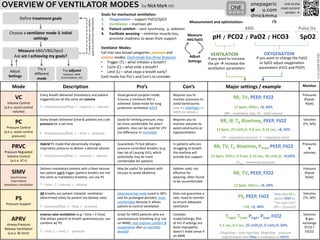
This document provides an overview of different ventilator modes, including volume control (VC), pressure control (PC), pressure regulated volume control (PRVC), synchronous intermittent mandatory ventilation (SIMV), pressure support (PS), and airway pressure release ventilation (APRV). For each mode, it describes the mode, pros, cons, and major settings. It emphasizes measuring blood gases and oxygen saturation to assess if treatment goals are being achieved and adjusting ventilator settings accordingly. The goals of mechanical ventilation are supporting oxygenation and ventilation while promoting patient comfort and readiness to wean from support.