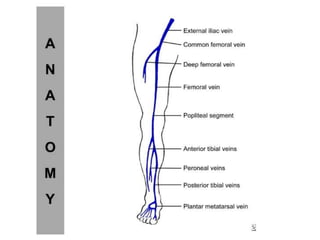
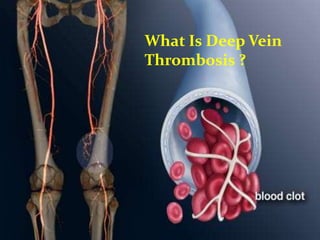
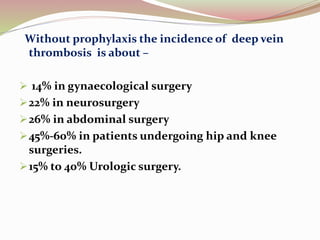
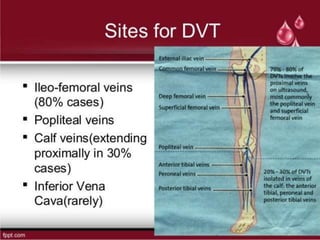
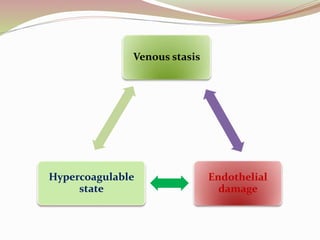
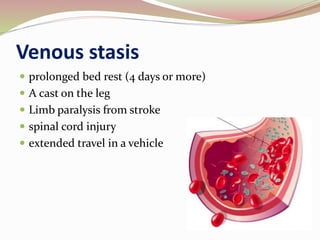
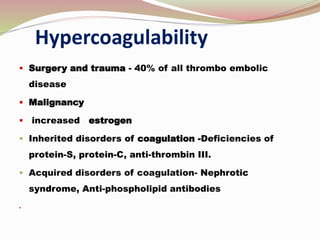
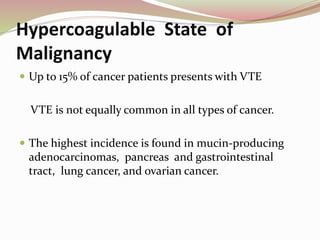
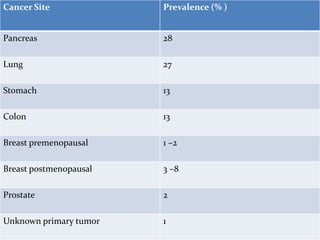
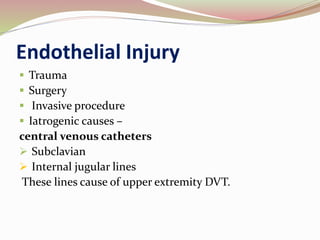
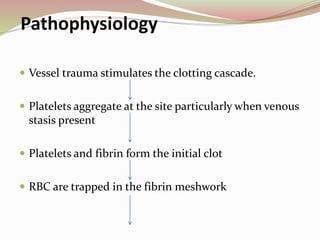
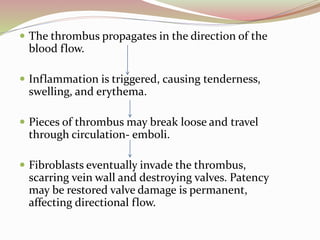
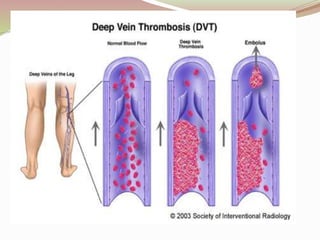
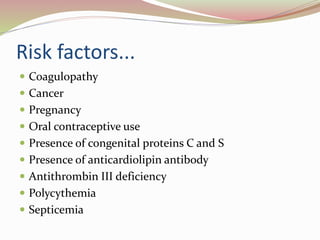
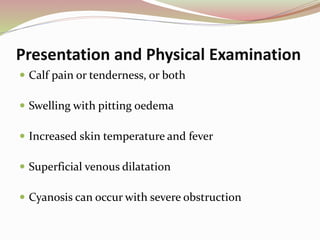
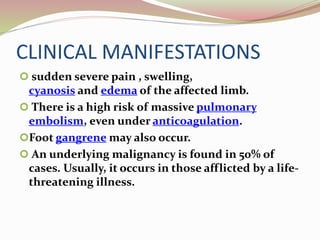
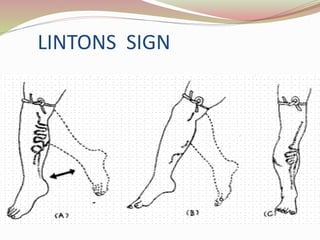
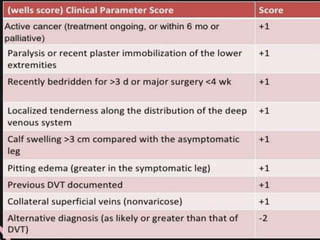
