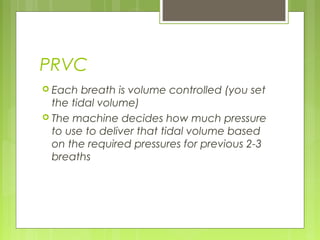
This document is a primer on mechanical ventilation by Dr. Firas Rabi, outlining indications for use, ventilator origins, terminology, and various modes of ventilation. It details the mechanics of pressure and volume control, the role of positive end-expiratory pressure (PEEP), and the differences between CPAP and BiPAP. Additionally, it emphasizes the importance of initial settings, oxygenation strategies, high-frequency ventilation, and troubleshooting techniques related to mechanical ventilation.