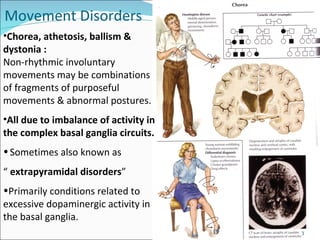
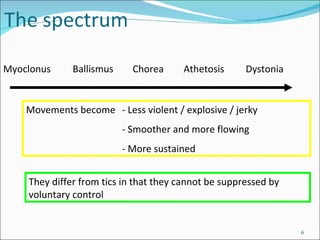
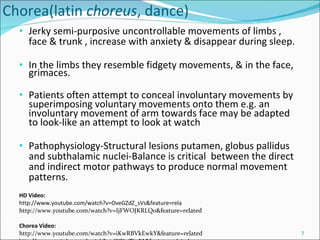
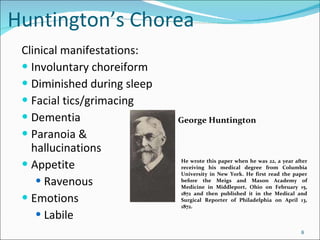
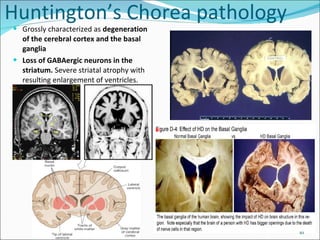
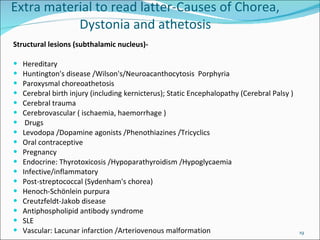
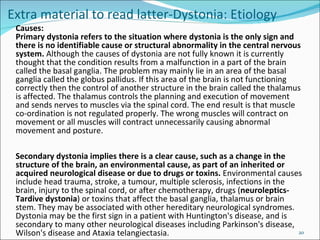
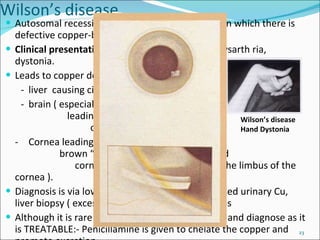
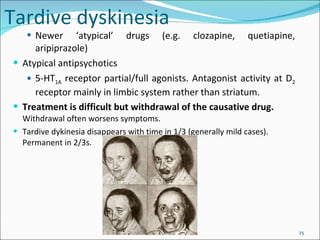
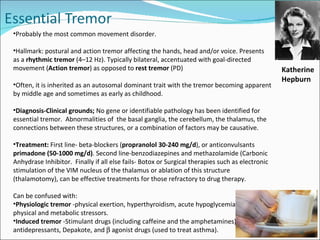
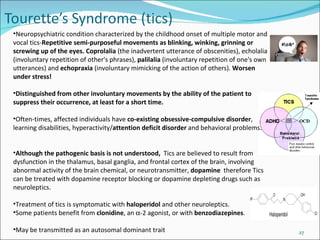
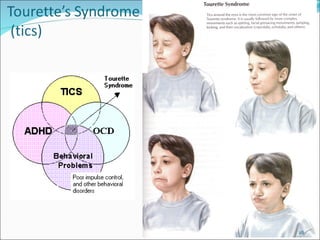
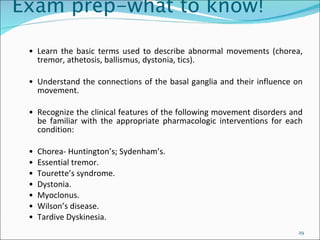
This document provides an overview of various movement disorders including chorea, athetosis, ballismus, myoclonus, Wilson's disease, tardive dyskinesia, essential tremor, and Tourette's syndrome. It describes the clinical manifestations and pathophysiology of each disorder and discusses treatment options. The disorders represent a spectrum of involuntary movements that can overlap and are often difficult to classify precisely. Accurate diagnosis relies on identifying structural lesions or genetic/environmental causes in the basal ganglia-thalamic motor circuits.