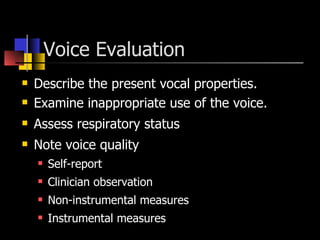
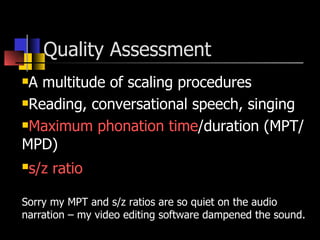
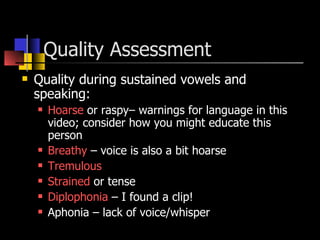
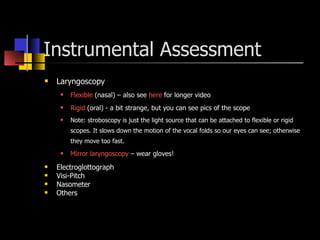
The document outlines the objectives and process for conducting a voice evaluation. The primary objective is to determine if the client has a voice disorder and evaluate symptoms. Additional objectives include patient education and establishing credibility. The evaluation should gather information on referral source, reason for referral, history of the problem, medical history, social history, and oral mechanism exam. Formal assessments include describing vocal qualities, respiratory status, and instrumental measures. The evaluator should rely on auditory perceptions over instrumentation and not make treatment recommendations without an ENT evaluation.