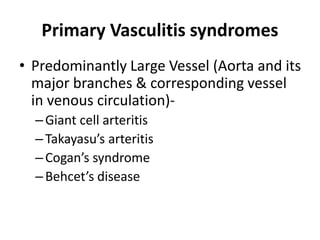
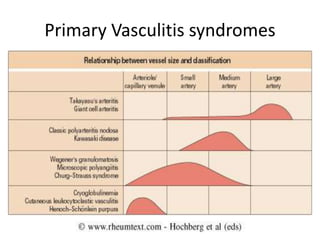
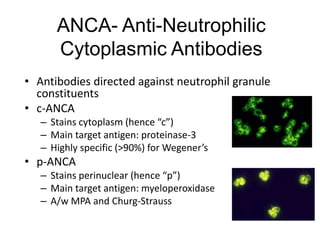
This document discusses vasculitis, including its classification, symptoms, and mimickers. Vasculitis is characterized by inflammation of blood vessels that can lead to ischemia. It is classified as either primary, where vasculitis is the principal feature, or secondary, where it is associated with another condition. Primary vasculitis is further divided based on vessel size affected. Symptoms depend on the vessel size involved and can include limb pain, rashes, organ dysfunction. Secondary causes include drugs, infections like hepatitis, and rheumatologic diseases. The document outlines features of different types and emphasizes vasculitis must be differentiated from conditions that can mimic its presentation.