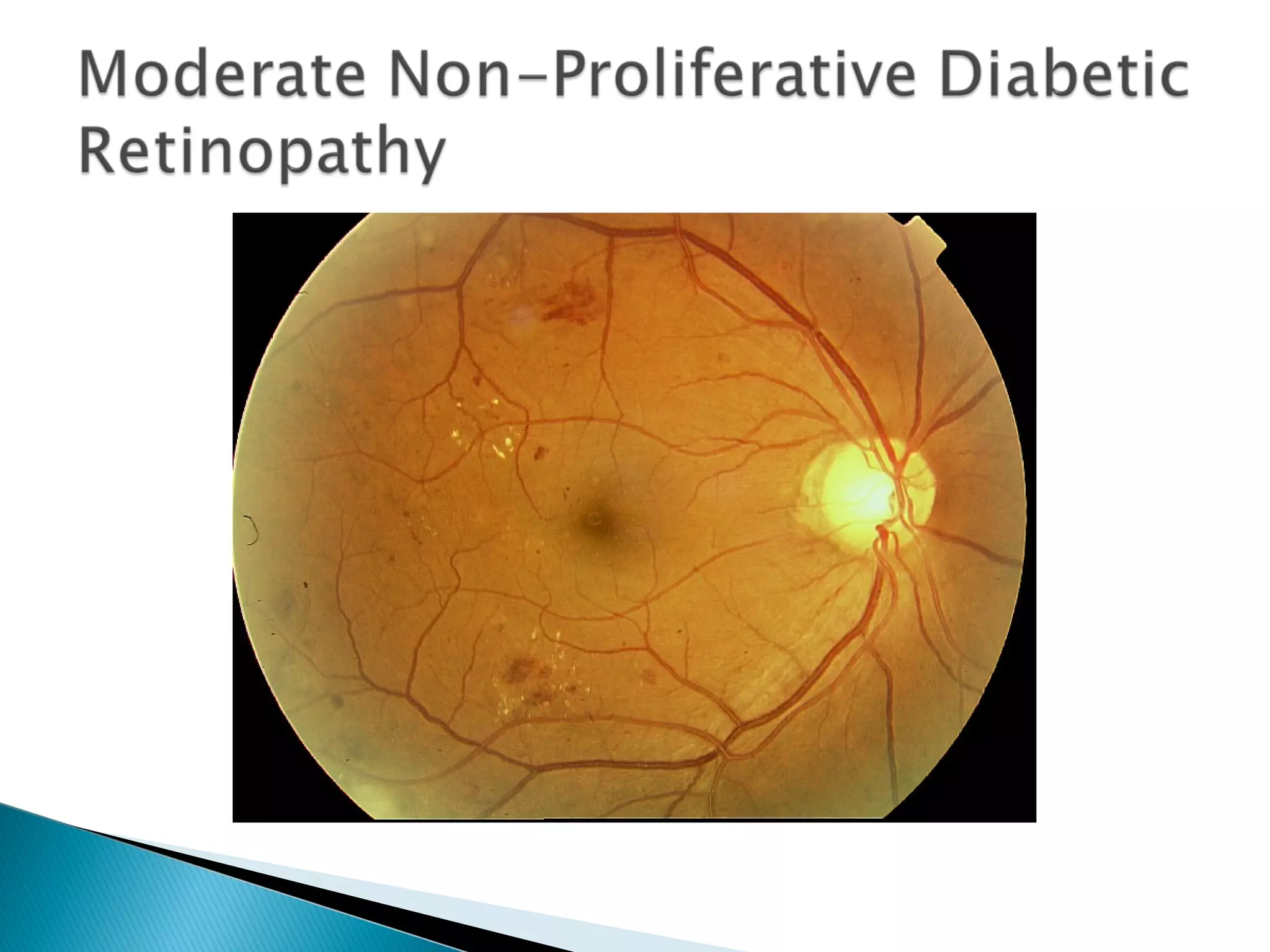
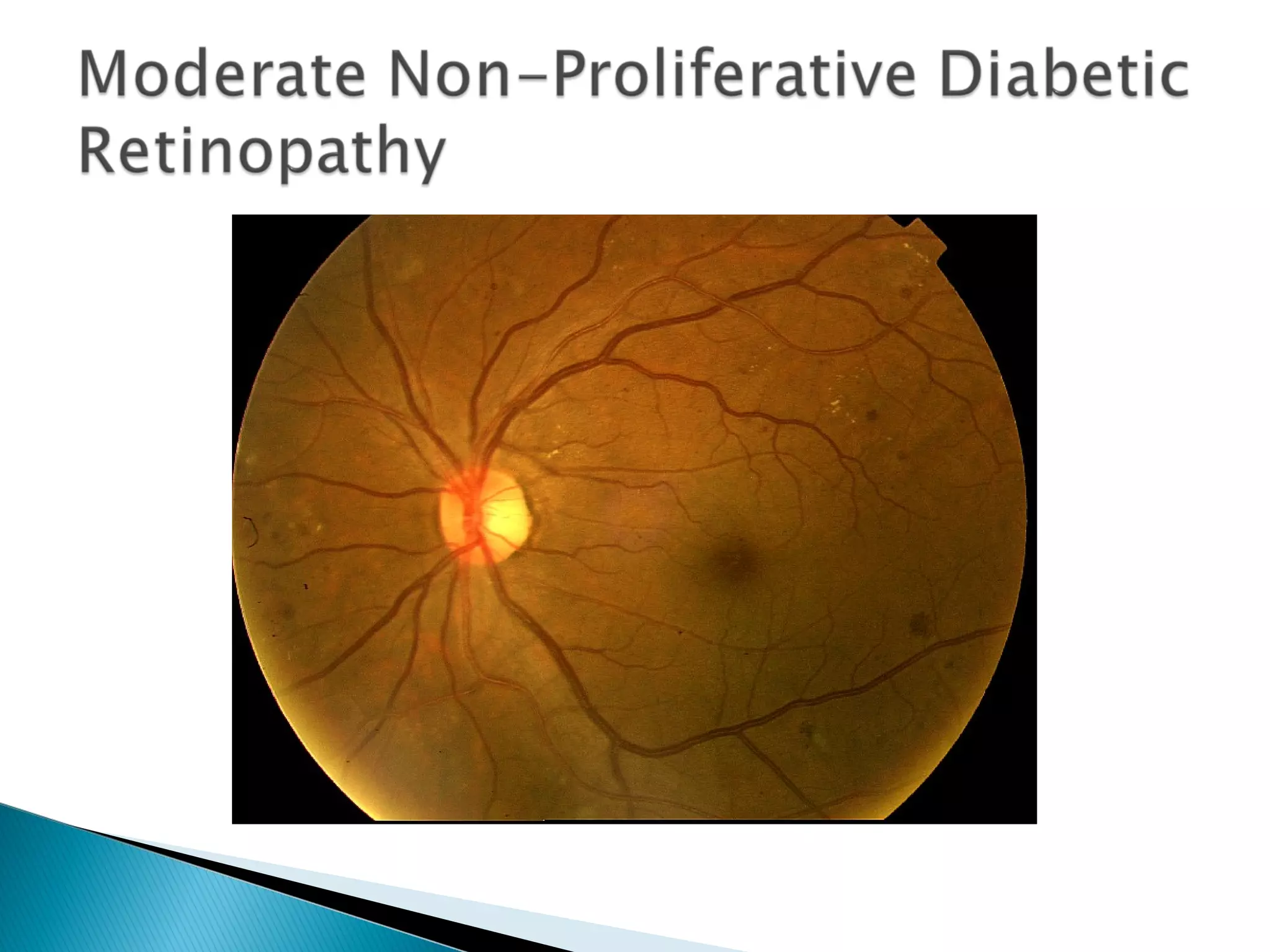
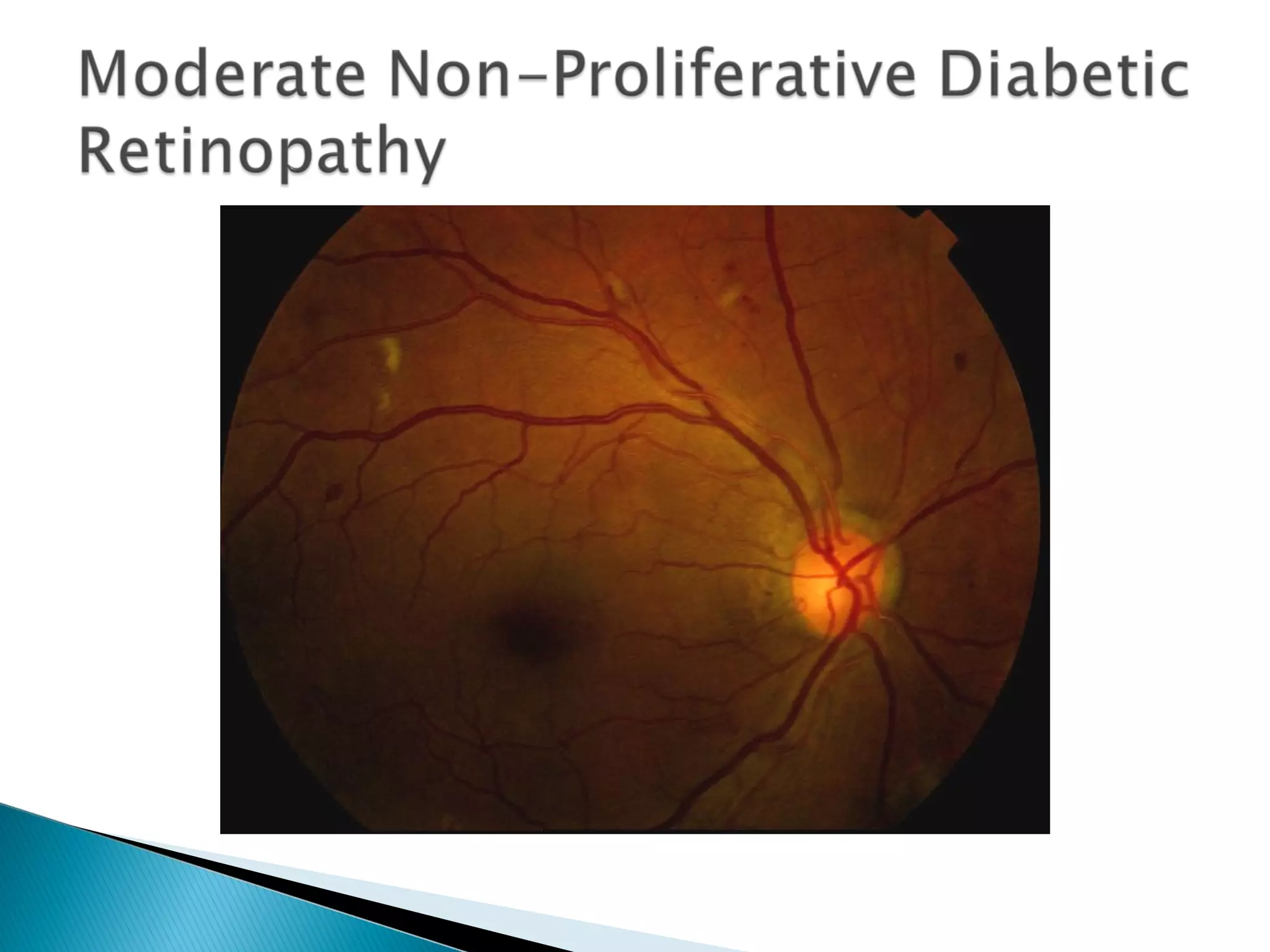
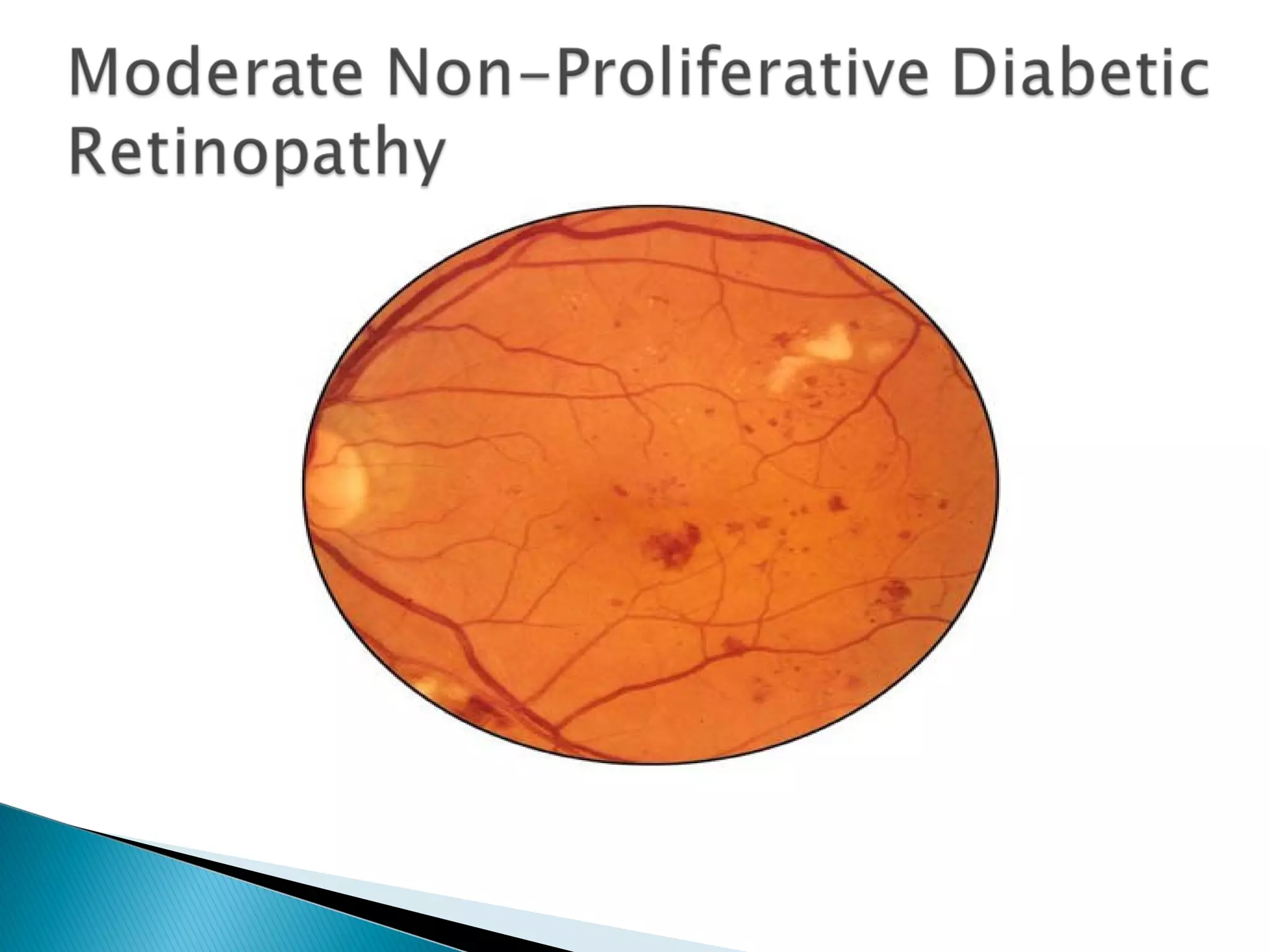
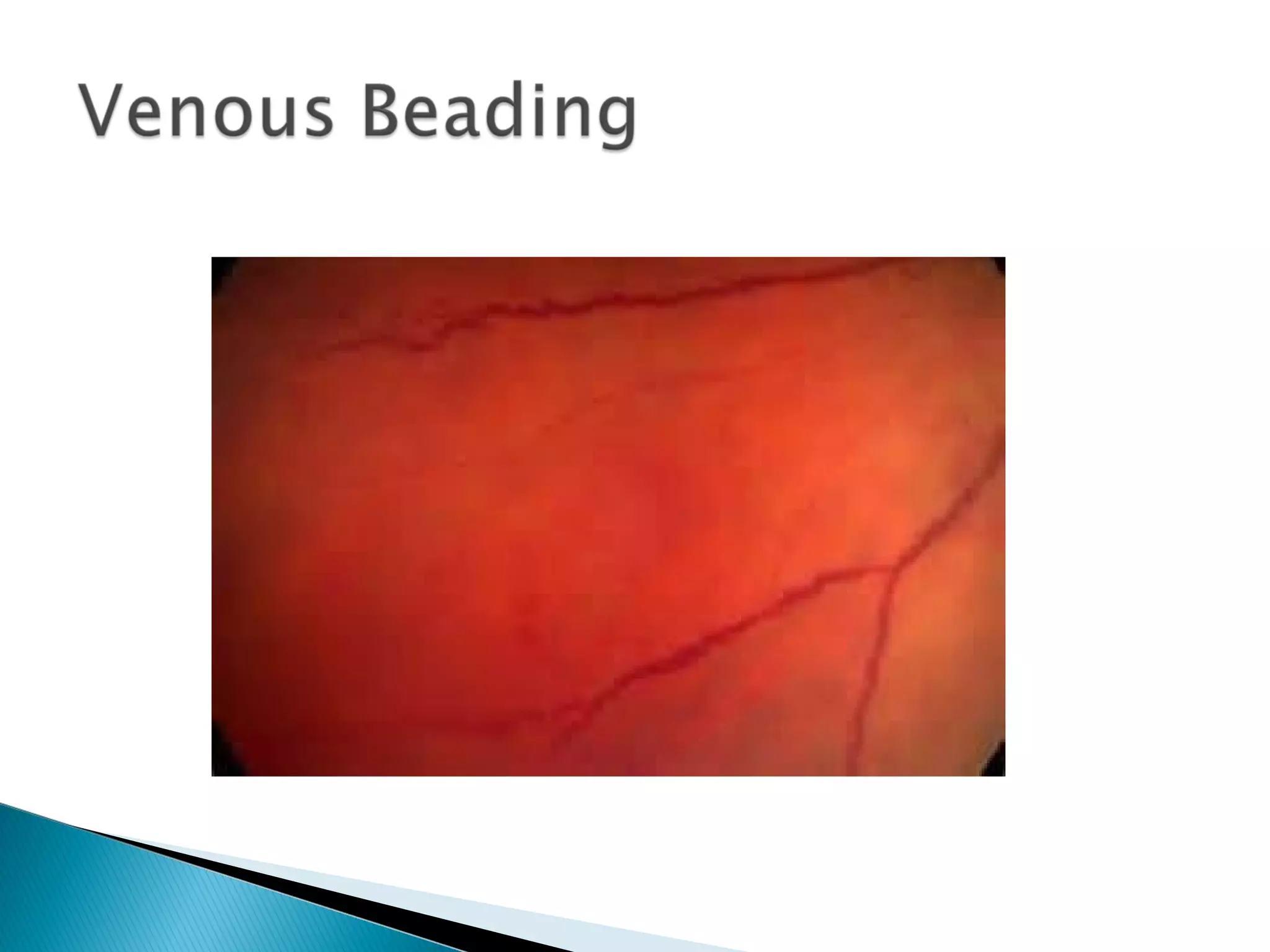
