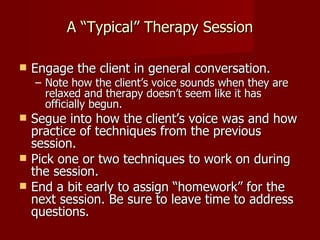
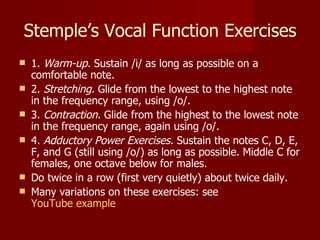
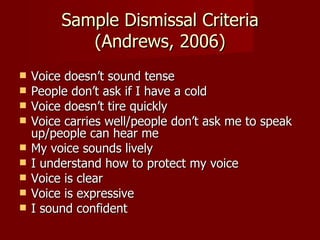
This document discusses various techniques and approaches used in voice therapy, including relaxation, respiration training, elimination of vocal abuses, and vocal function exercises. It emphasizes that successful therapy requires a holistic approach combining behavioral, cognitive, and counseling techniques tailored to the individual client. Progress is measured through pre- and post-therapy voice recordings, instrumentation, and tracking improvement across specific criteria.