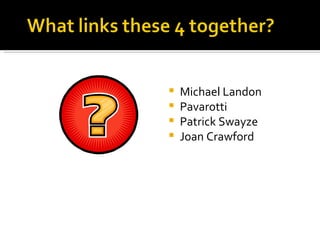
Michael Landon, Luciano Pavarotti, Patrick Swayze, and Joan Crawford all died of pancreatic cancer. Pancreatic cancer has a very poor prognosis, with most patients dying within a year of diagnosis. Risk factors include smoking, obesity, family history, and certain genetic conditions. Treatment options depend on how advanced the cancer is and may include surgery, chemotherapy, radiation, and targeted therapies. However, pancreatic cancer remains very difficult to treat due to late diagnosis and lack of effective therapies.