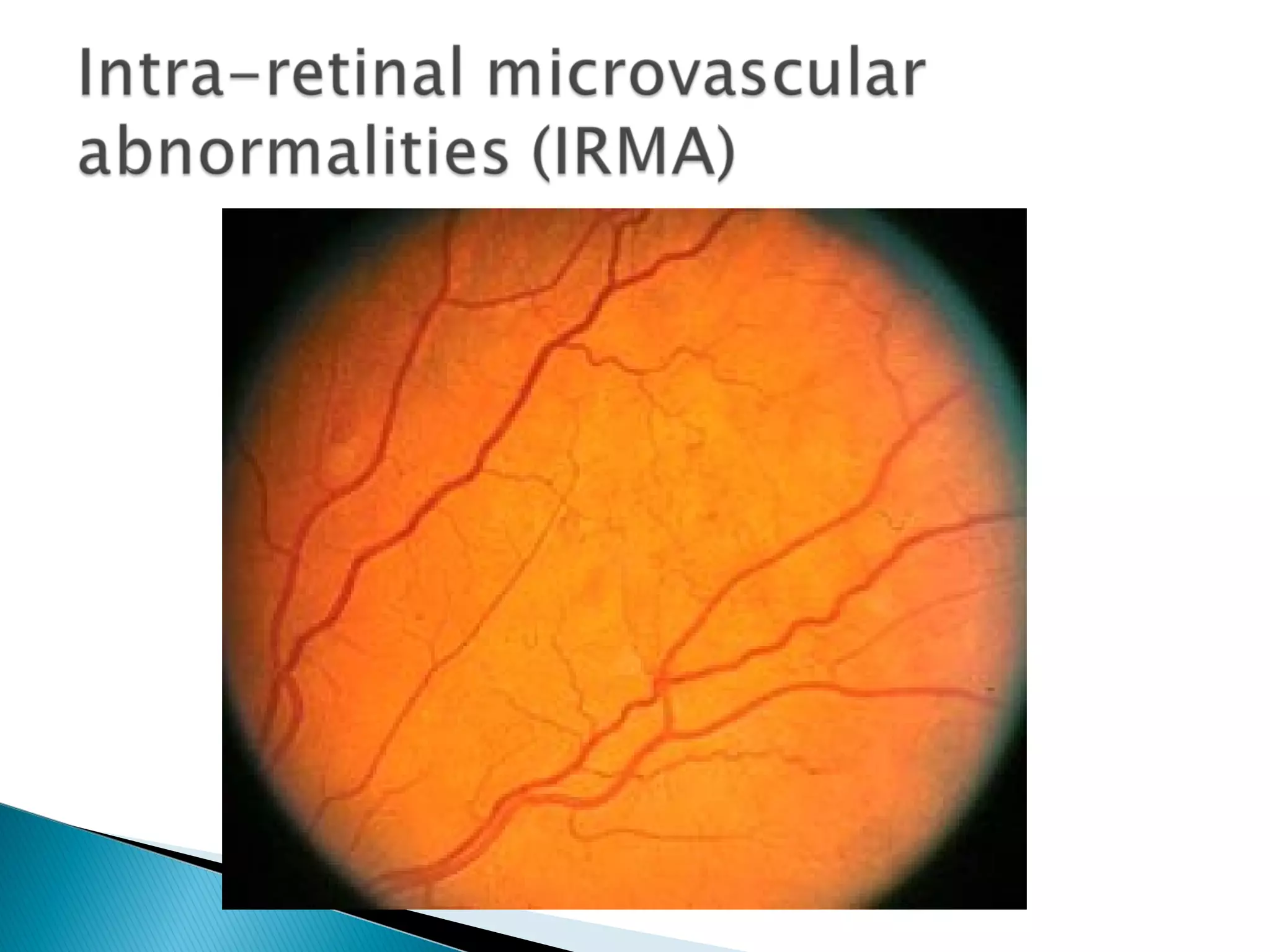
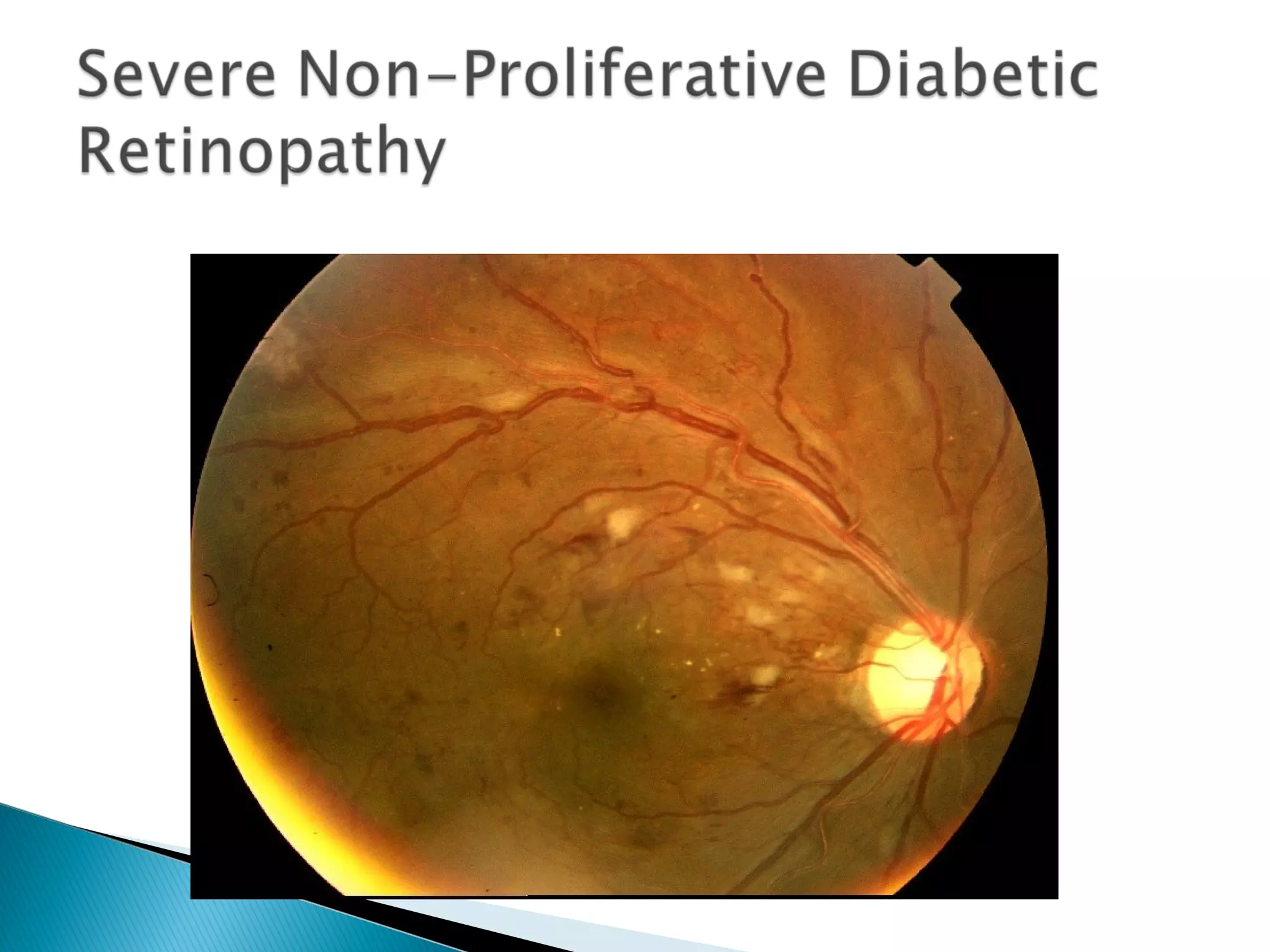
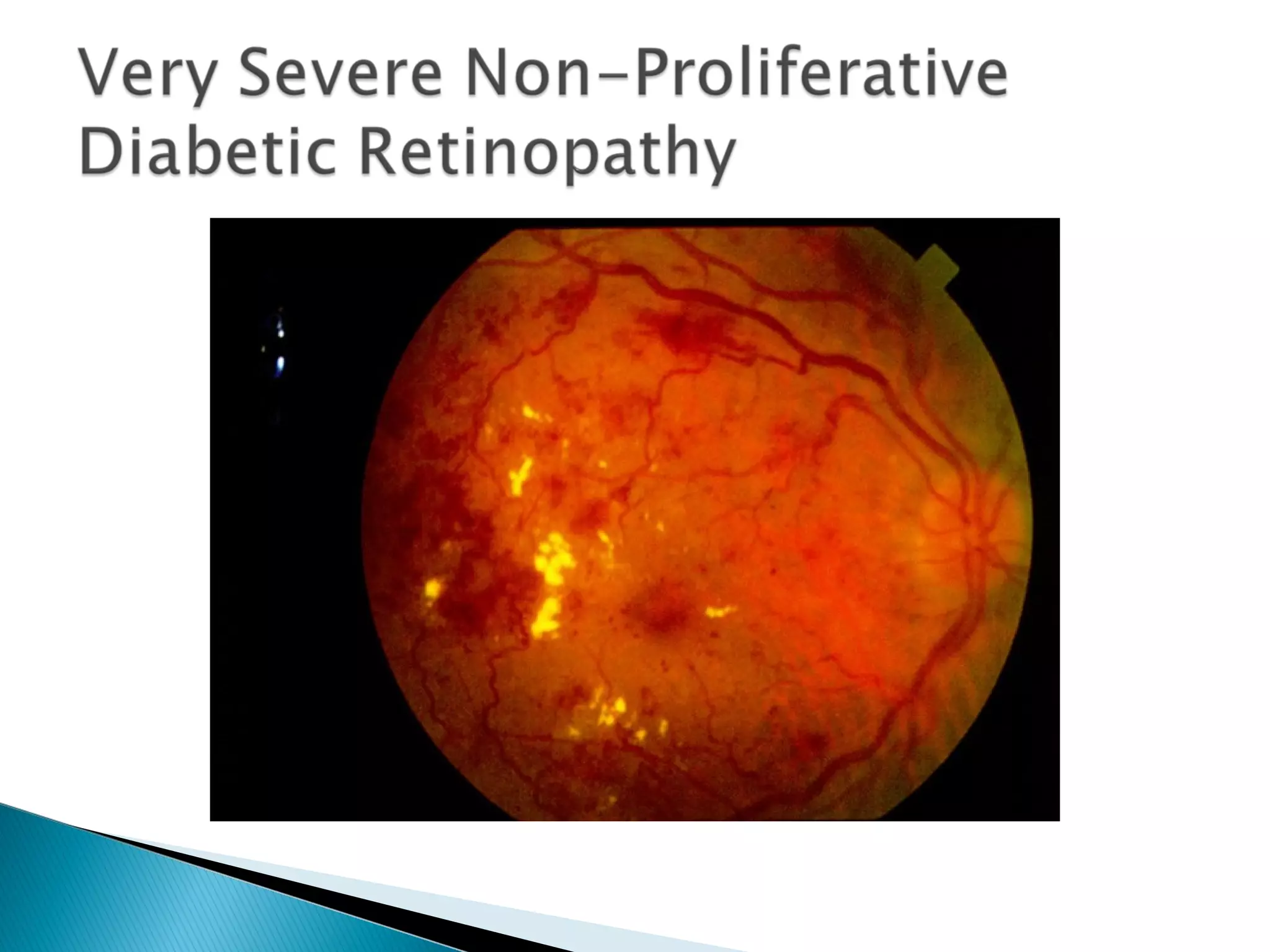
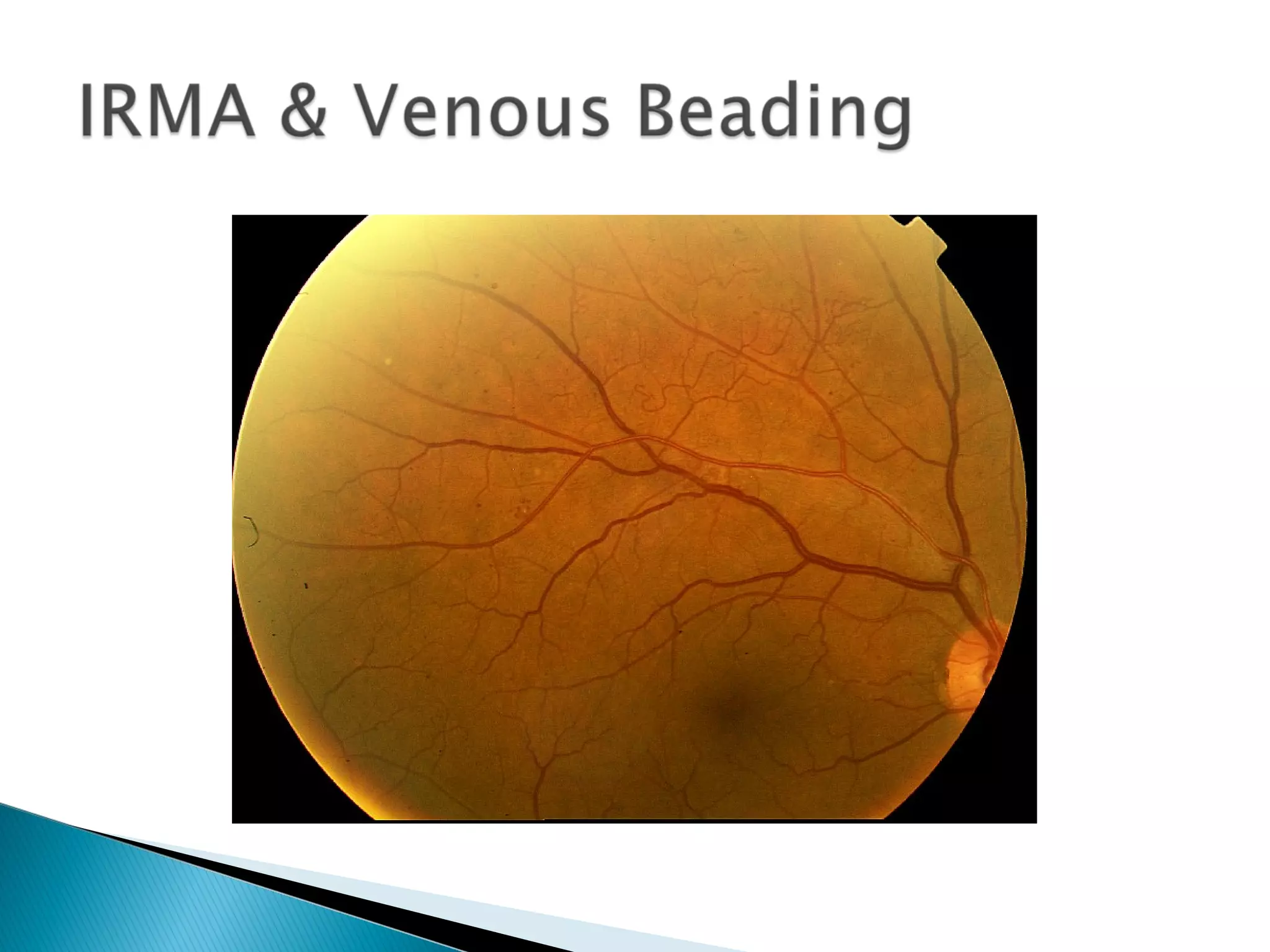
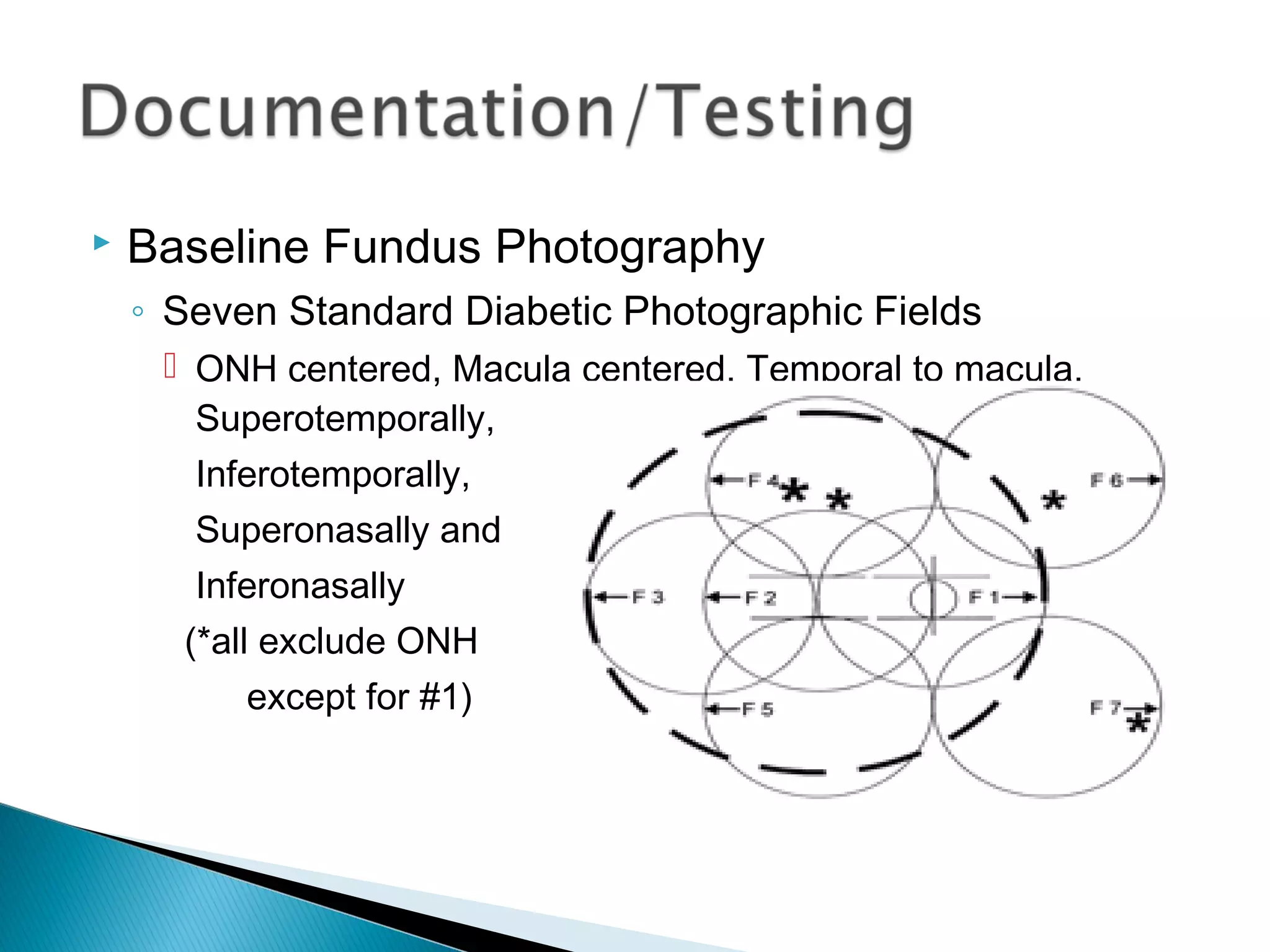
