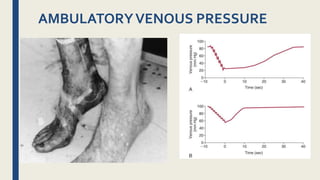
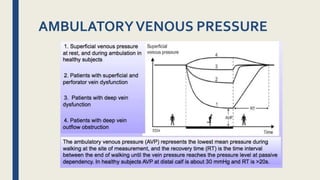
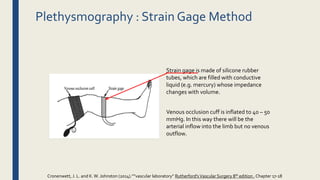
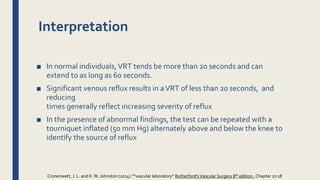
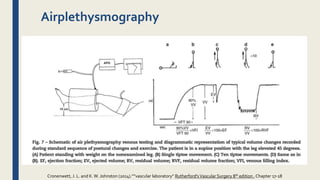
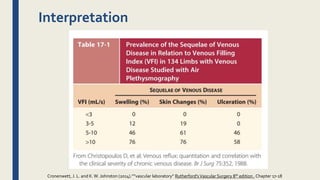
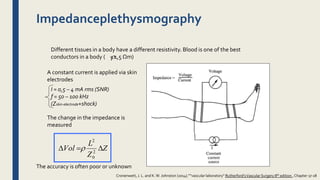
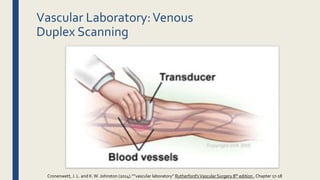
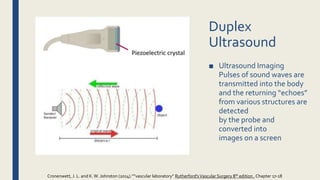
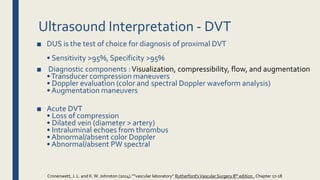
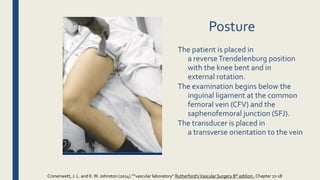
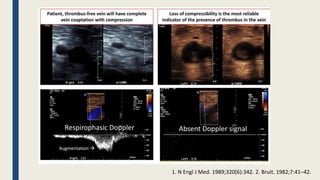
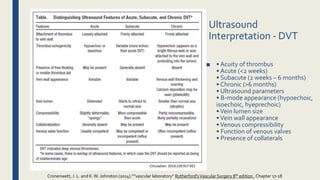
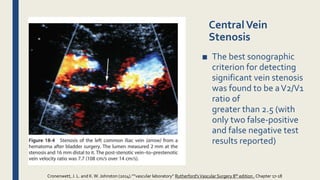
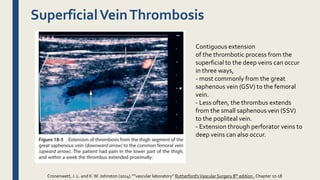
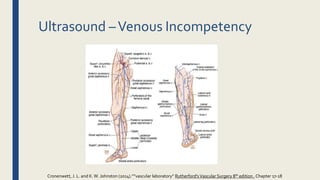
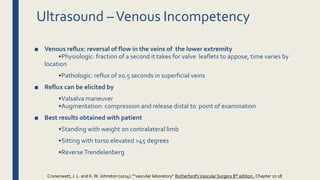
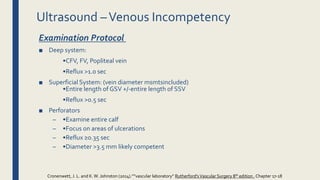
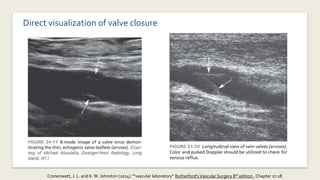
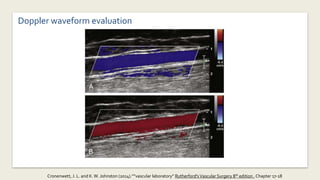
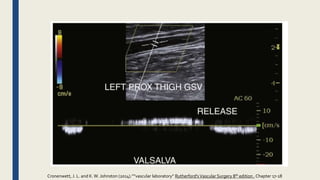
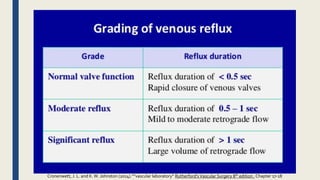
This document provides an overview of venous physiology assessment techniques performed in vascular laboratories, including ambulatory venous pressure measurement, plethysmography, and duplex ultrasound scanning. It describes how each test is performed and what it evaluates. Ambulatory venous pressure directly measures pressure in foot veins and is considered the gold standard, but it is invasive. Plethysmography uses strain gauges or impedance to estimate volume changes during venous occlusion and identify reflux. Duplex ultrasound combines imaging with Doppler to evaluate veins for deep vein thrombosis, reflux, and stenosis by assessing compressibility and flow. Physiologic testing and ultrasound mapping of reflux guides treatment of venous insufficiency.