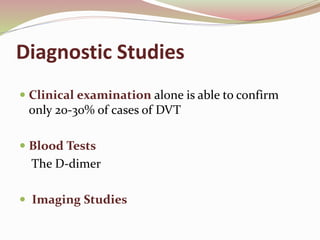
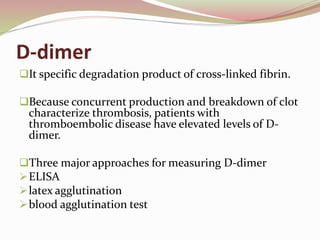
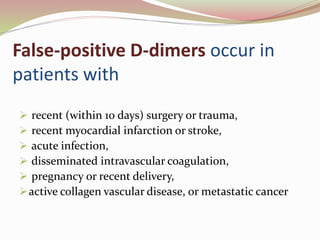
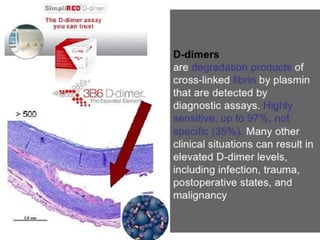
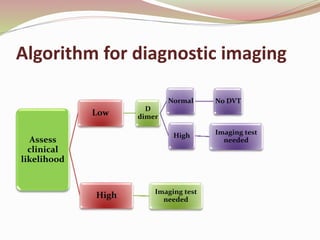
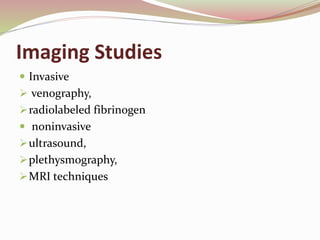
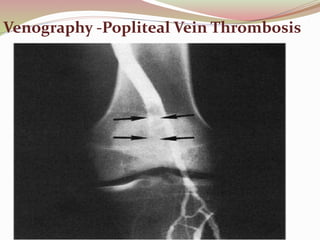
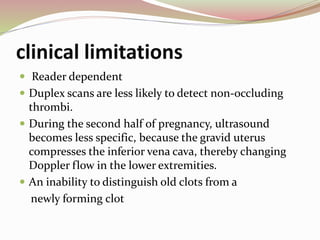
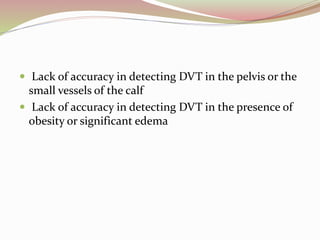
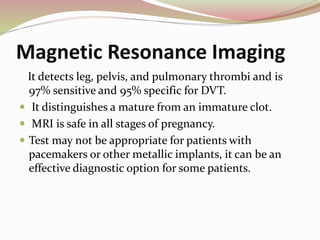
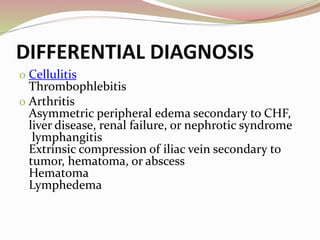
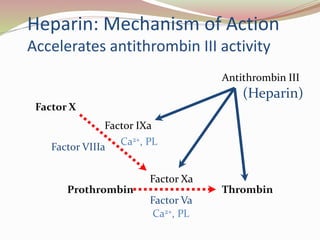
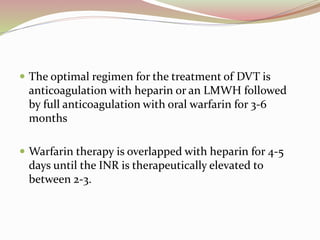
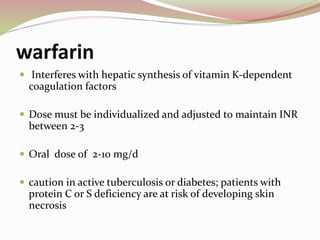
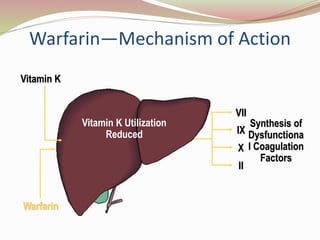
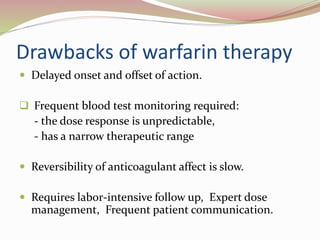
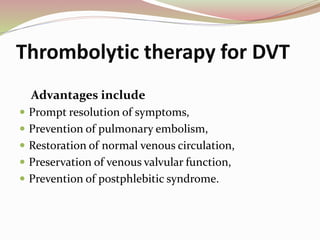
