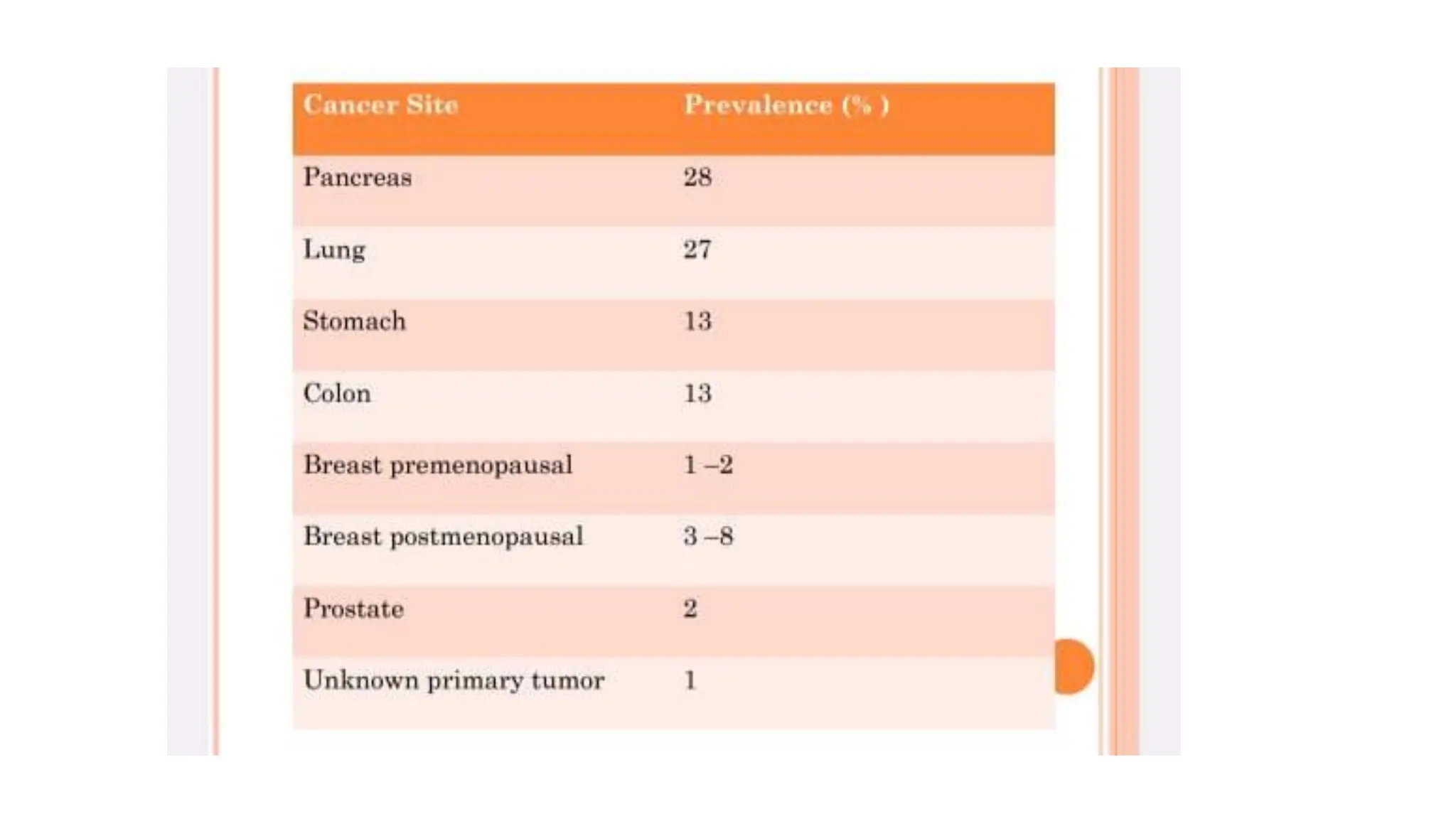
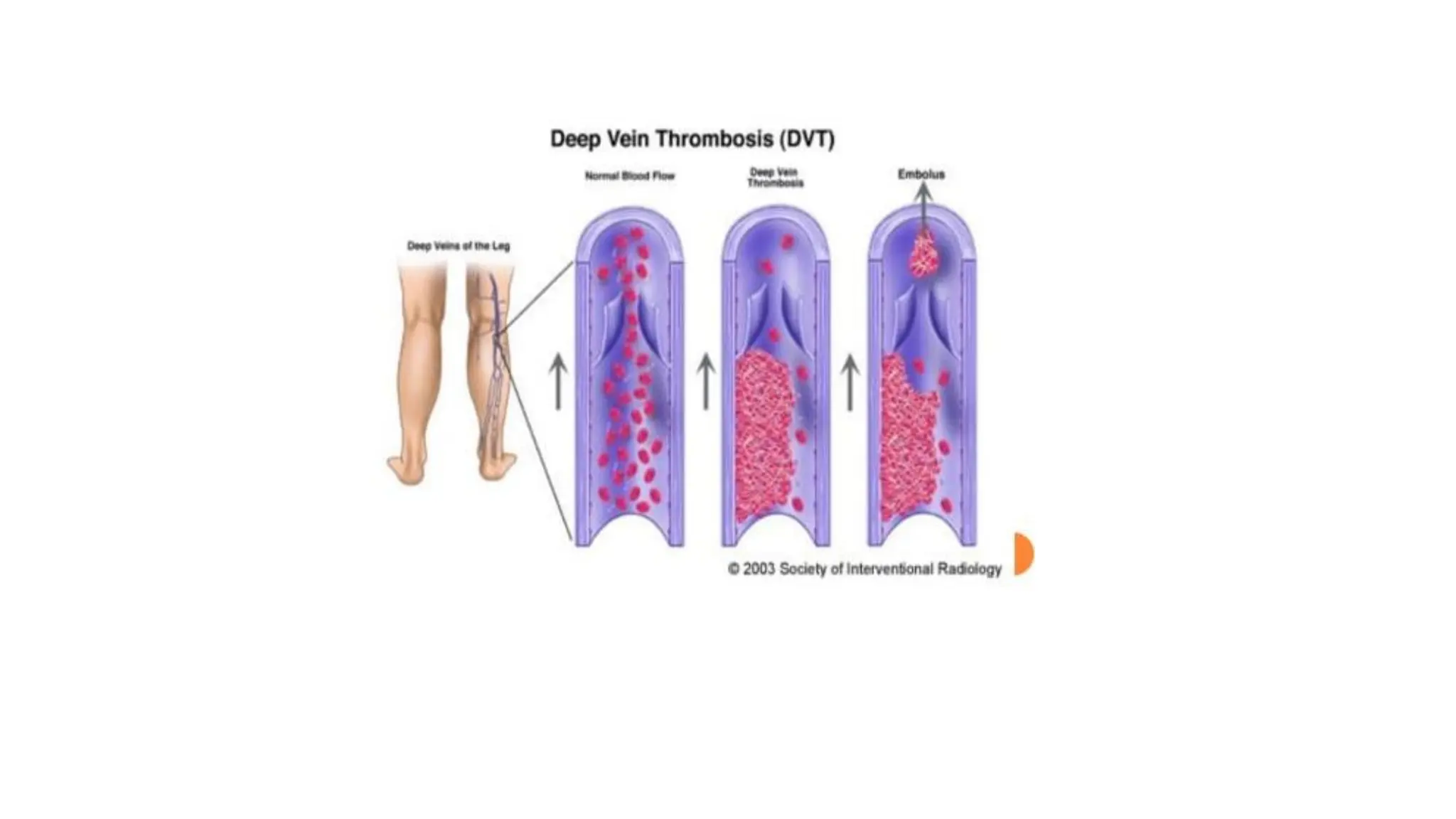
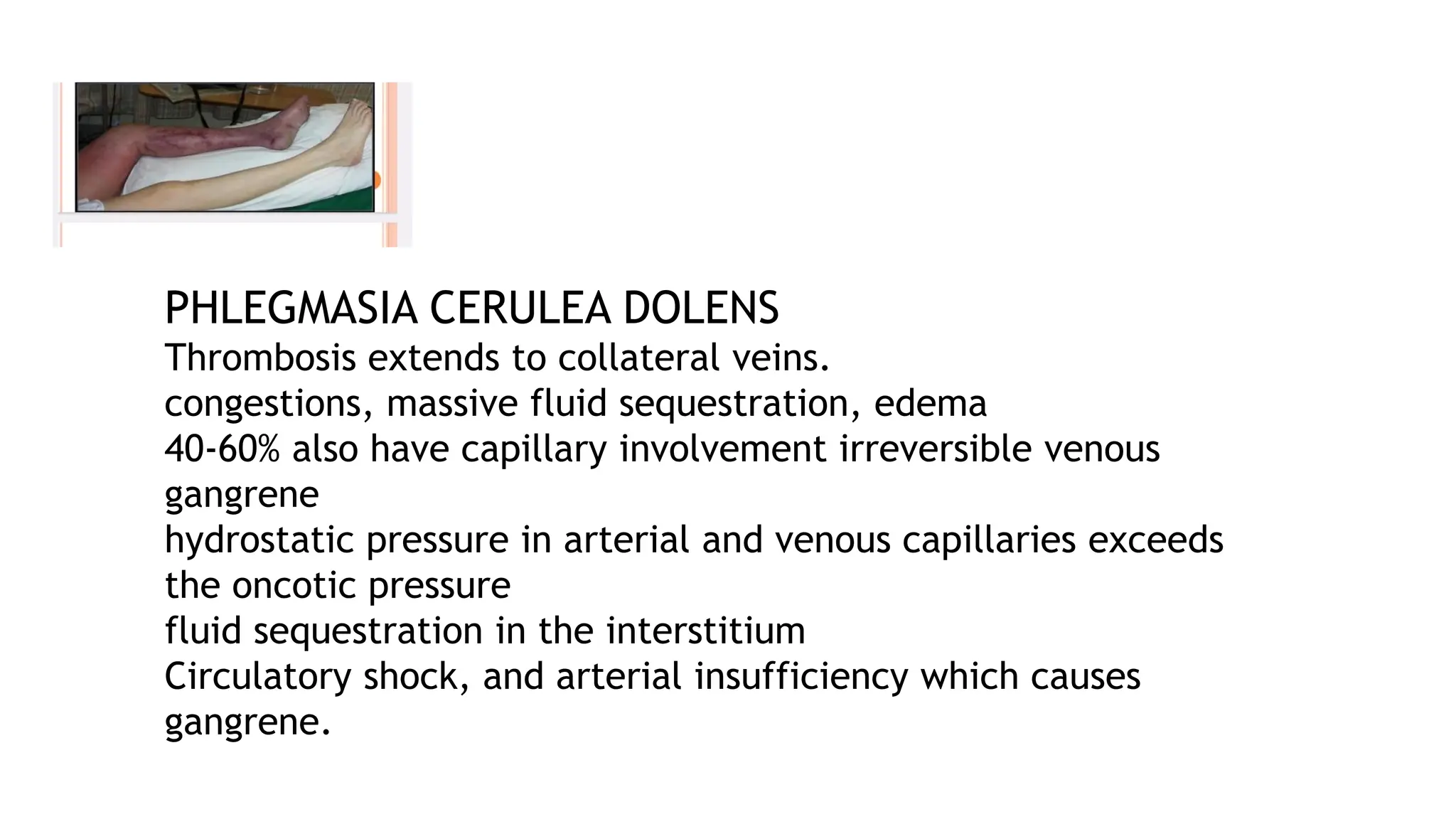