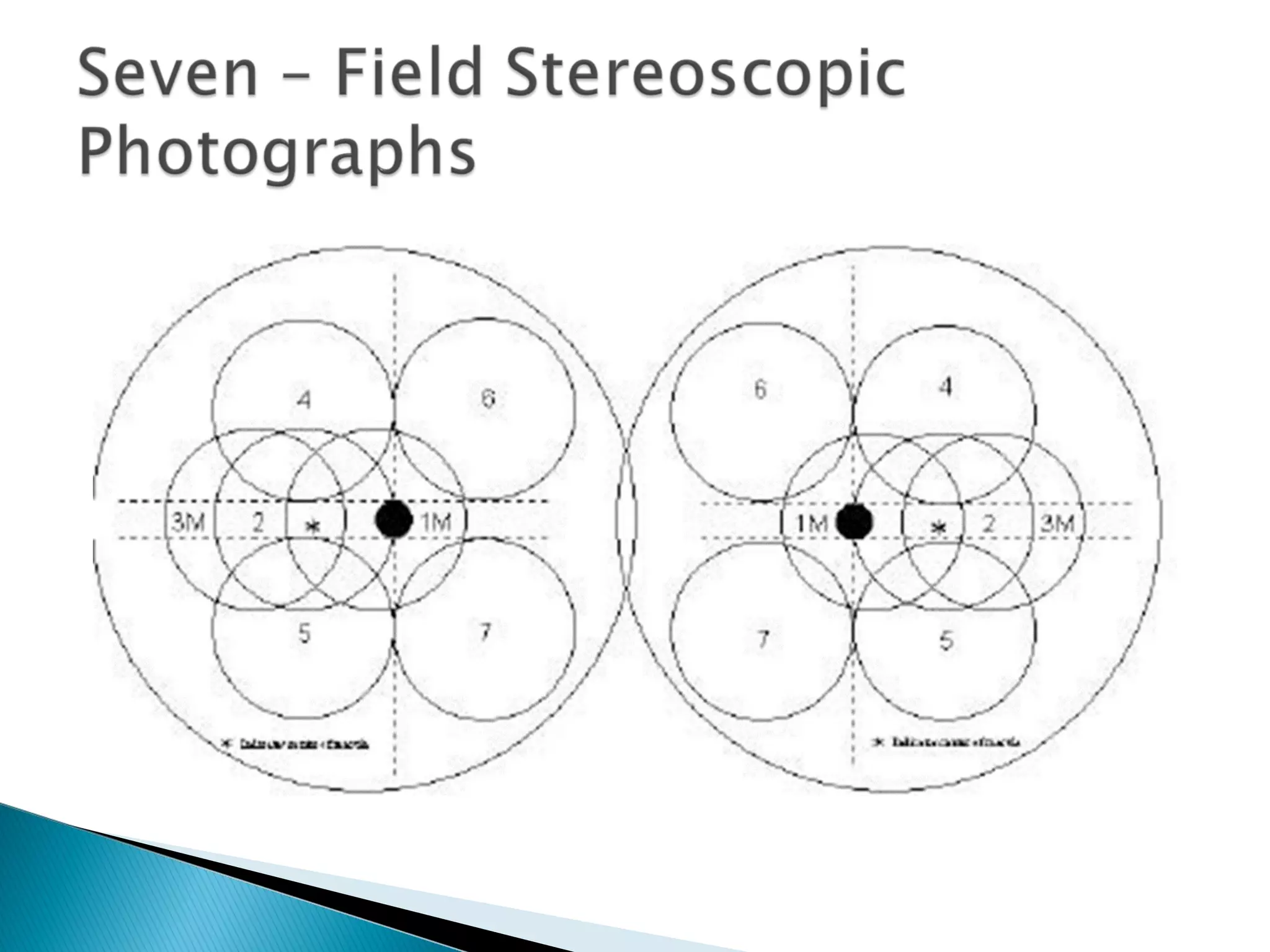
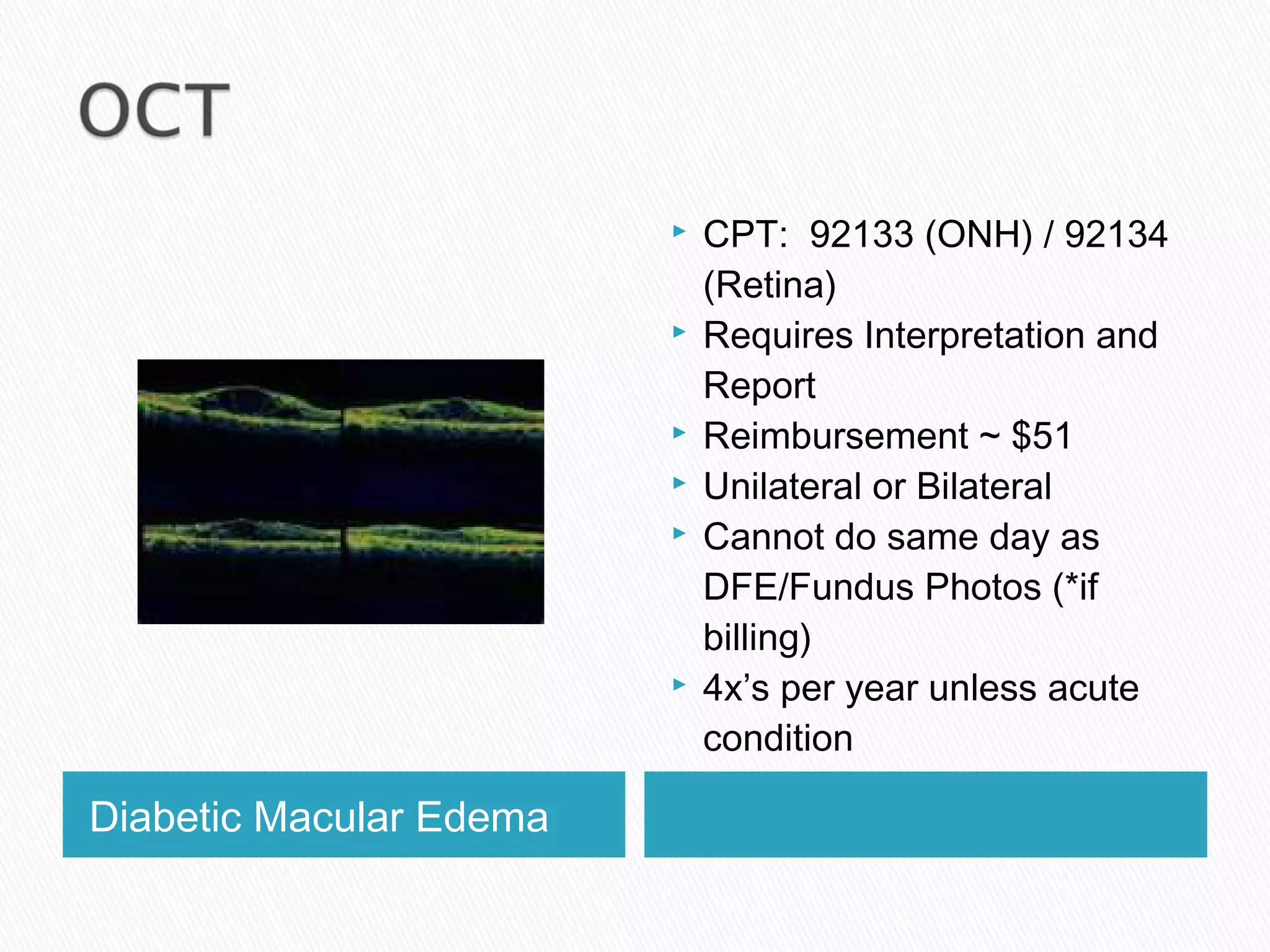
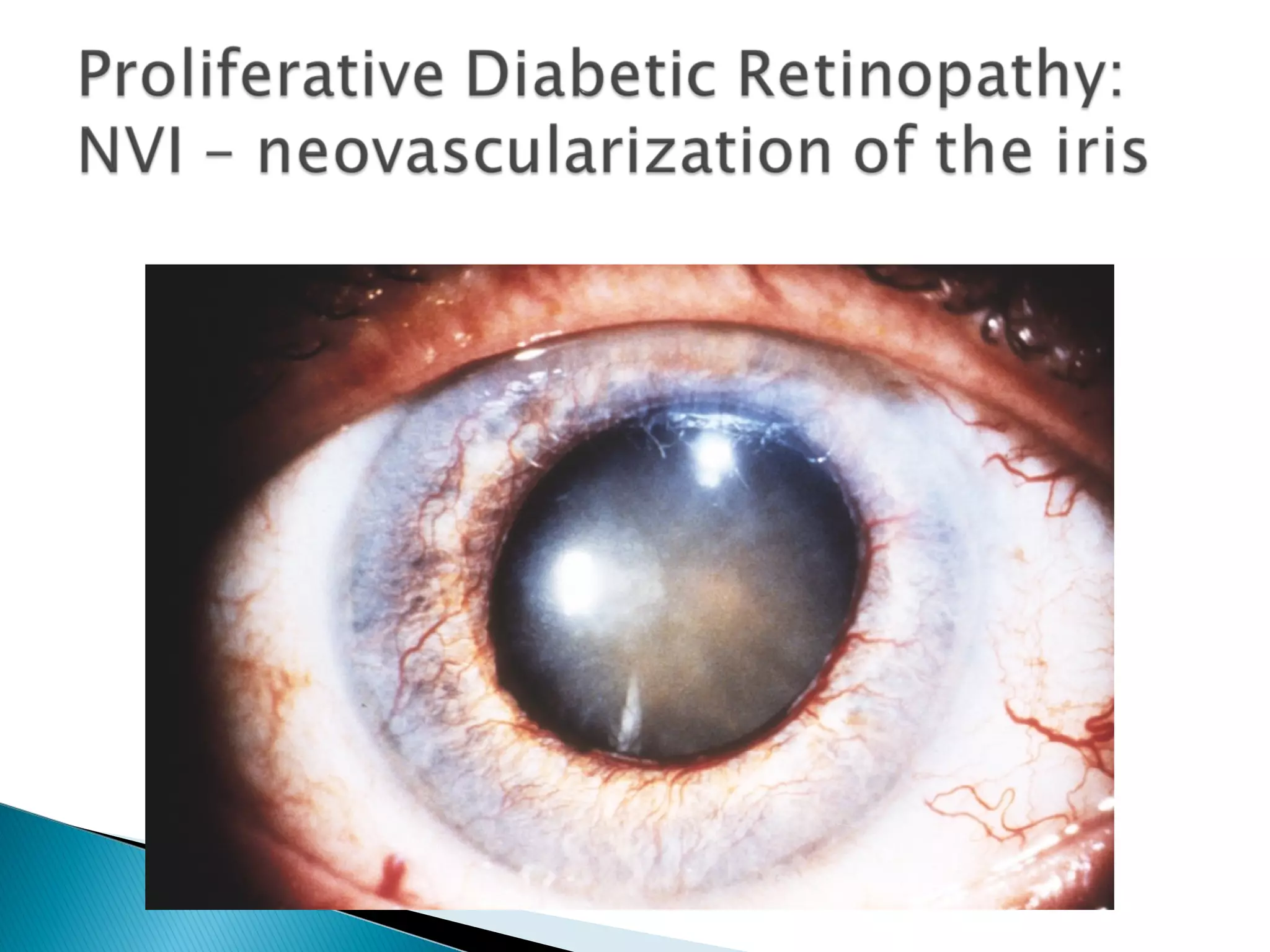
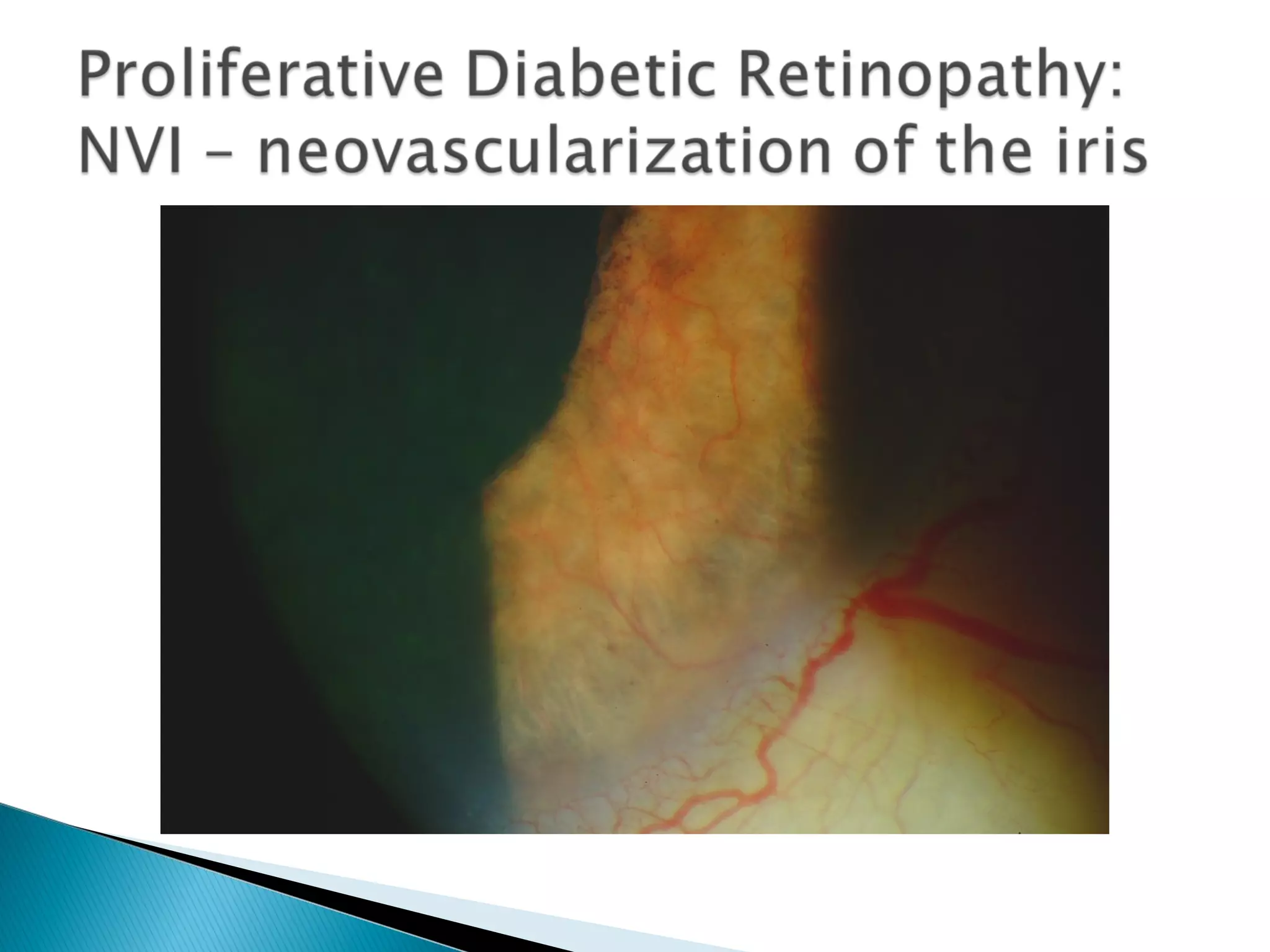
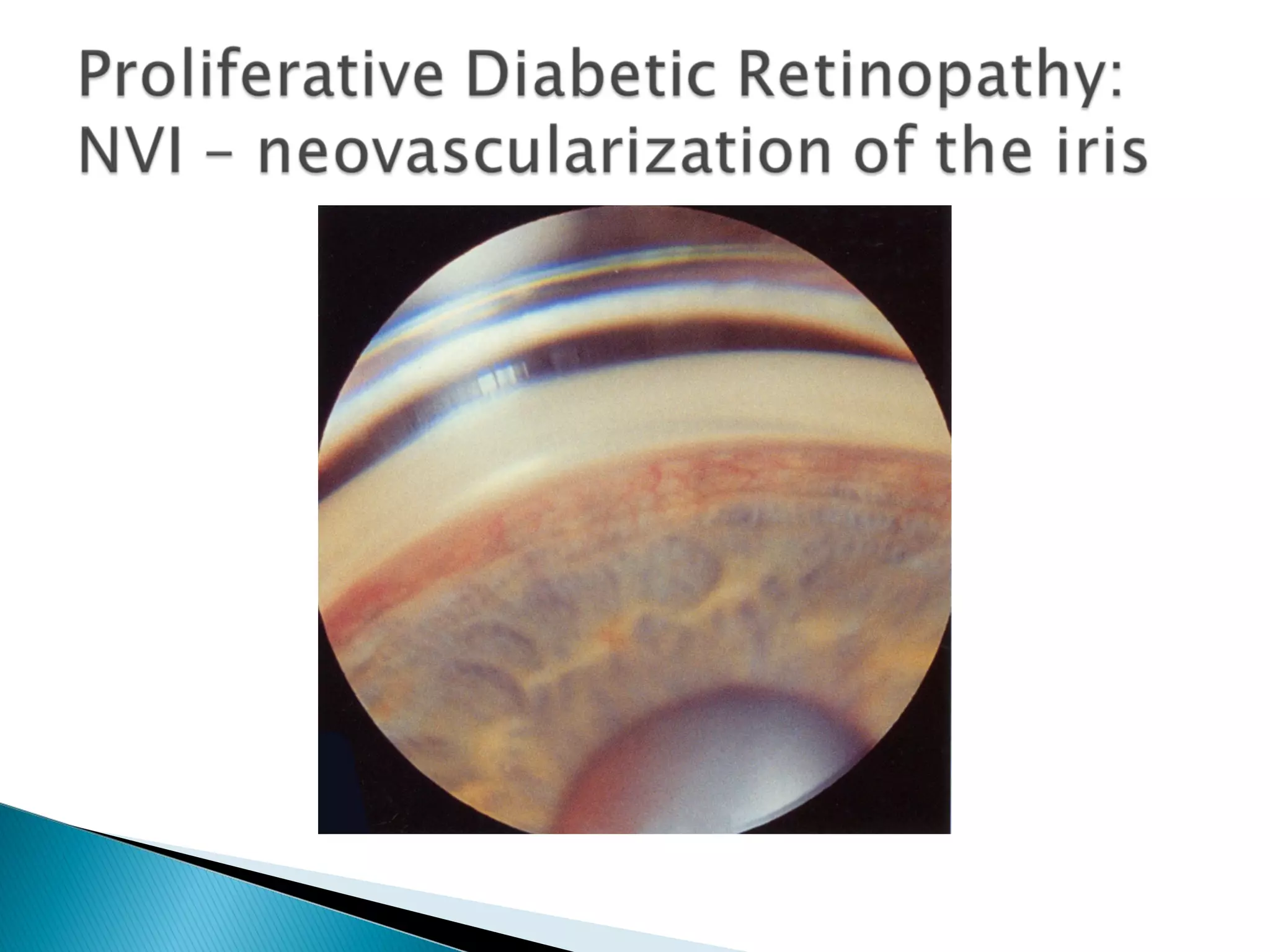
