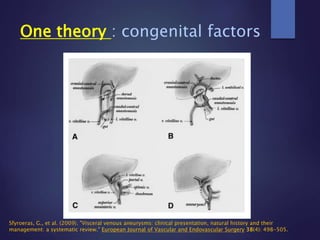
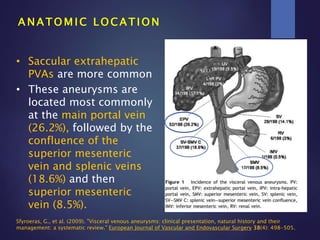
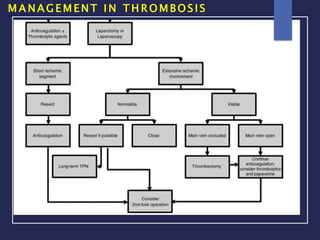
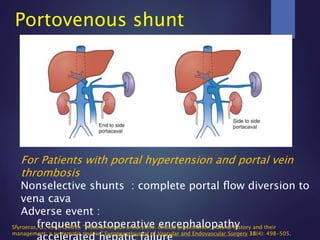
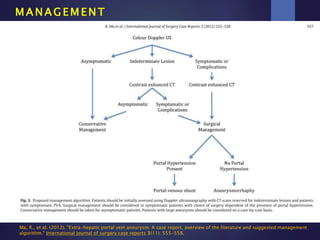
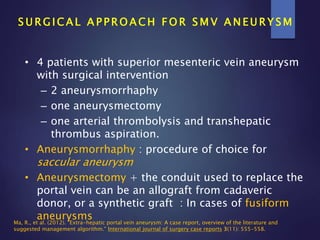
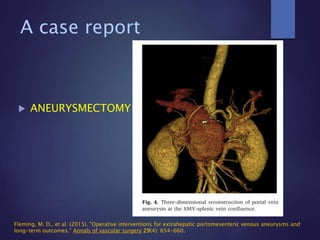
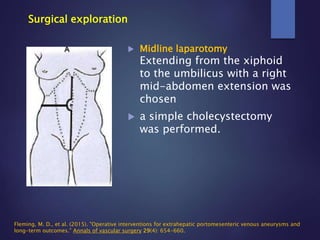
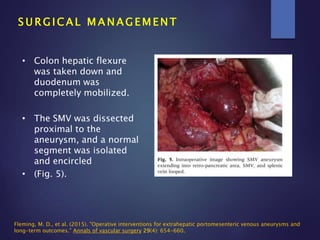
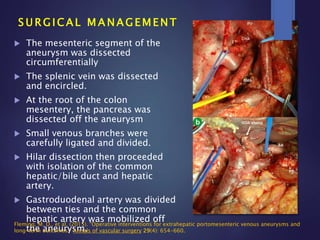
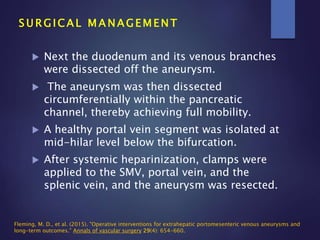
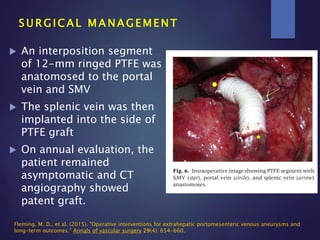
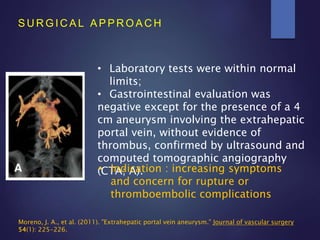
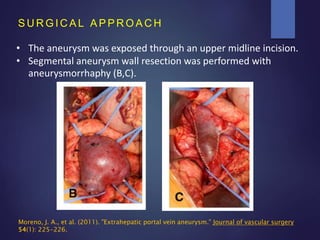
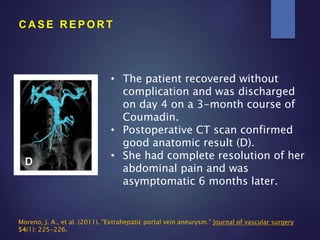
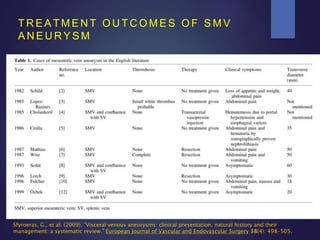
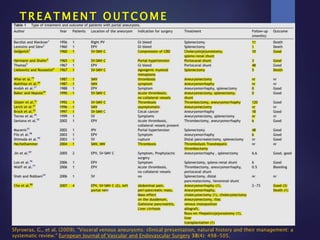
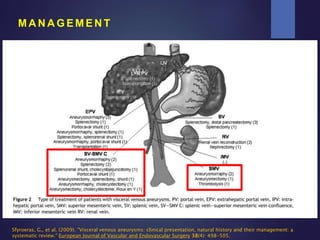
This document describes the case of a 74-year-old Thai female with a known superior mesenteric vein (SMV) aneurysm. She presented with abdominal discomfort for one month. On examination, her abdomen was moderately distended with mild tenderness in the suprapubic region. The document then reviews definitions, etiology, clinical presentation, complications, and management approaches for SMV aneurysms. It discusses that surgical intervention is usually indicated for symptomatic or expanding aneurysms. Options include aneurysmorrhaphy or aneurysmectomy. For this patient, proper management would involve surgical resection of the aneurysm.