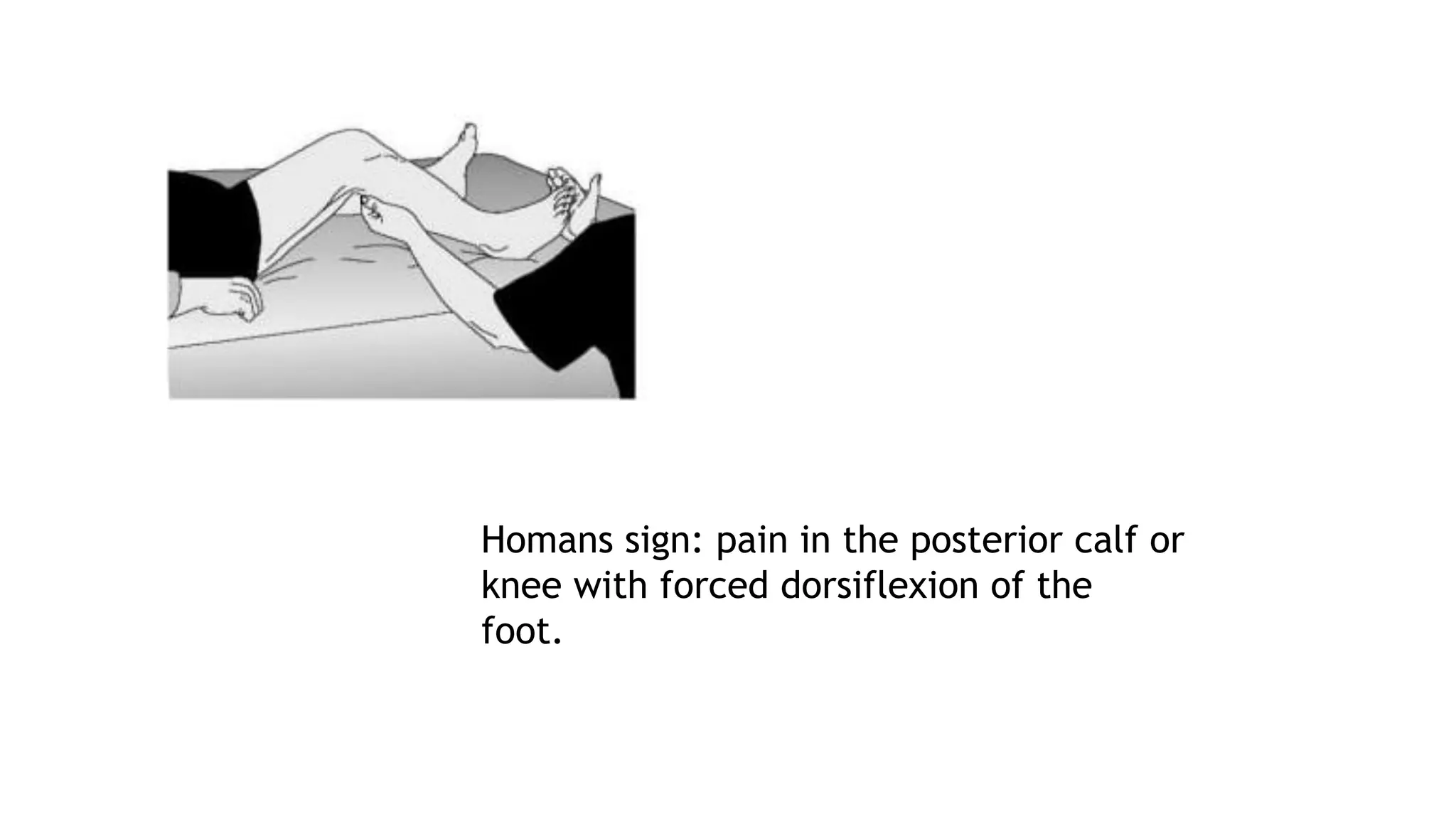
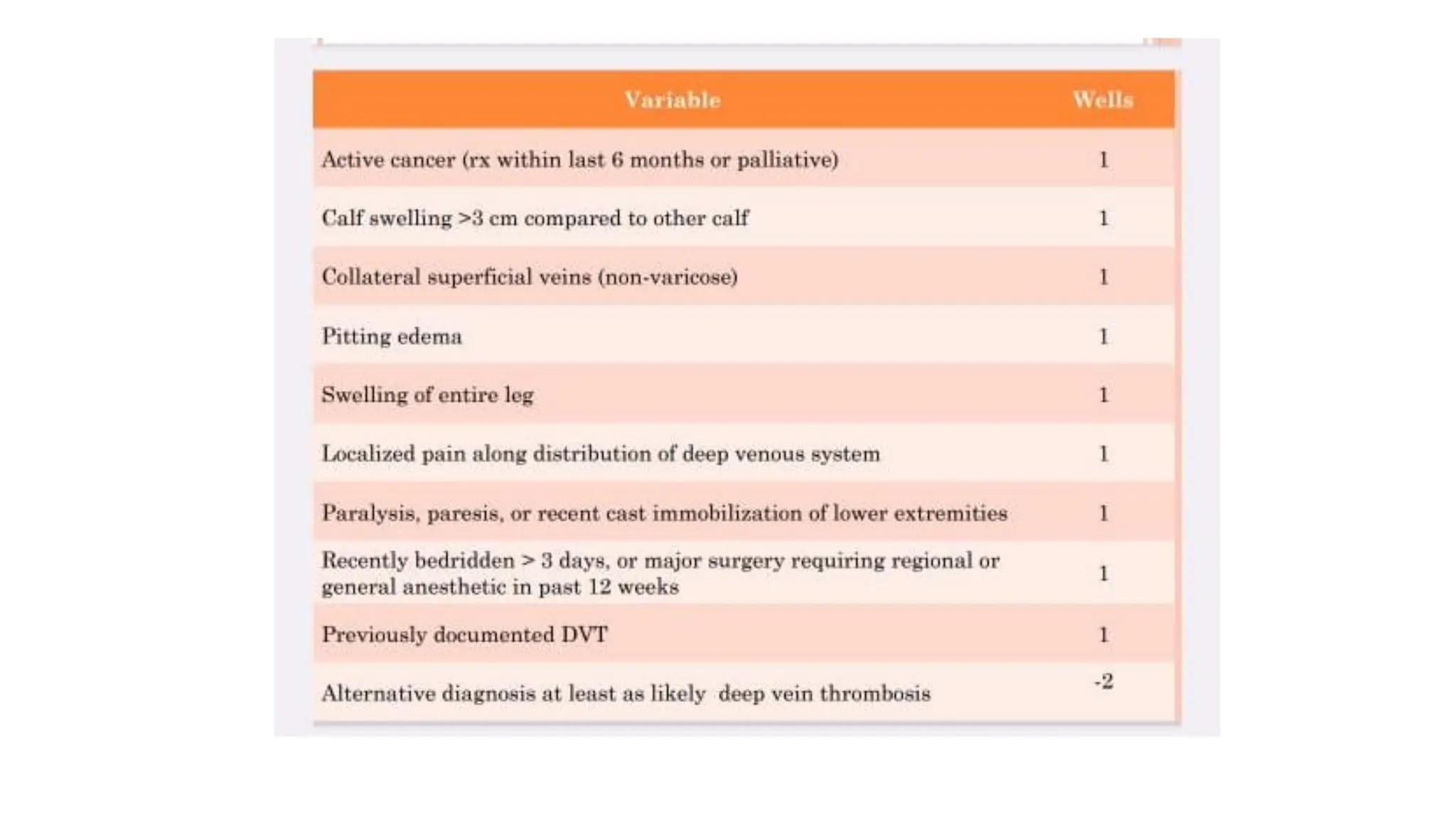
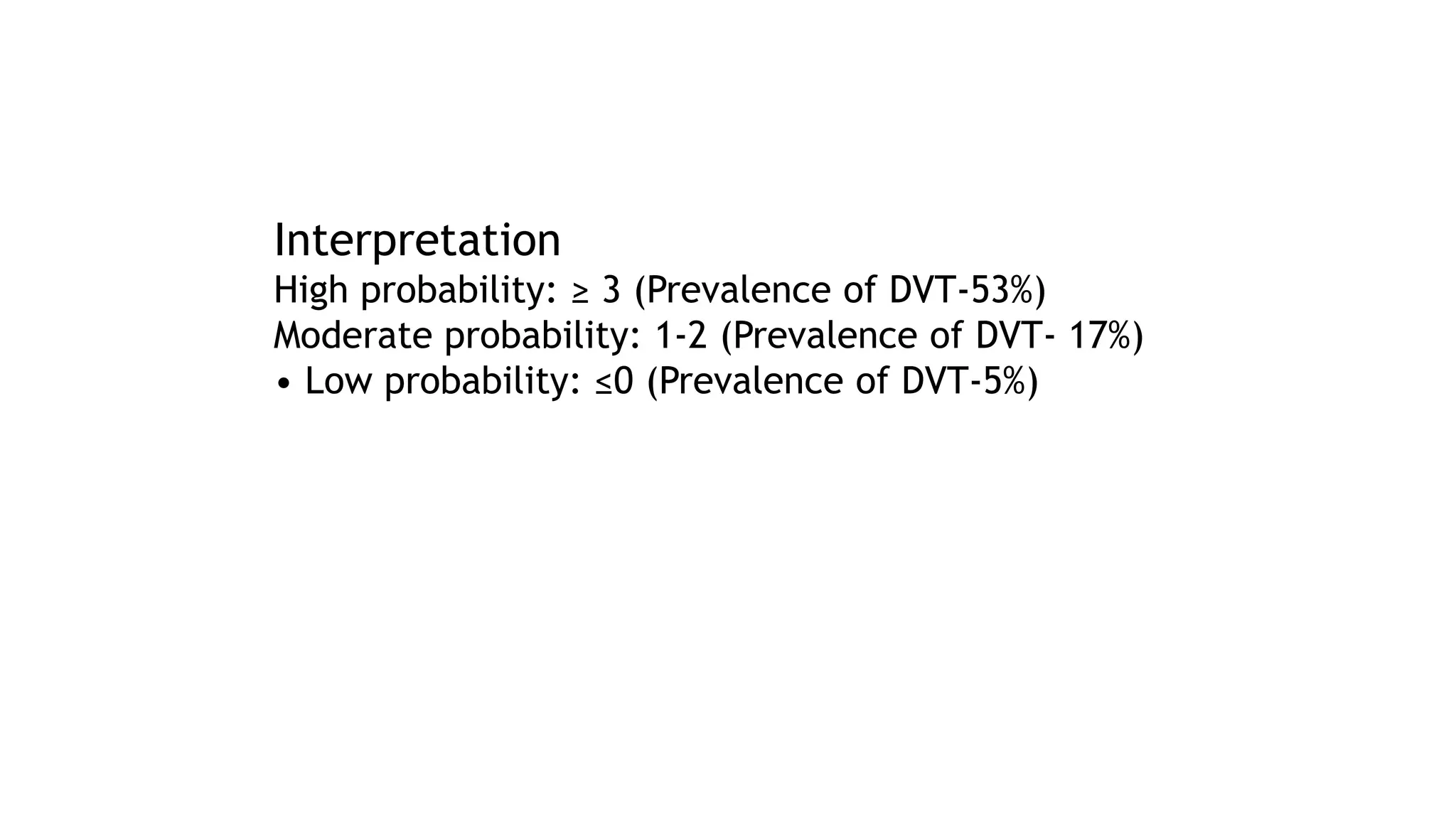
