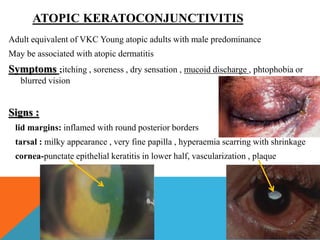
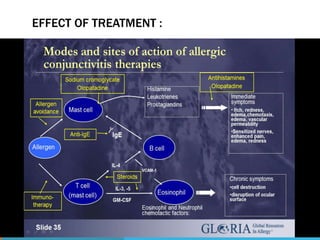
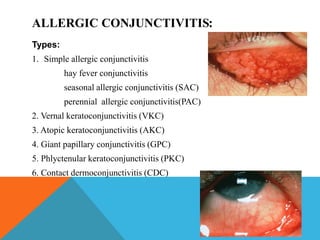
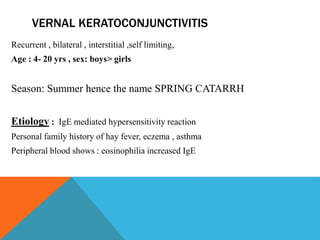
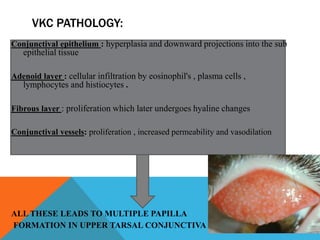
This document summarizes different types of allergic conjunctivitis including simple allergic conjunctivitis, vernal keratoconjunctivitis, atopic keratoconjunctivitis, giant papillary conjunctivitis, phlyctenular keratoconjunctivitis, and contact dermoconjunctivitis. It describes the etiology, pathology, symptoms, signs, and management of each type. For simple allergic conjunctivitis, common allergens include pollens and treatments involve reducing allergen exposure, cold compresses, tear substitutes, vasoconstrictors, mast cell stabilizers, and antihistamines. Vernal keratoconjunctivitis causes cob
![MANAGEMENT :
• Exposure to allergens should be reduced as far as possible
• Cold compresses
• Topical tear substitutes to flush out allergens
medications:
• vasoconstrictors
• Mast cell stabilizer: sodium chromoglycate 2% [QID]
• severe and non-responsive: steroids
• Systemic antihistamines : Cetirizine 10 mg OD(acute with marked
itching)](https://image.slidesharecdn.com/allergicconjunctivitis-140606123034-phpapp01/85/Allergic-conjunctivitis-6-320.jpg)
![VKC SYMPTOMS
• Intense itching & burning sensation
• Lacrimation
• Foreign body sensation
• Photophobia,
• Thick mucous discharge [ropy]
3 clinical form
• palpebral
• bulbar
• mixed form](https://image.slidesharecdn.com/allergicconjunctivitis-140606123034-phpapp01/85/Allergic-conjunctivitis-9-320.jpg)