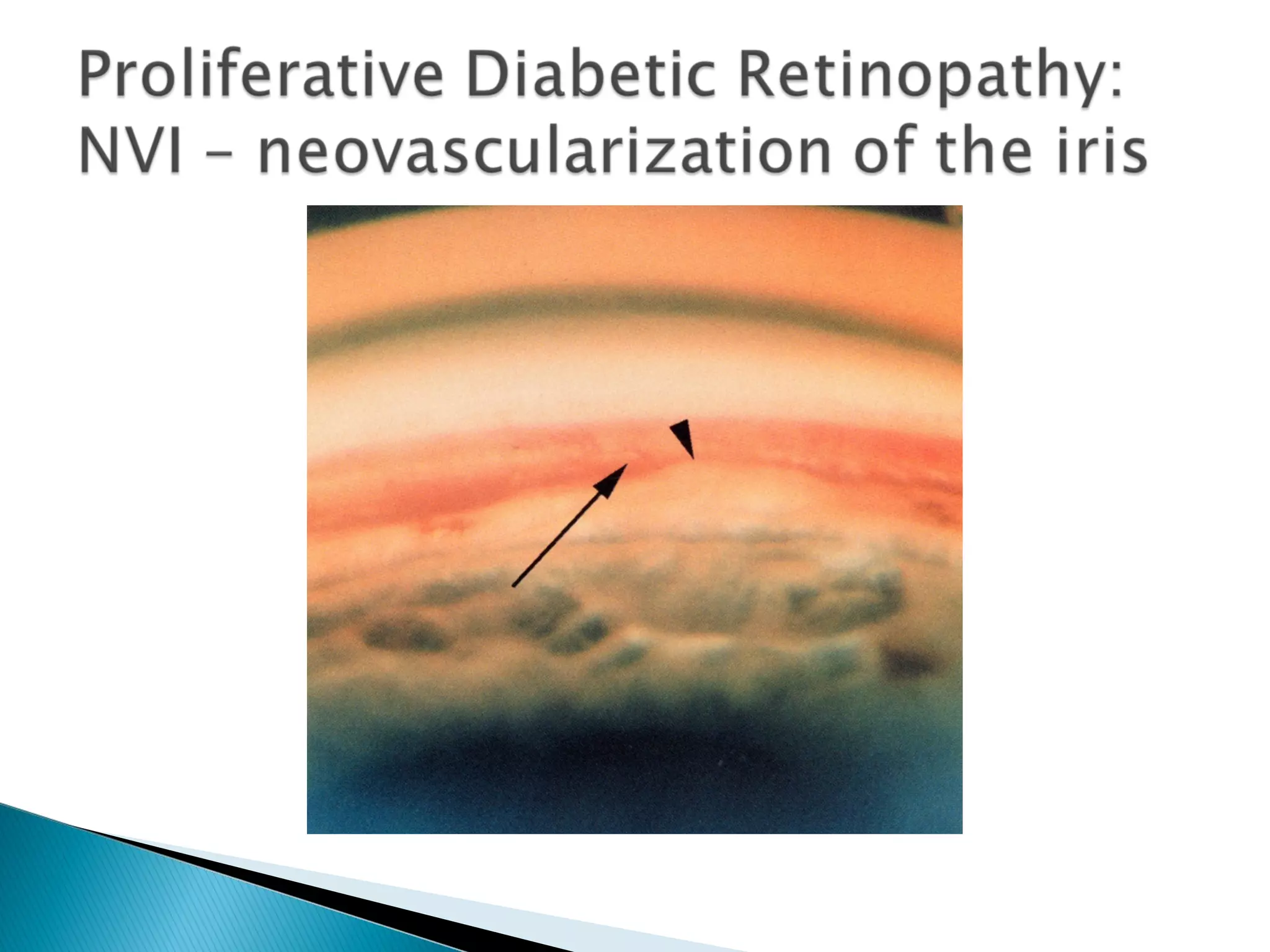
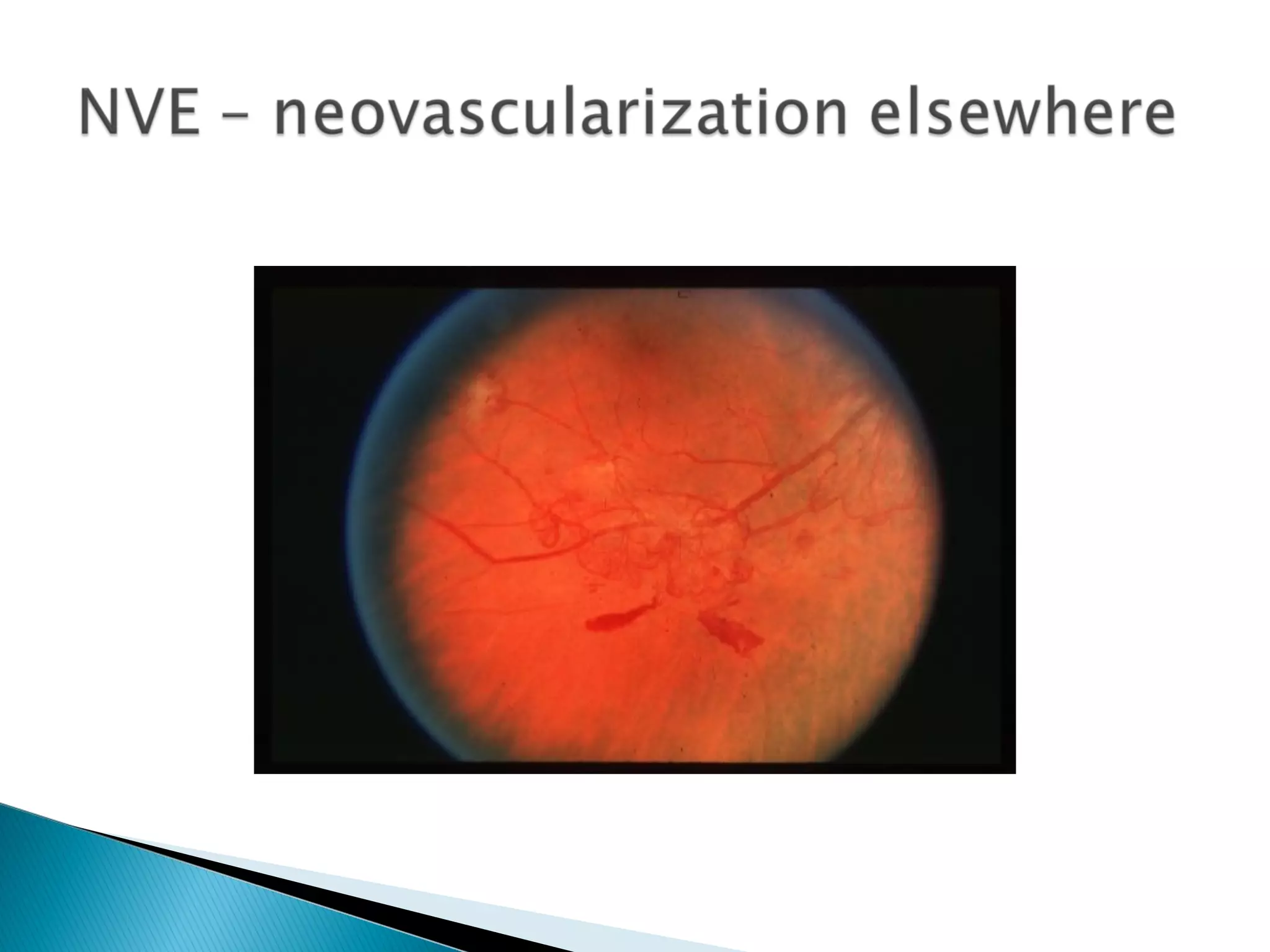
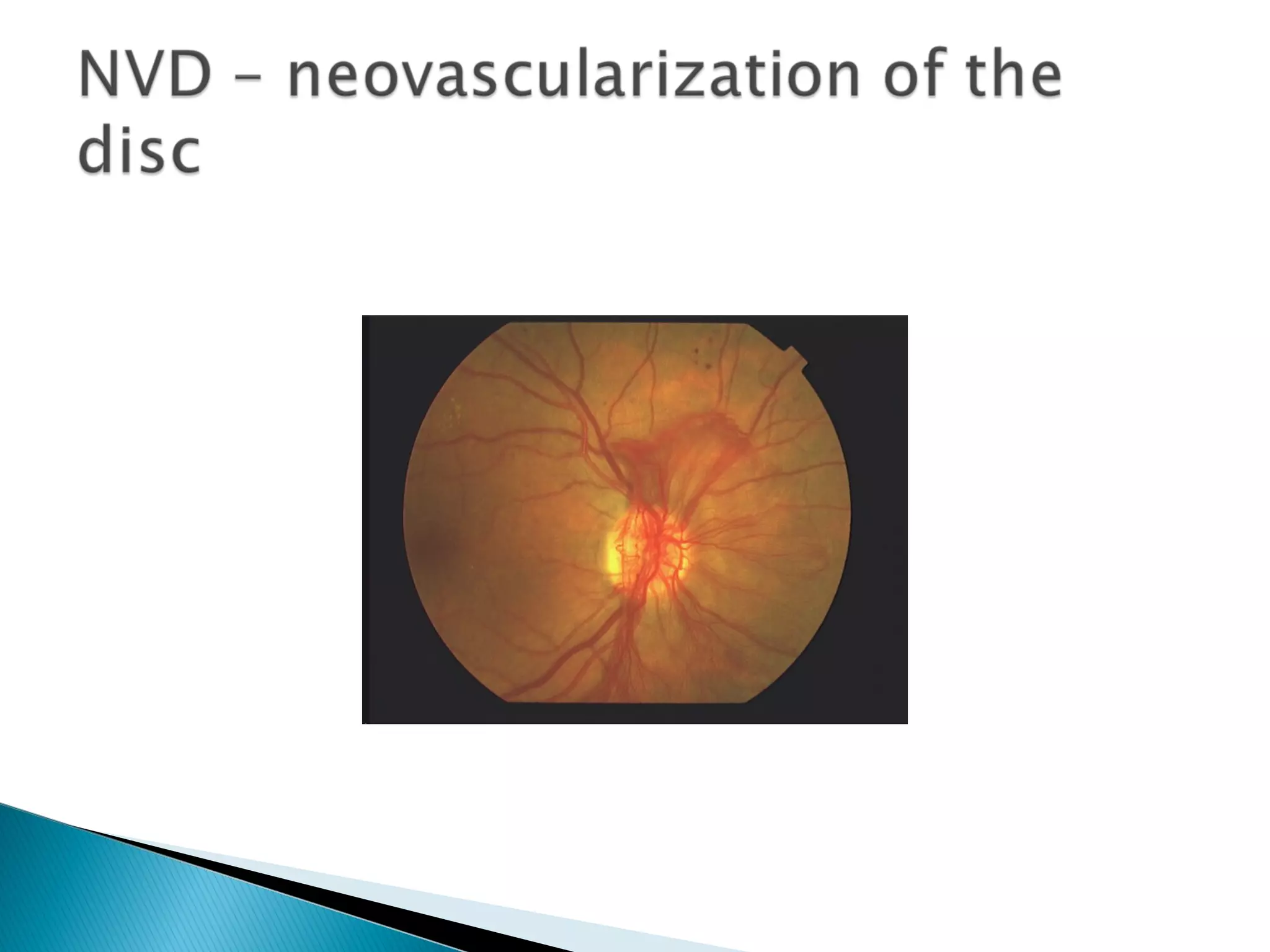
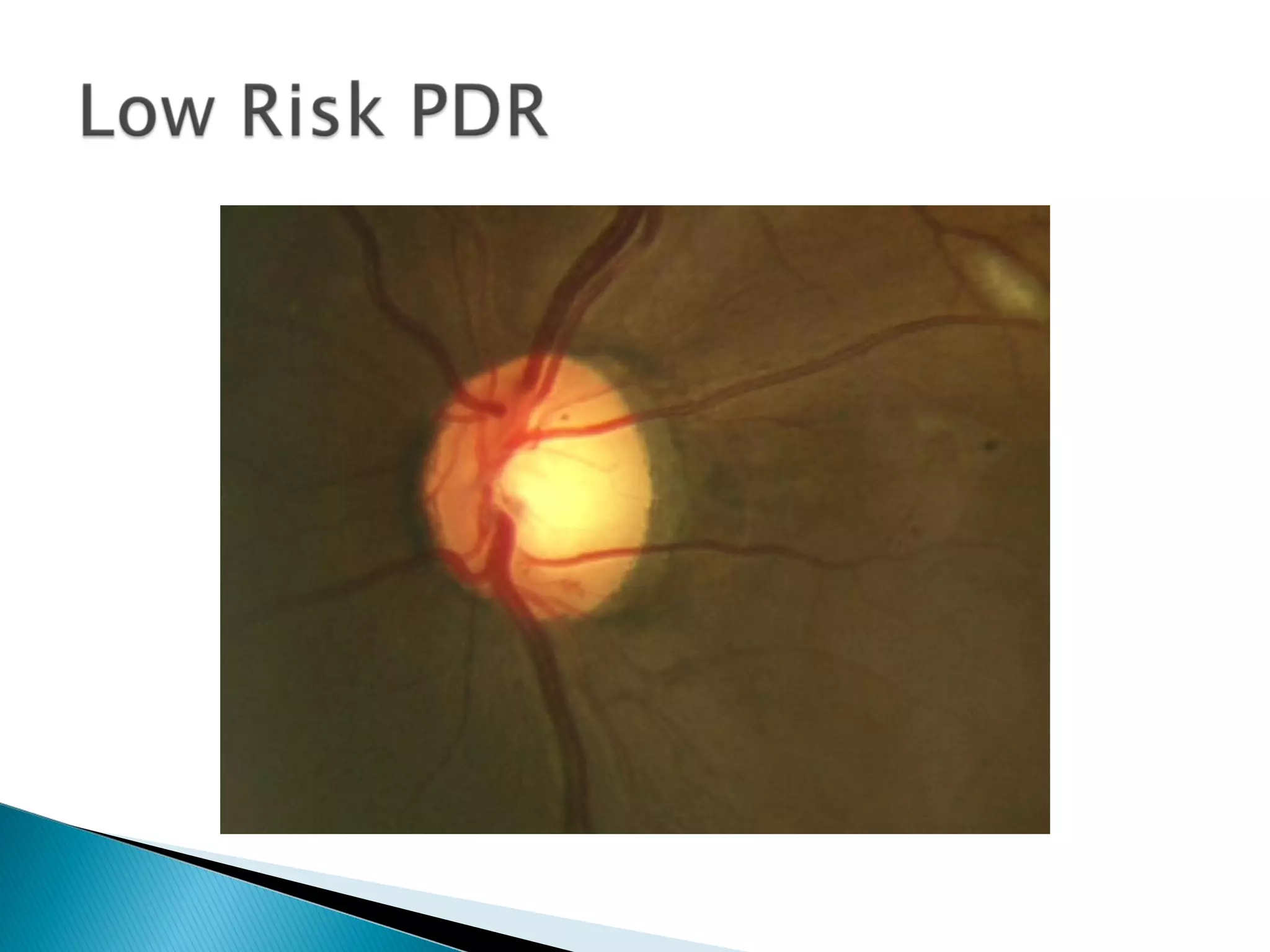
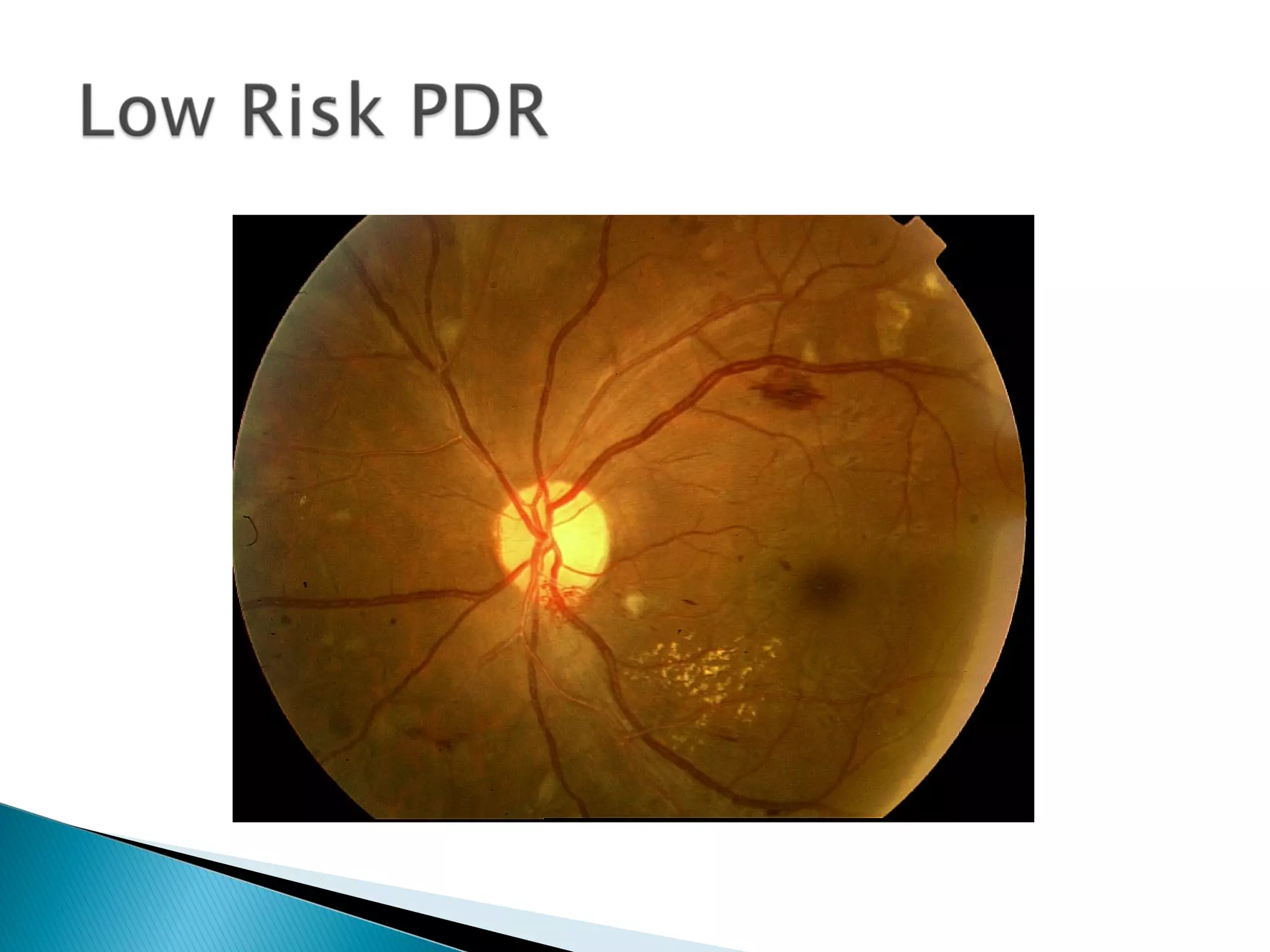
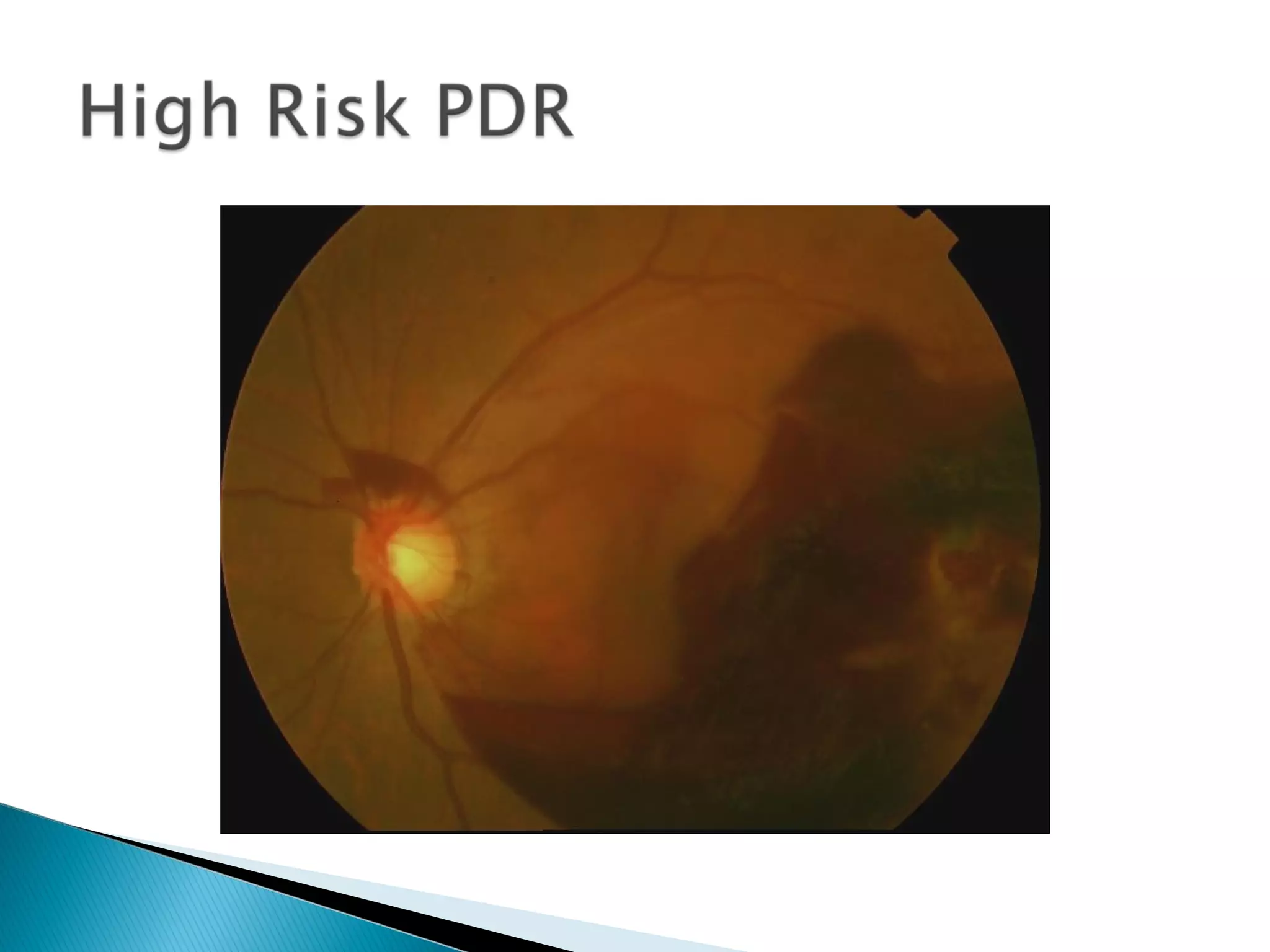