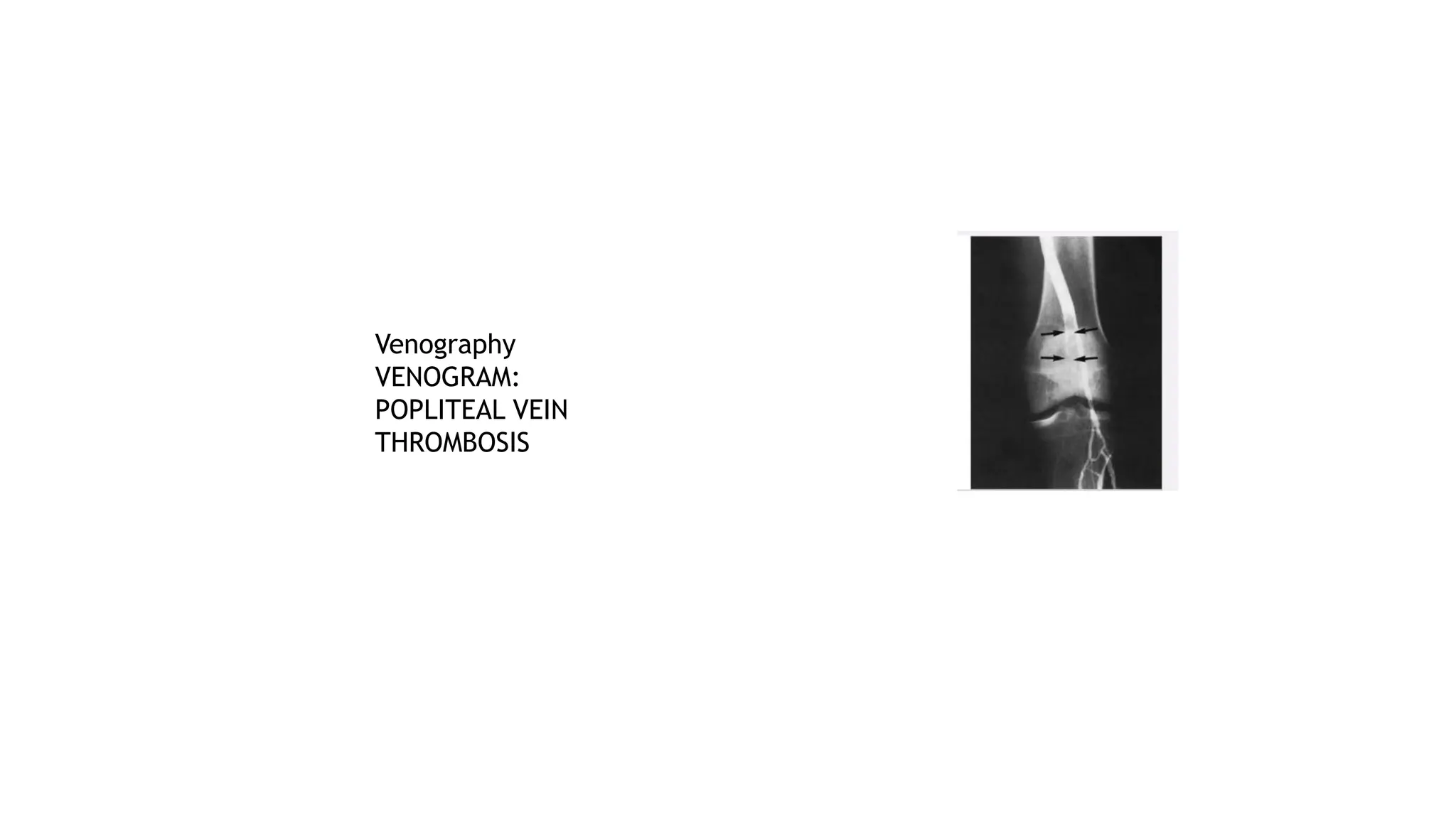
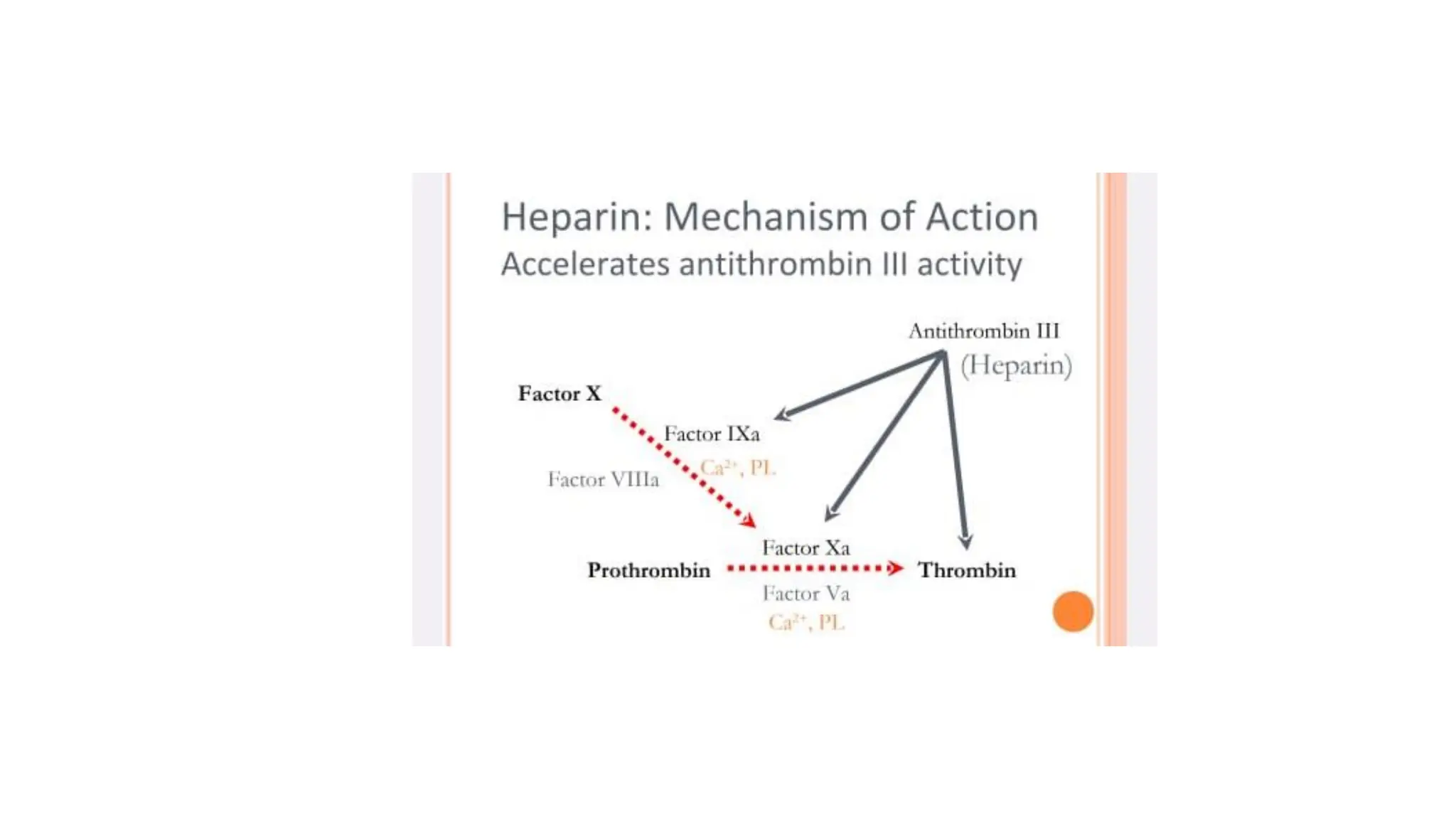
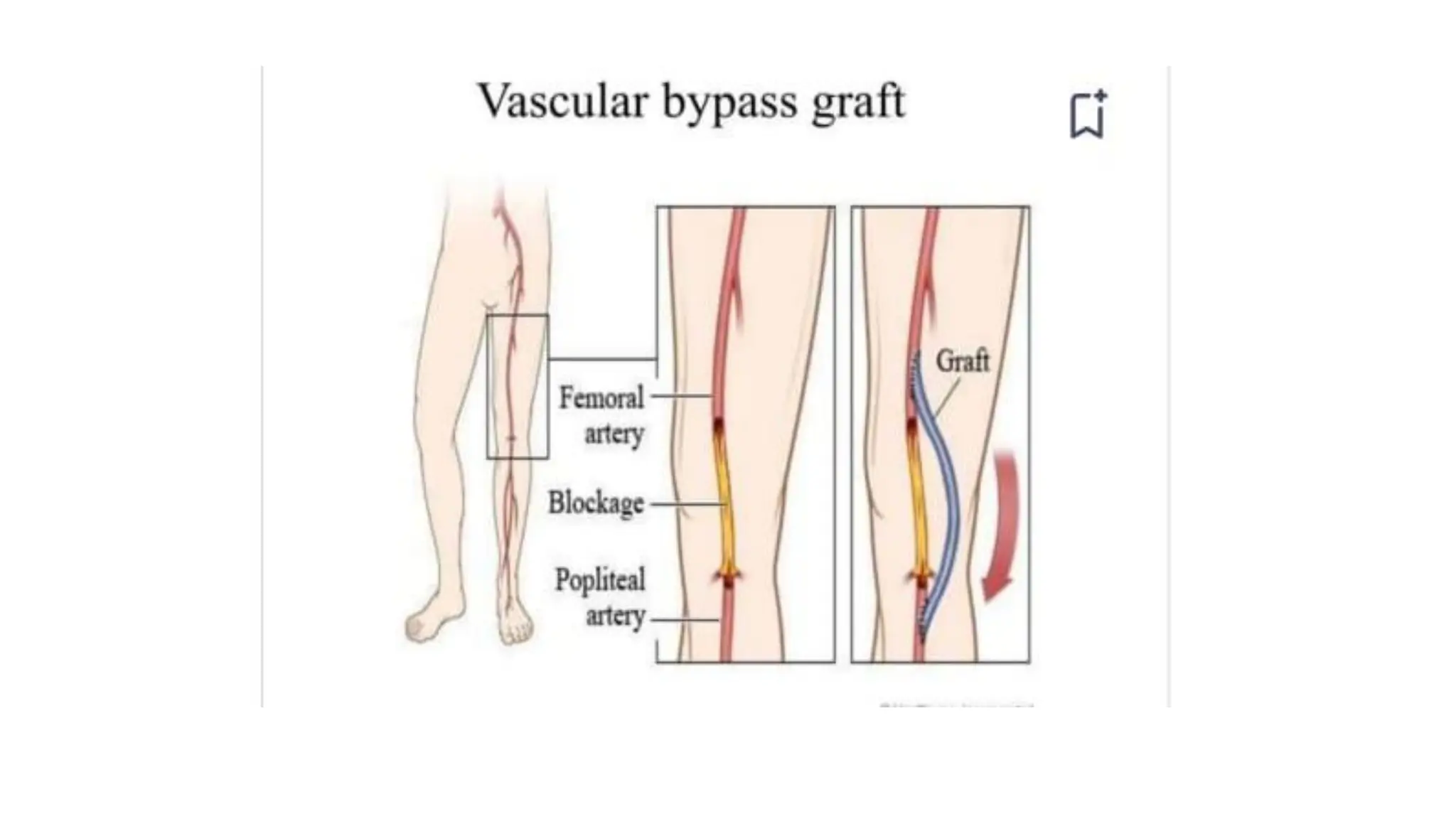