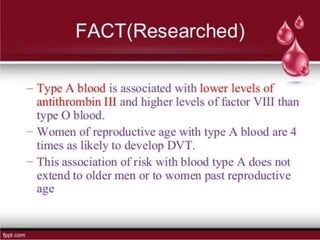
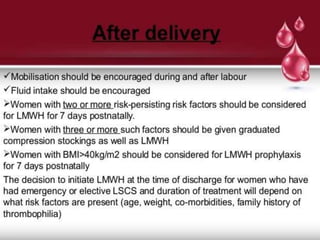
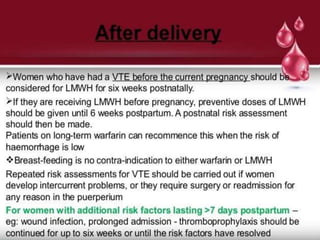
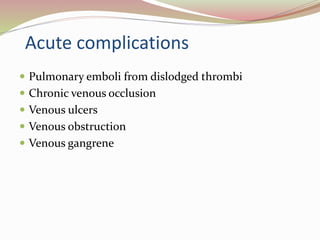
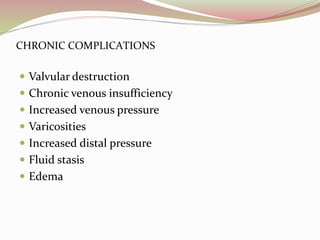
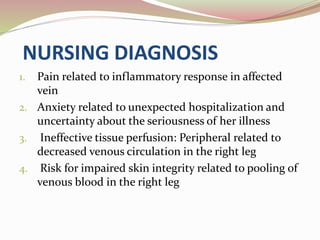
Deep vein thrombosis is a blood clot that forms in the deep veins, usually of the legs. It can dislodge and travel to the lungs, causing a pulmonary embolism. Risk factors include surgery, trauma, cancer, and prolonged immobility. Symptoms may include leg pain, swelling, redness, and warmth. Diagnosis involves assessing risk factors and testing such as ultrasound, venography, MRI, or D-dimer blood test. Treatment focuses on blood thinners to prevent clot growth and embolism.