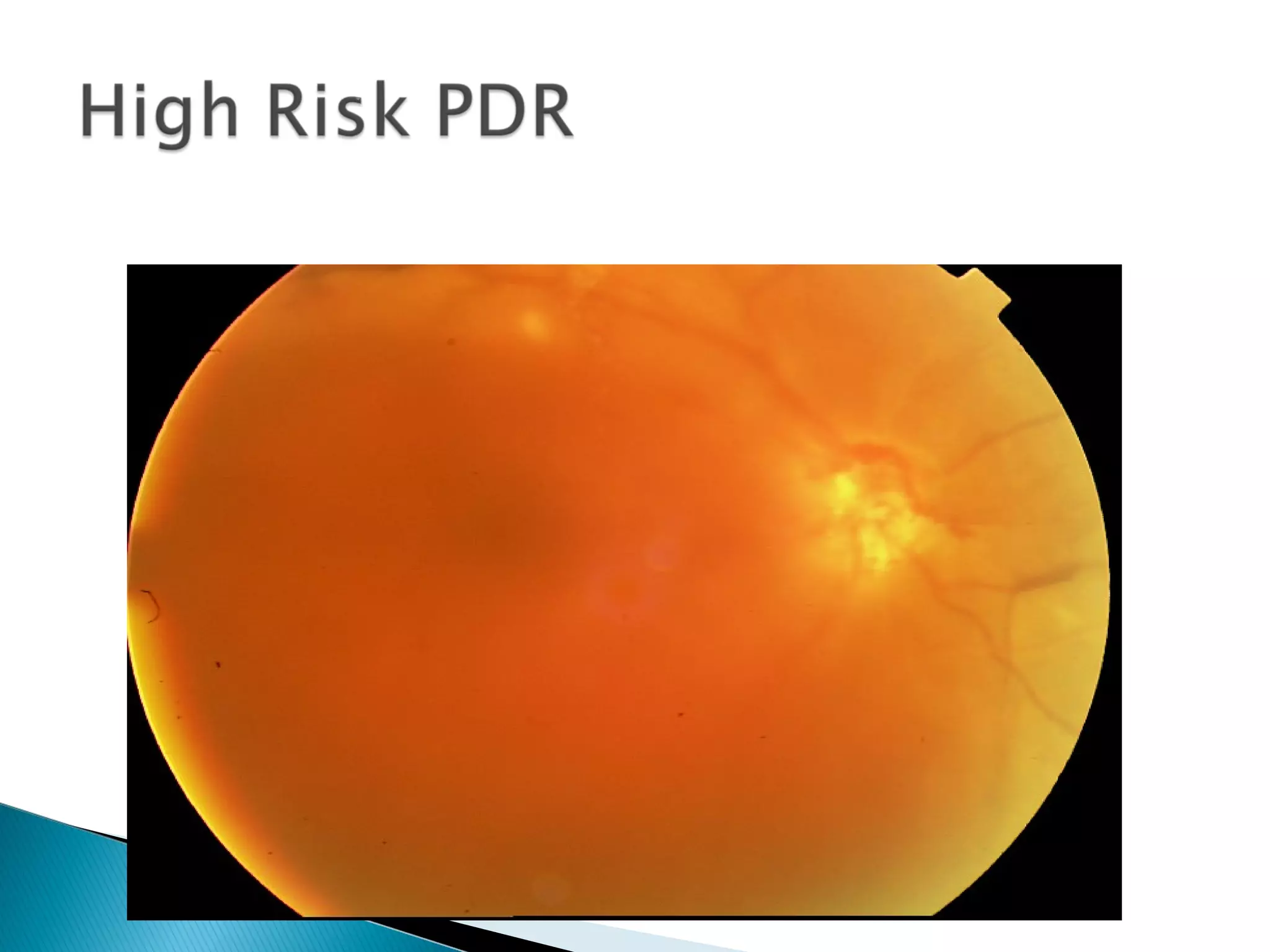
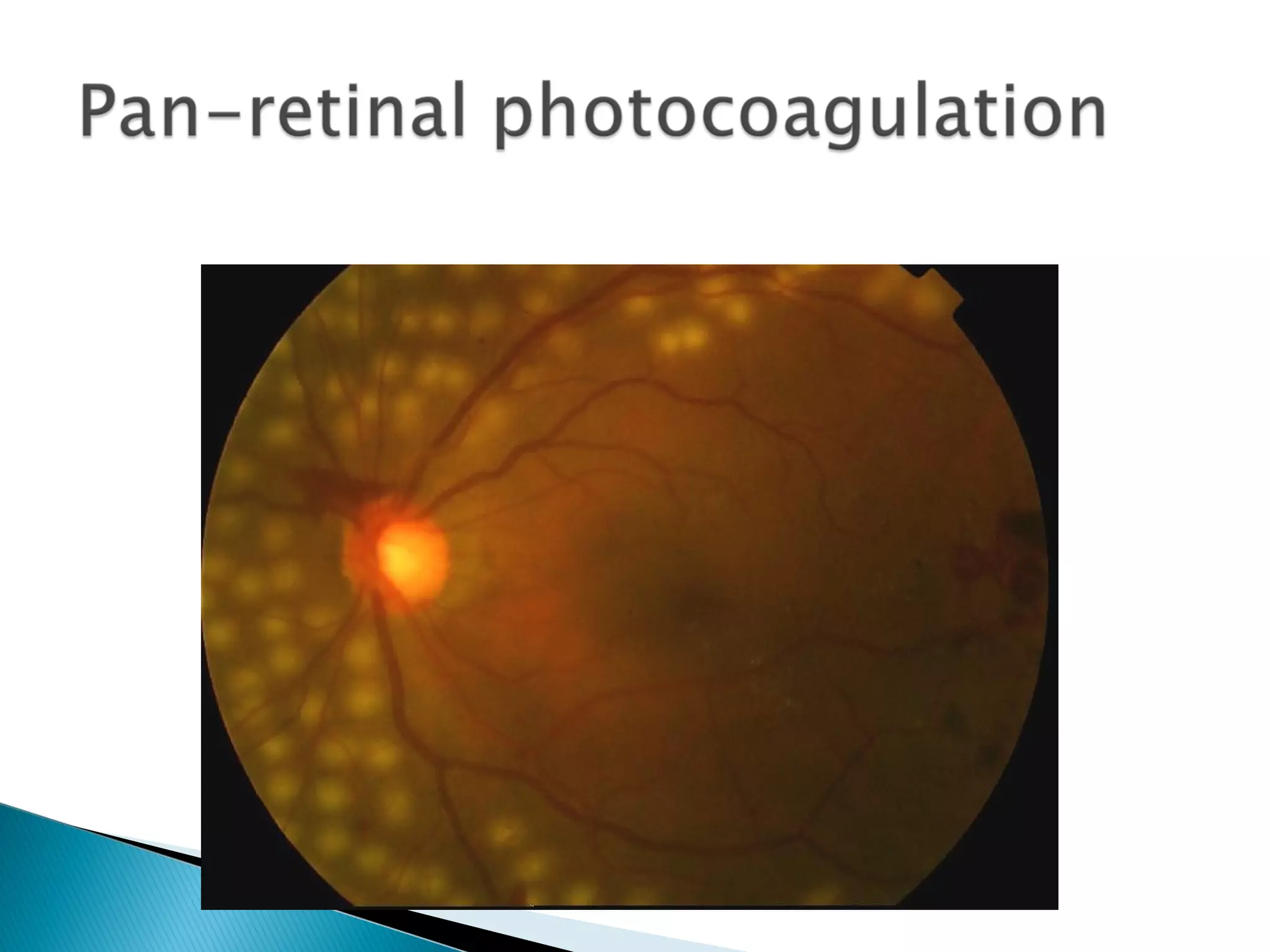
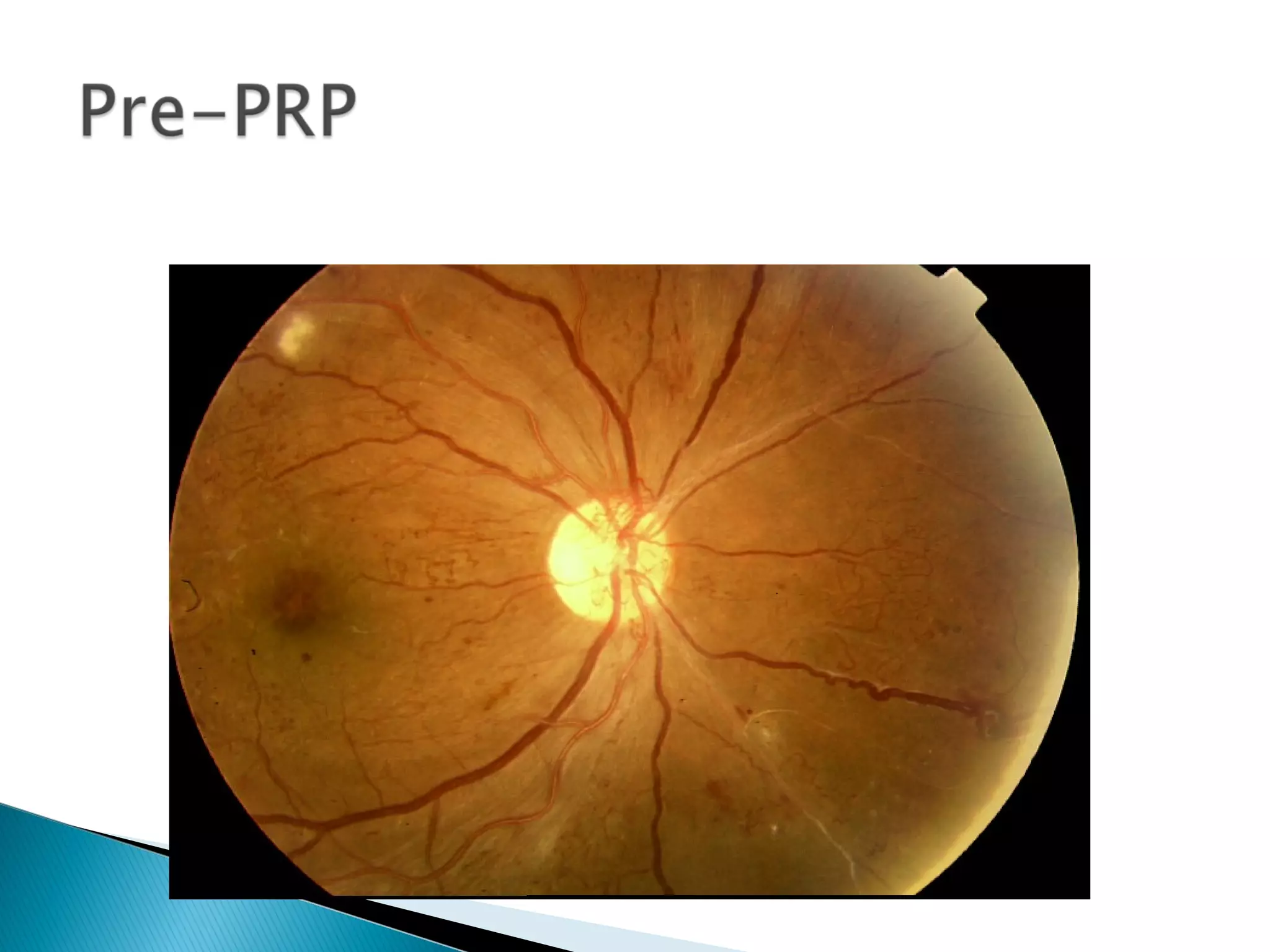
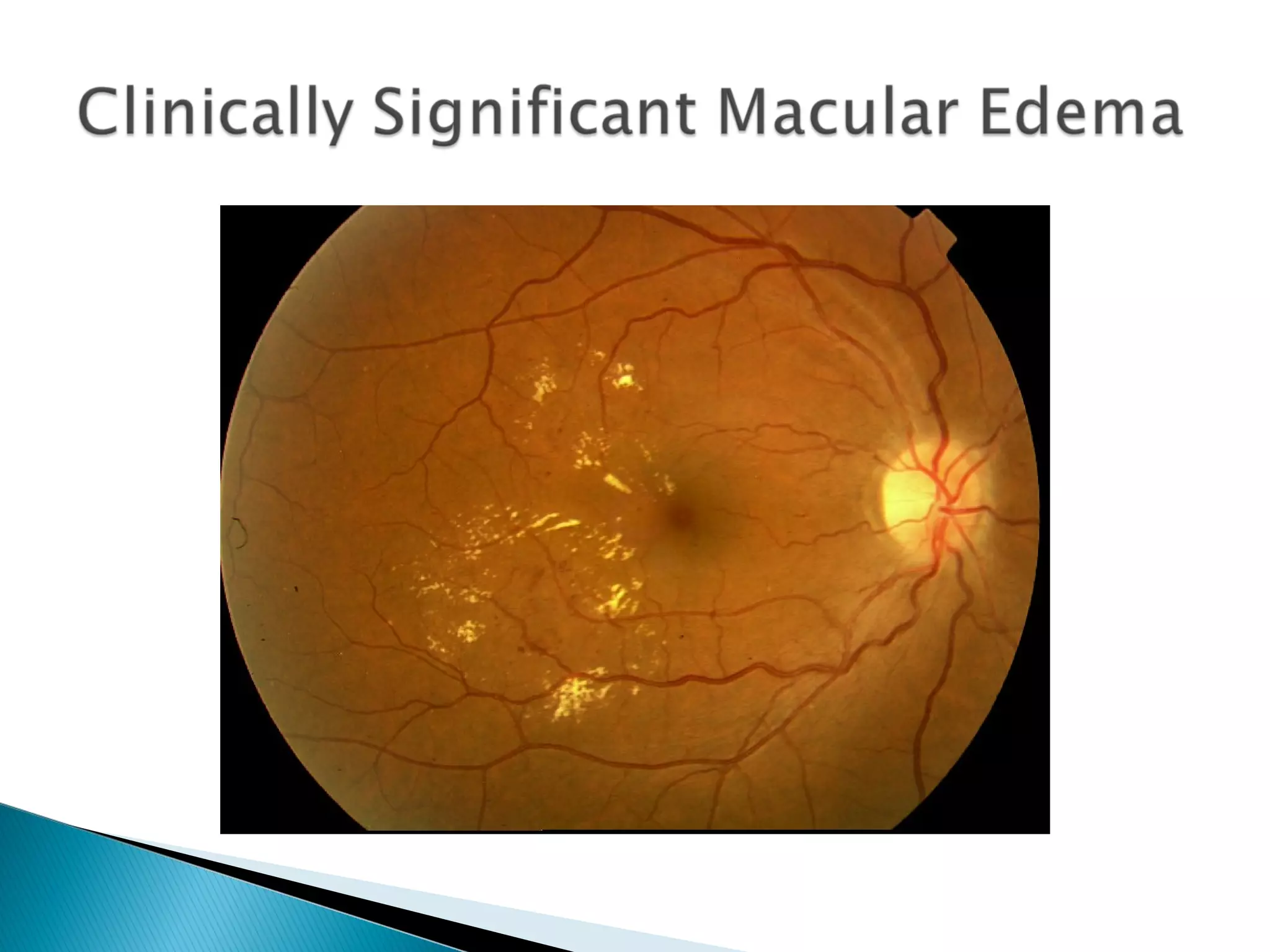
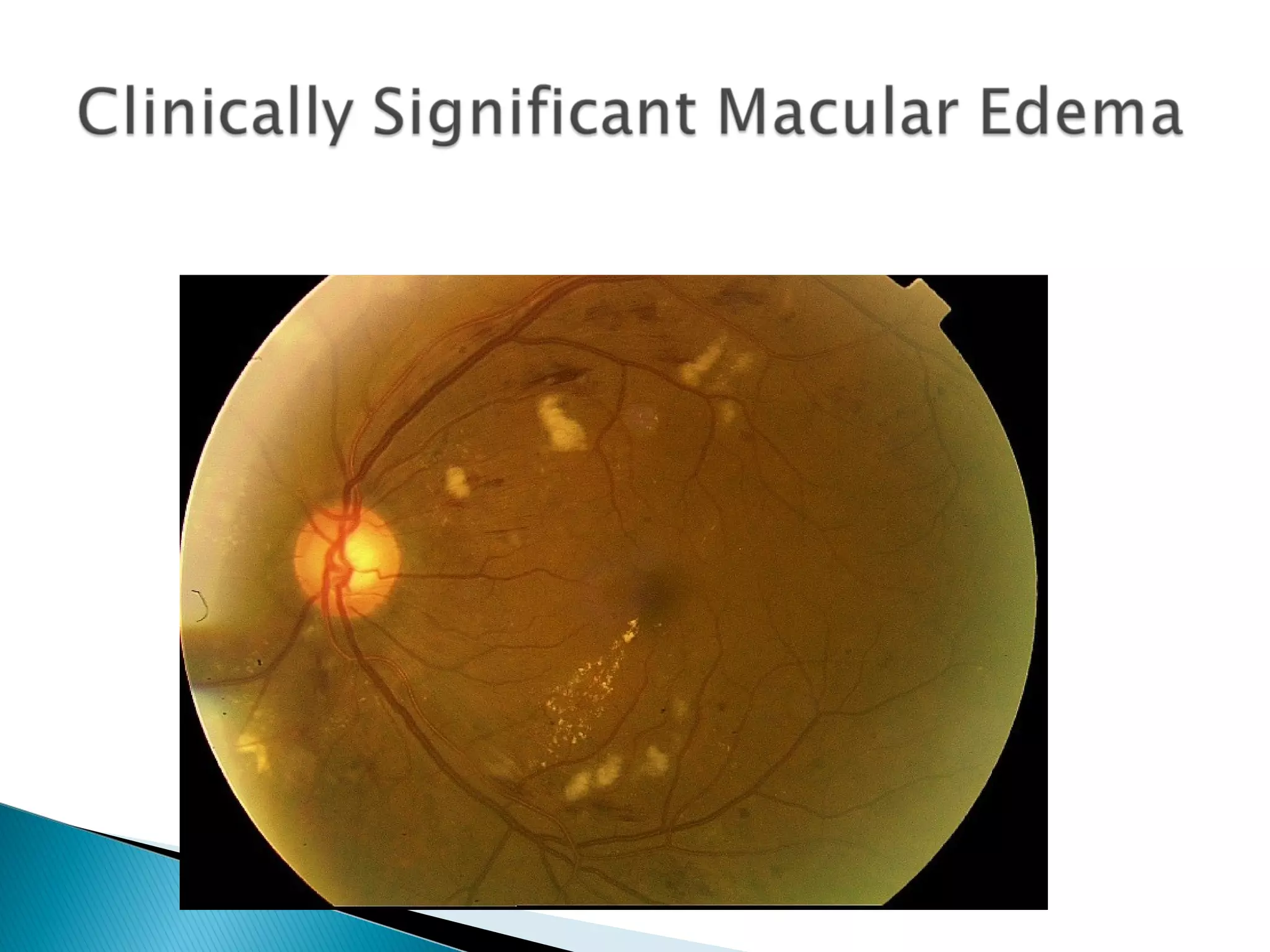
