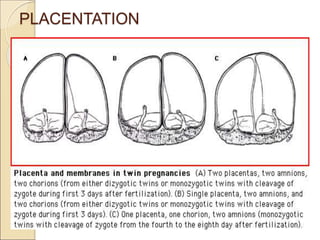
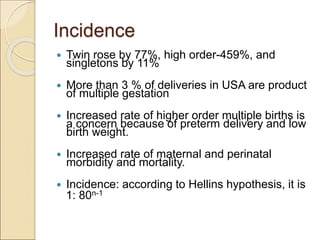
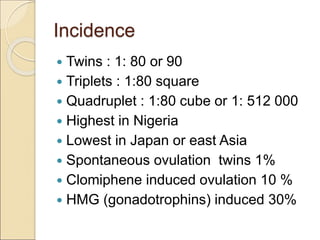
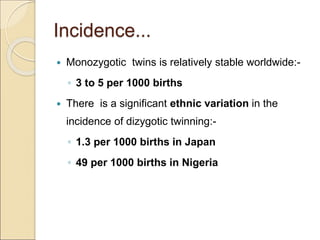
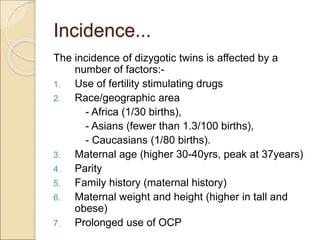
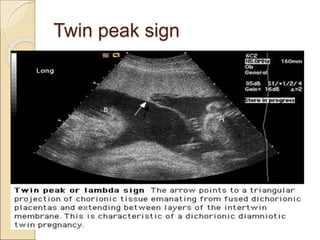
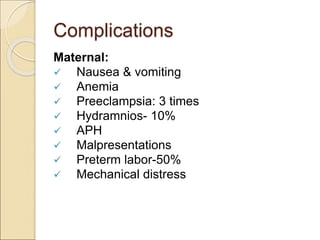
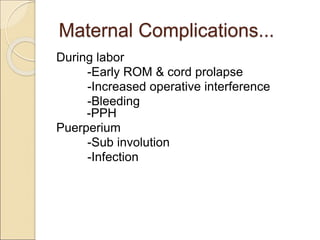
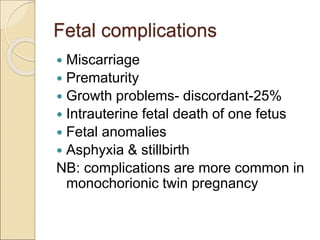
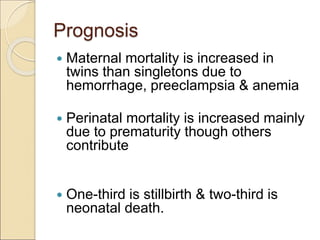
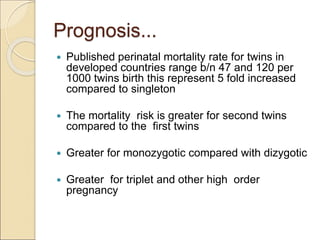
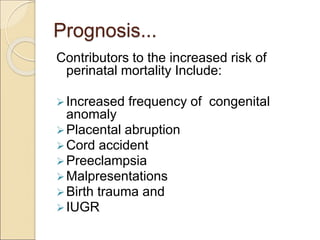
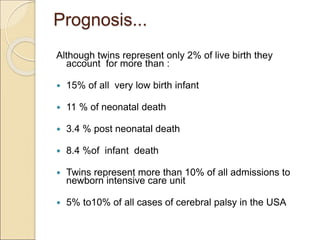
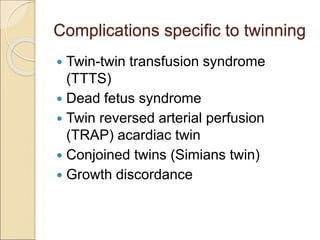
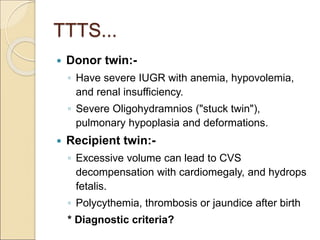
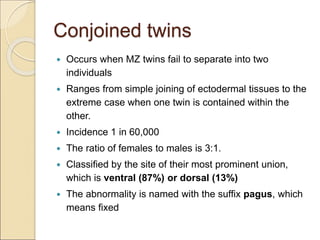
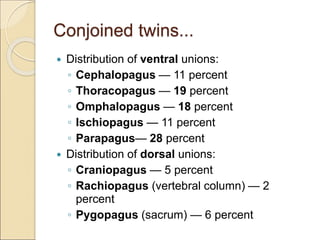
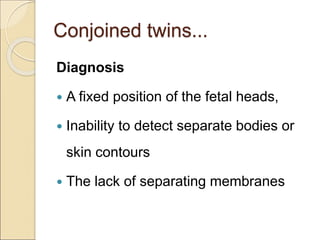
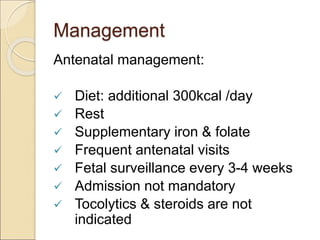
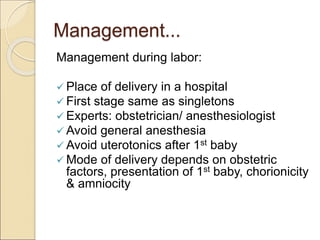
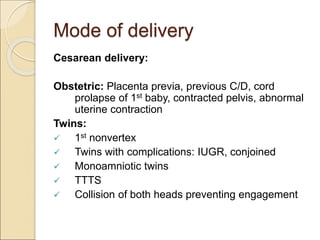
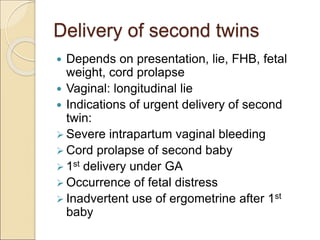
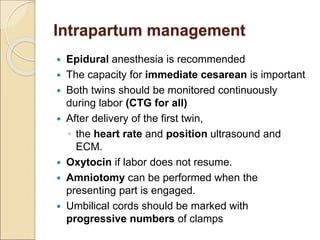
This document discusses multifetal pregnancies, including twins, triplets, and higher order multiples. It defines key terms, describes the types and incidence of twins. Complications are more common in multifetal pregnancies and include preterm birth, preeclampsia, and increased risk of stillbirth. Specific complications discussed include twin-twin transfusion syndrome and conjoined twins. The management of multifetal pregnancies during antenatal, intrapartum, and postpartum periods is also summarized.