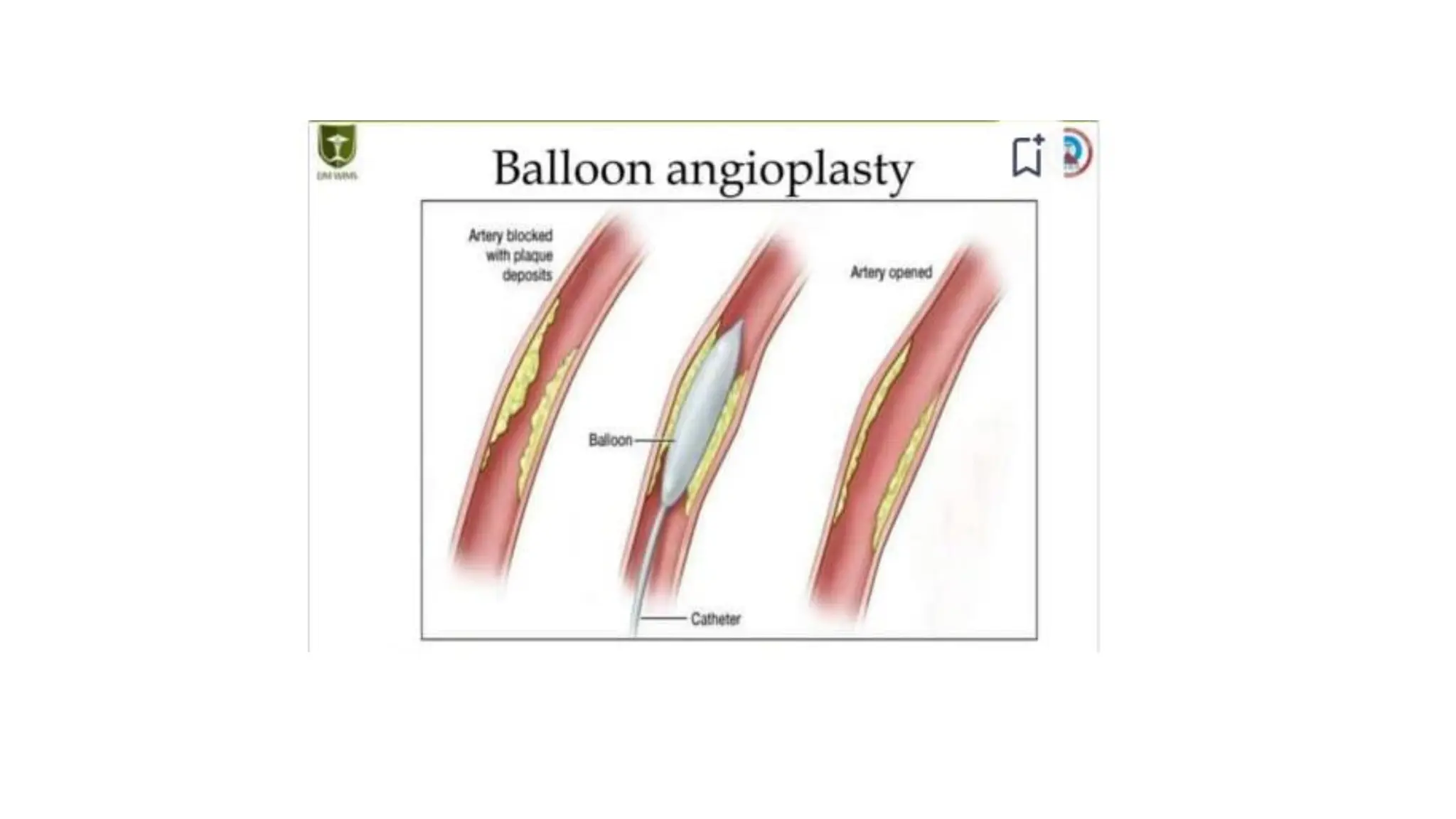
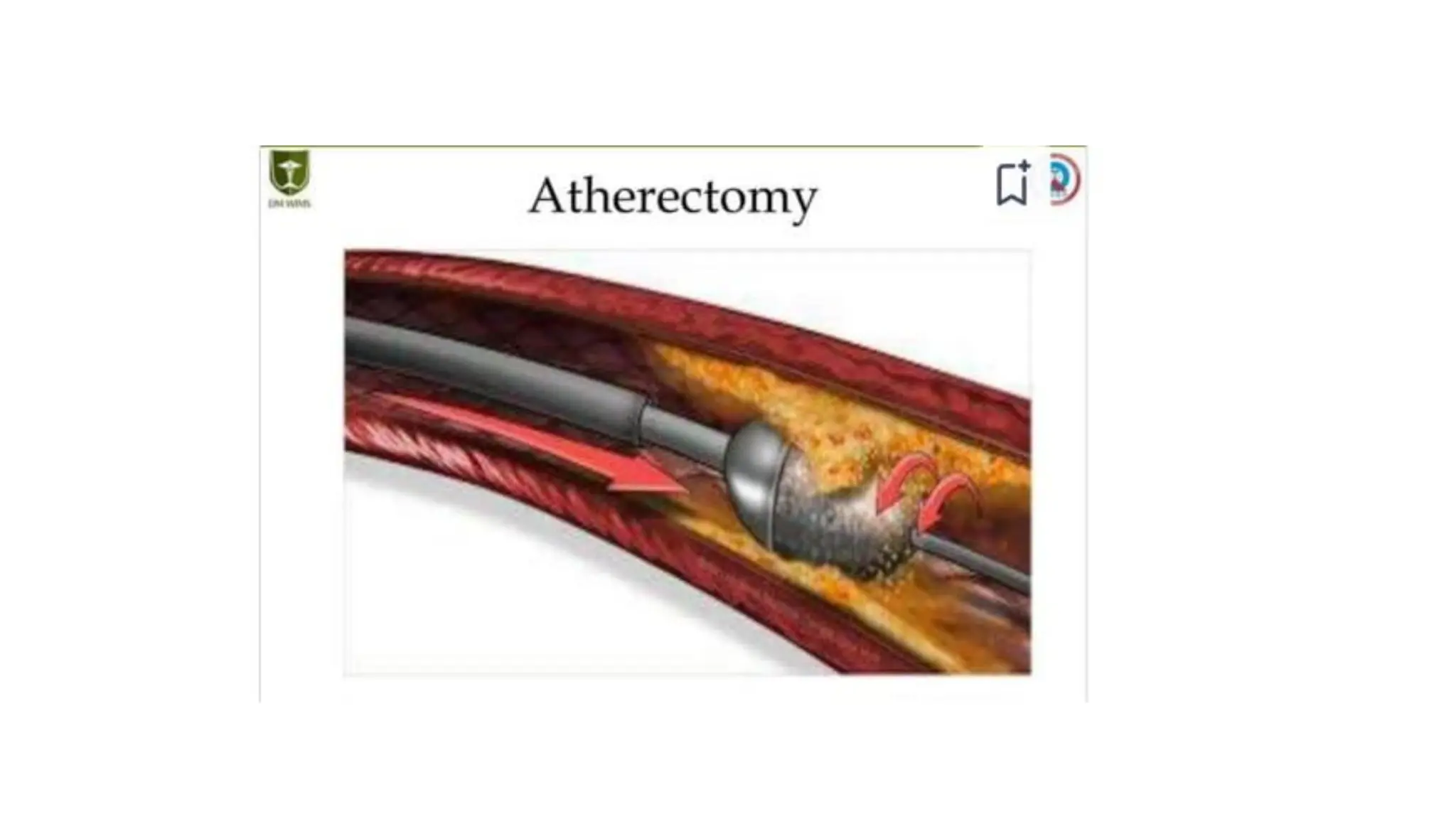
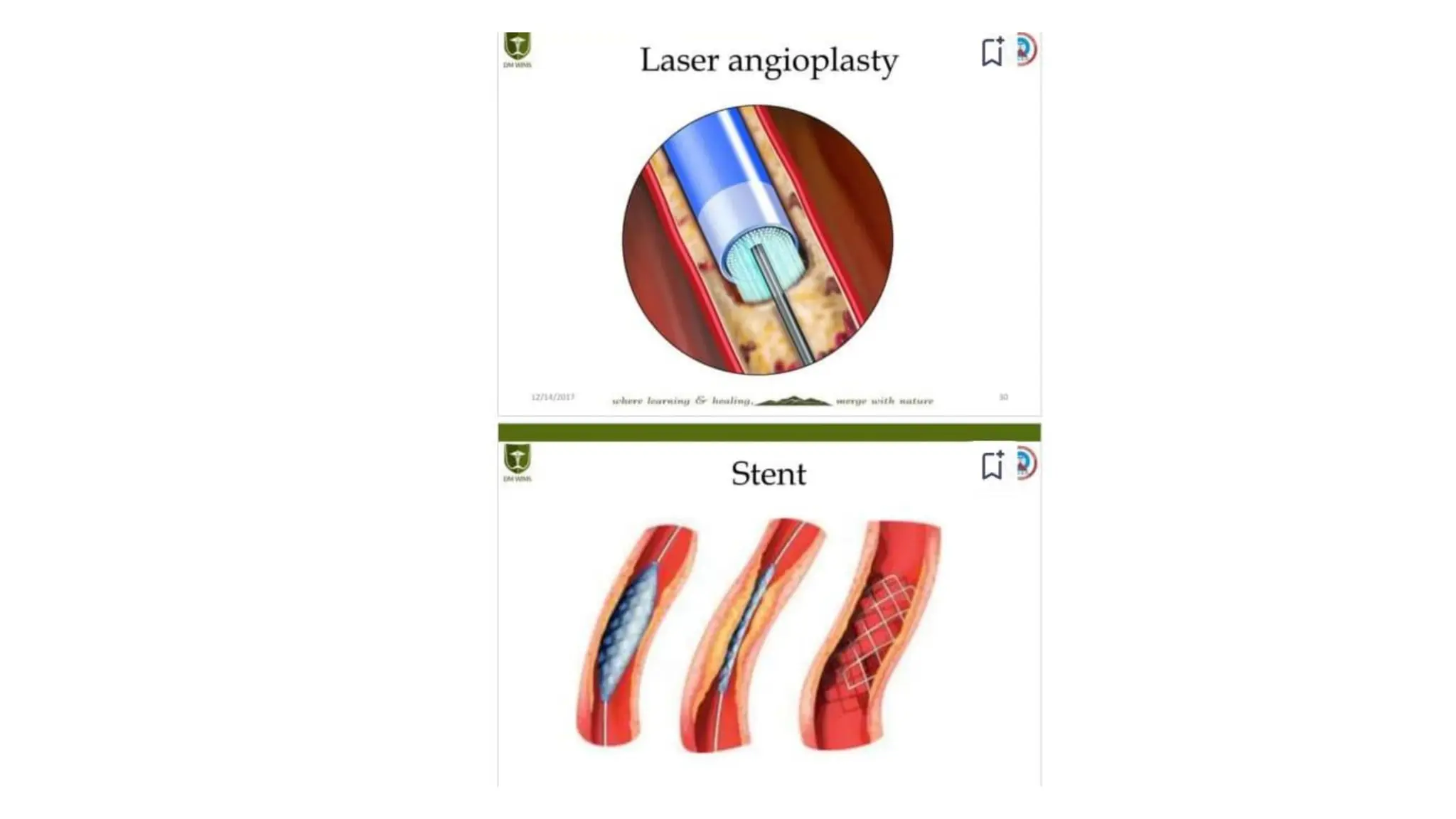