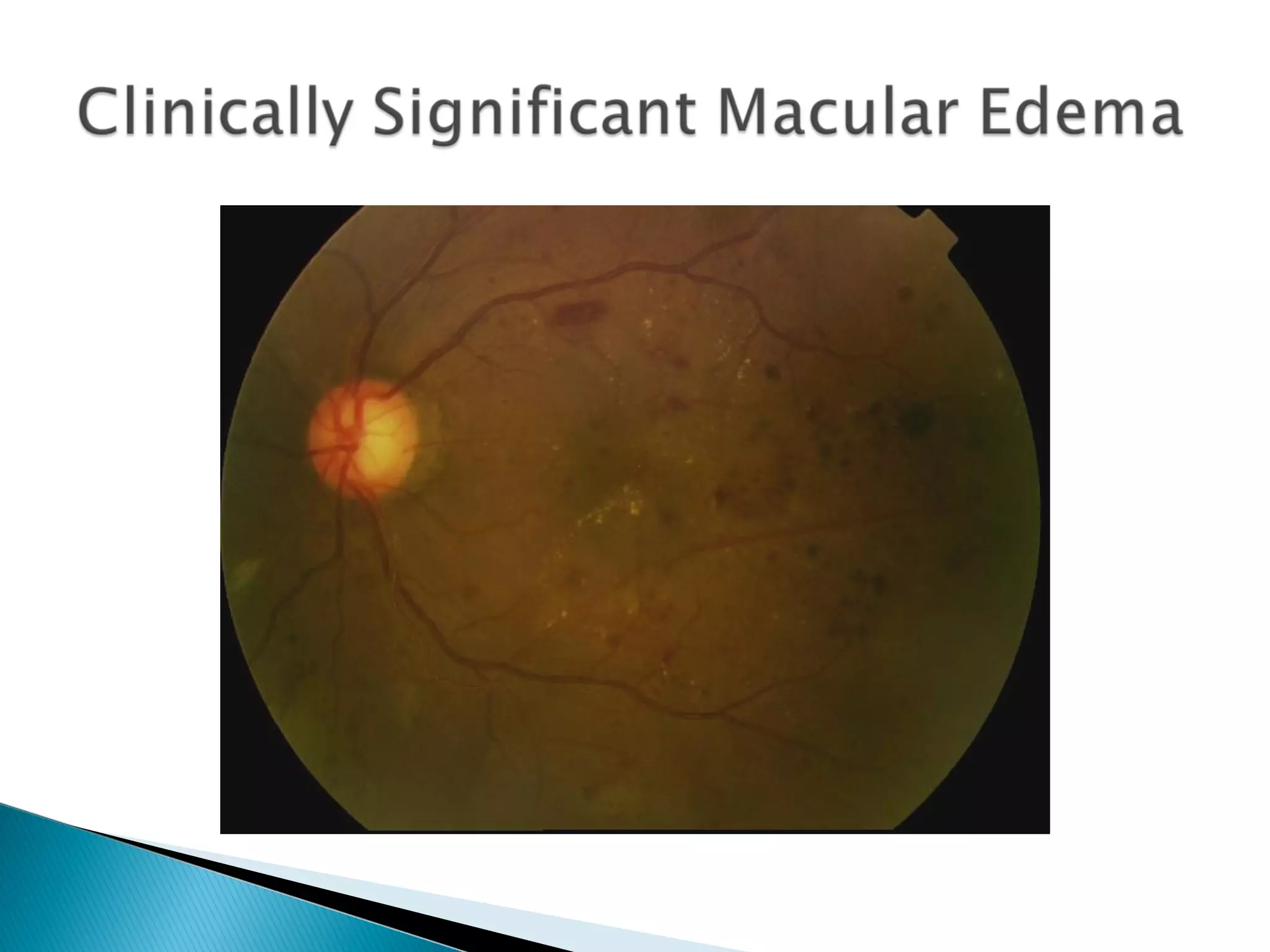
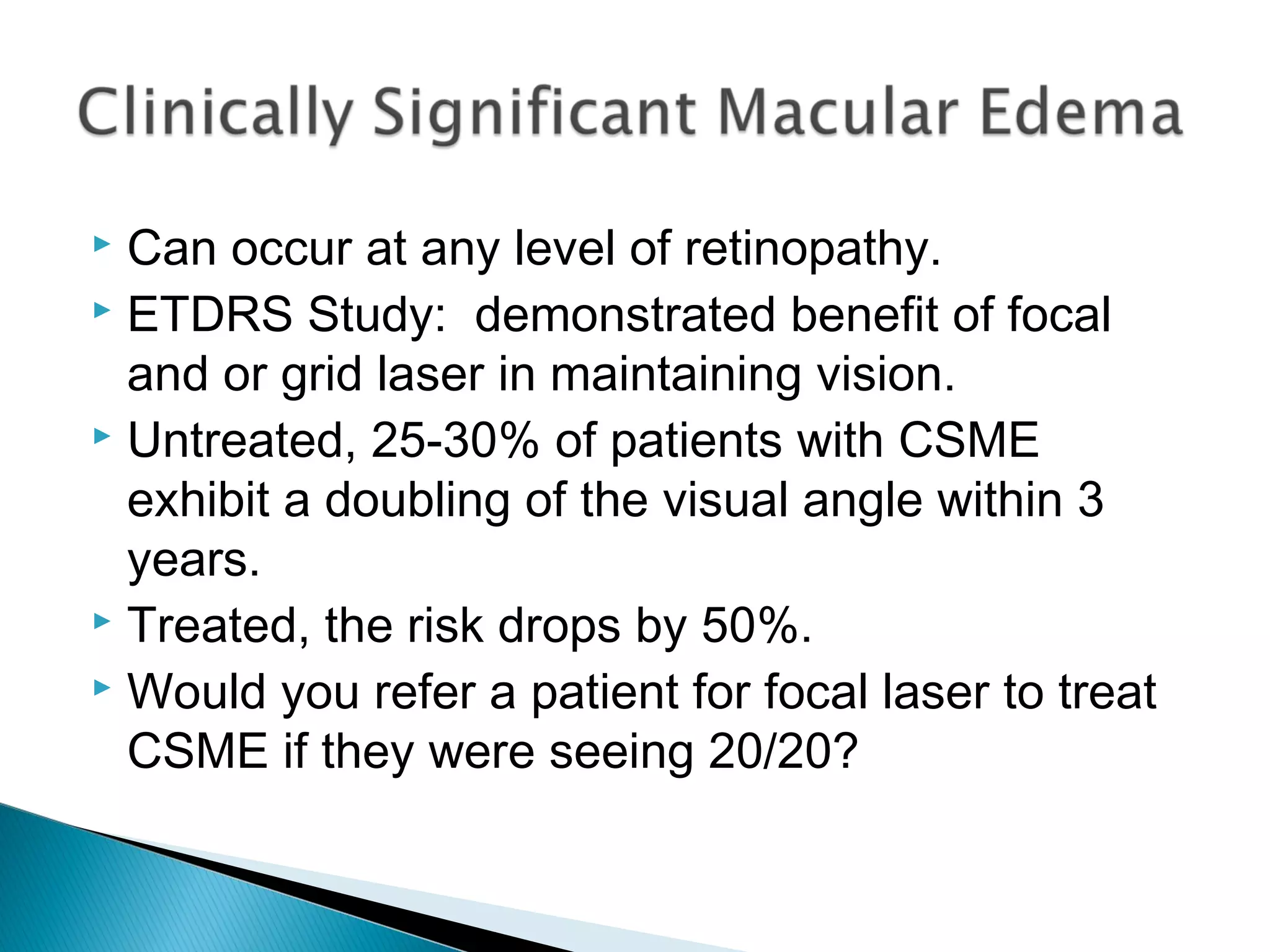
This document provides information about diabetes and diabetic retinopathy for medical students. It outlines learning objectives related to understanding diabetes demographics, diagnosis, complications, and treatments. Key points include that diabetes affects over 29 million Americans and has significant medical costs. Diabetic retinopathy is a leading cause of blindness and its progression can be slowed by controlling blood sugar and blood pressure. The document also defines the stages of diabetic retinopathy and diabetic macular edema.