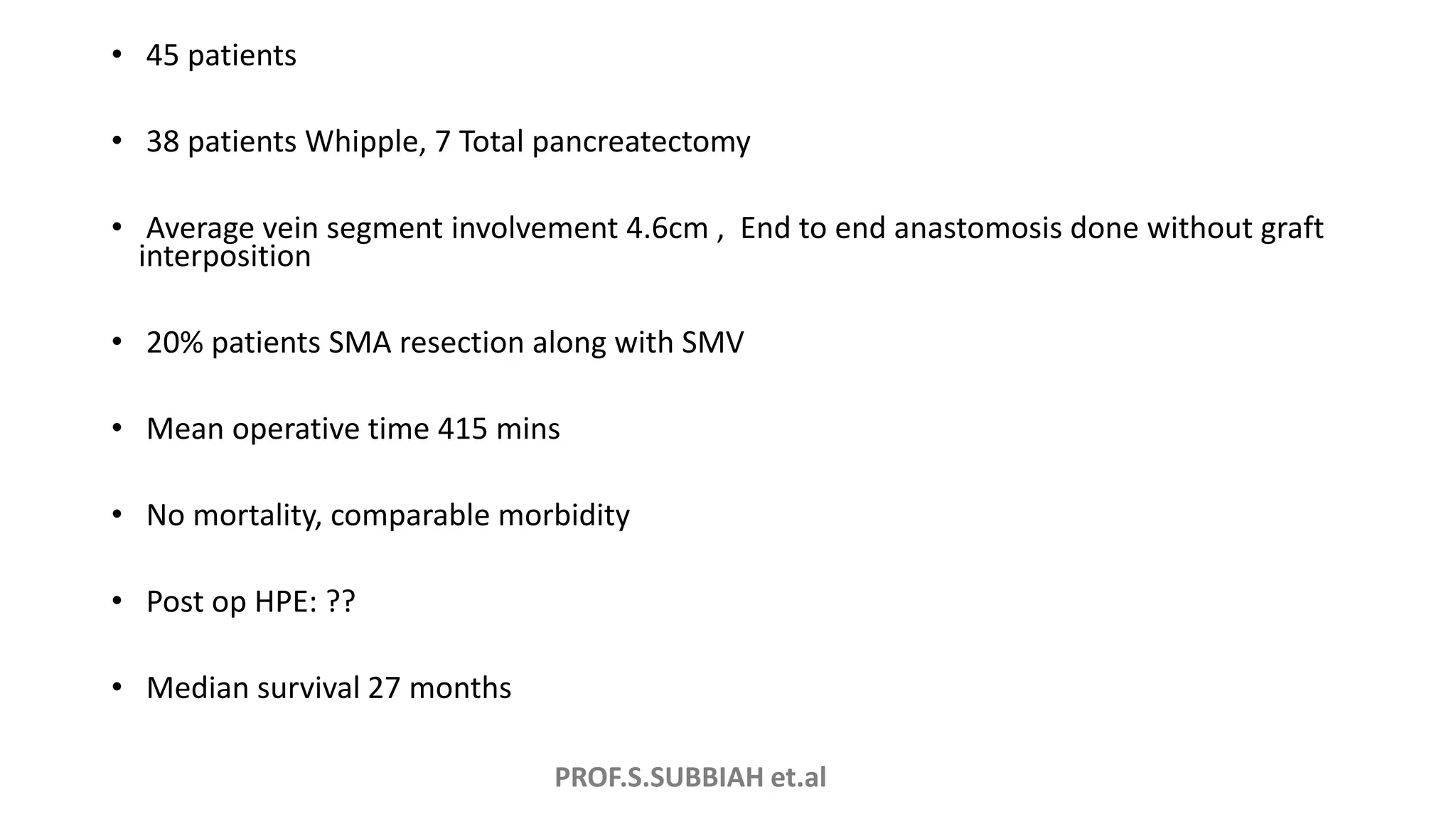
The document discusses recent surgical updates for pancreatic resections. It introduces novel techniques for pancreatic resections like the Cattell Braasch maneuver, triangle operation, and modified Appleby procedure. It summarizes outcomes from using these techniques on 45 patients, finding no mortality and comparable morbidity. The document also discusses techniques like vein resection without reconstruction that can increase resectability in select cases.