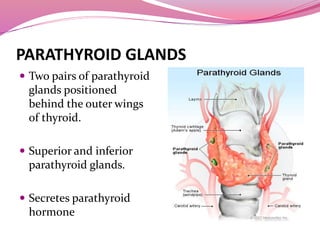
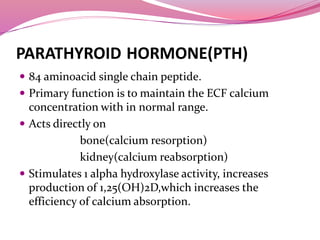
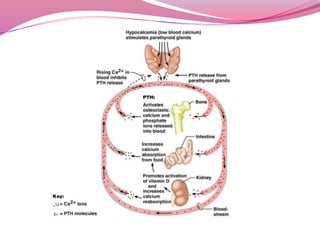
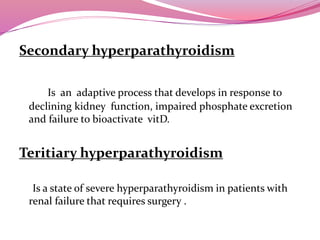
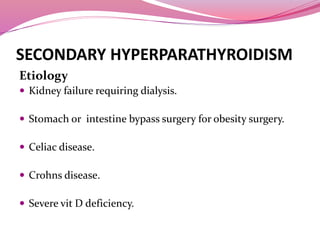
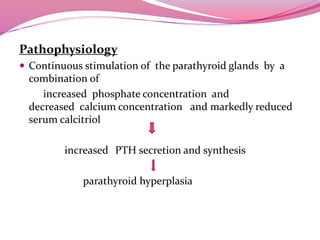
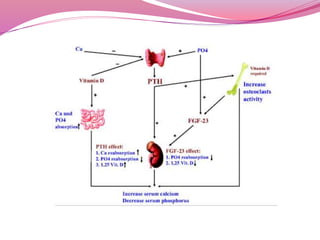
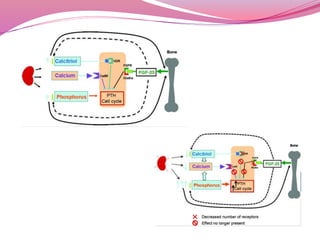
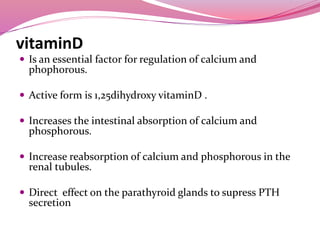
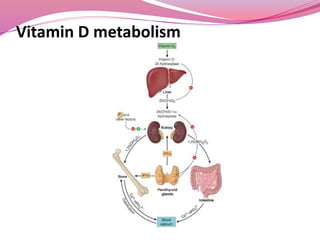
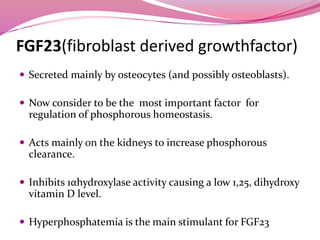
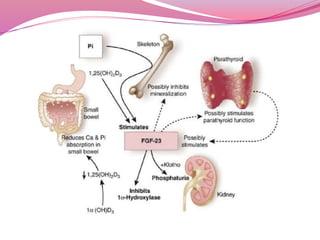
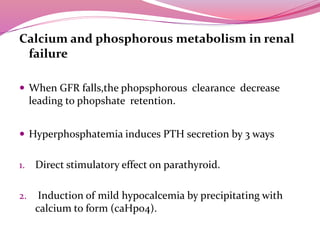
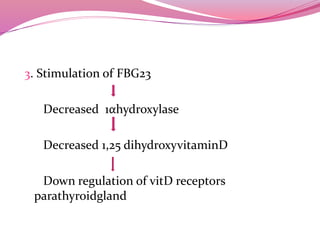
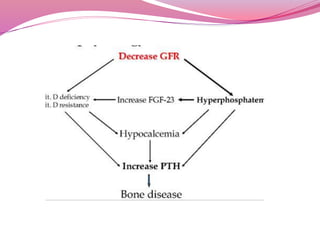
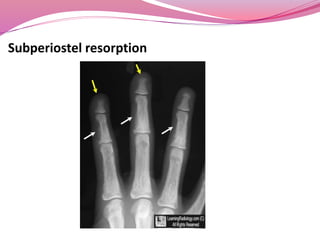
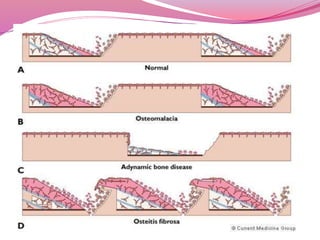
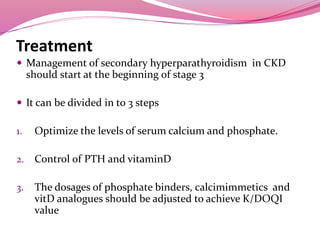
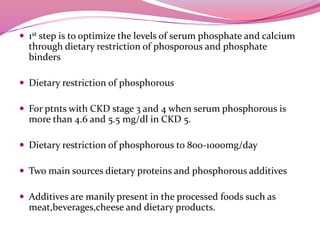
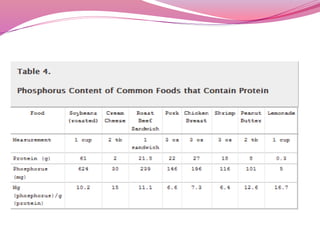
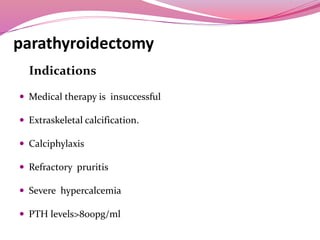
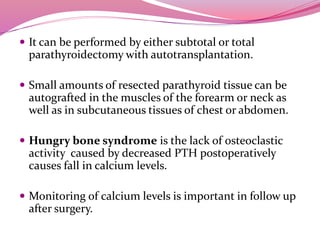
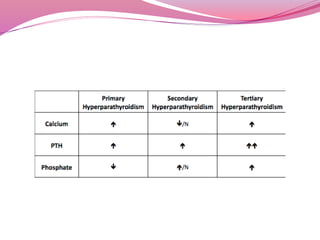
The document discusses parathyroid glands and parathyroid hormone (PTH). It notes that parathyroid glands secrete PTH, which regulates calcium levels in the blood. PTH acts on bone, kidneys, and stimulates vitamin D production. Secondary hyperparathyroidism occurs in kidney disease and is caused by low calcium and vitamin D levels stimulating increased PTH secretion. Treatment focuses on controlling calcium, phosphate, PTH, and vitamin D levels through diet, binders, analogs, and calcimimetics. For refractory cases, parathyroidectomy may be required.