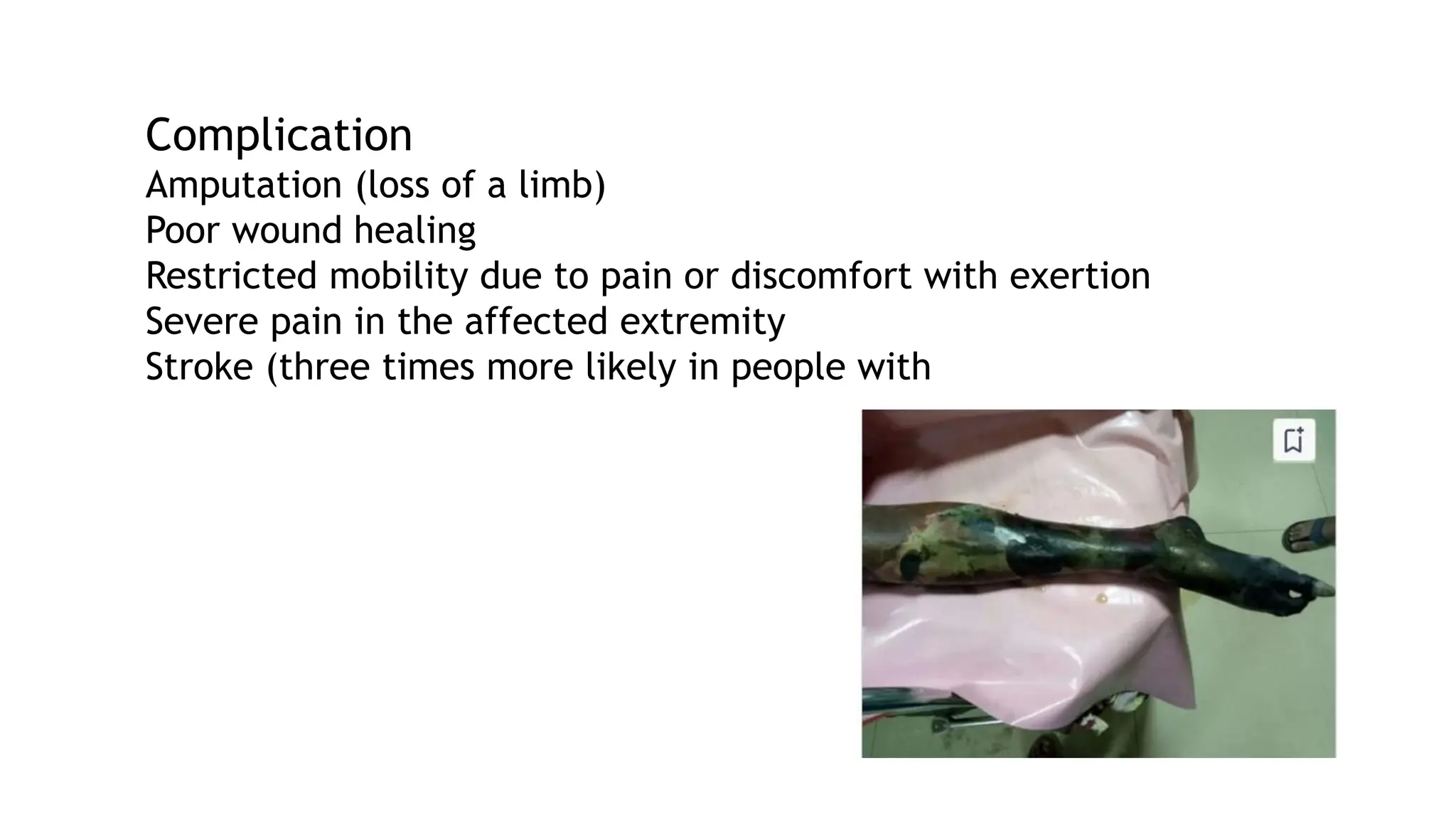
Deep vein thrombosis (DVT) is a condition characterized by the formation of a blood clot in deep veins, primarily in the legs, influenced by factors like venous stasis, hypercoagulable states, and endothelial damage. Symptoms include calf pain, swelling, and potential severe complications like pulmonary embolism and gangrene. Diagnosis involves clinical evaluation, D-dimer tests, and imaging, with treatment focusing on anticoagulation, thrombolytic therapy, and prevention of recurrence.