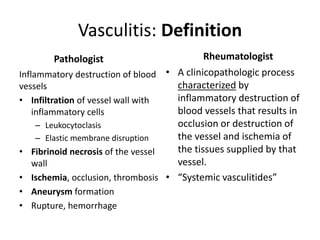
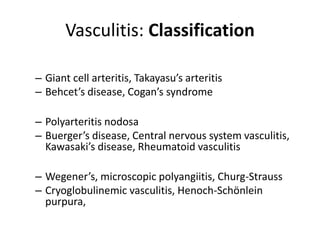
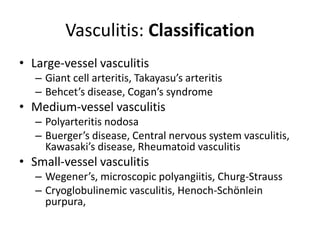
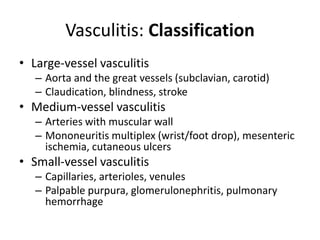
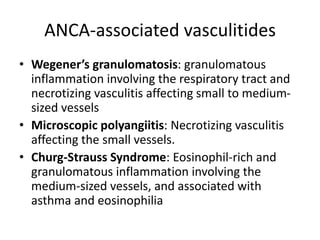
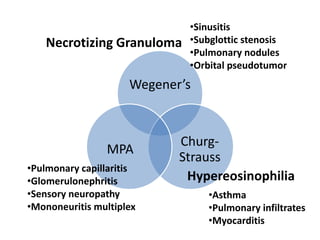
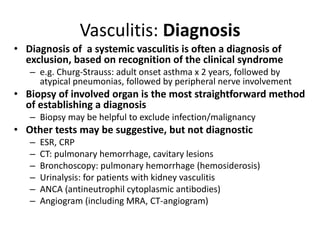
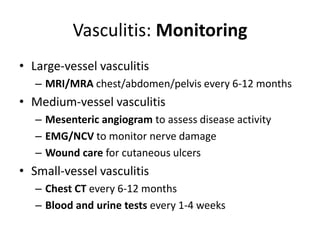
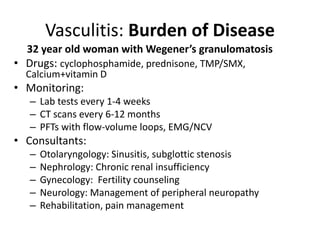
Vasculitis refers to inflammation of blood vessels. It affects people of all ages and can be chronic and relapsing in nature. Vasculitis is classified based on the size of blood vessels involved, such as large, medium, or small vessels. Diagnosis involves ruling out other conditions through biopsies and tests. Treatment aims to induce remission through immunosuppressants, while monitoring focuses on preventing damage to organs. Even in remission, patients commonly experience pain, fatigue, and long-term consequences from both the disease and its treatments.
![• Remission induction:
– Cyclophosphamide 2mg/kg po qd x 3-6 months
[or 15 mg/kg IV q 2 wk x3 then q 3 weeks x 6-12 months]
– Prednisone 1mg/kg po qd x 1 month, then taper
– [Bactrim, Calcium, Vitamin D]
• Remission maintenance (minimum 2 years)
– Methotrexate 20-25 mg po q week + folate
– Azathioprine 2mg/kg po qd
– Mycophenolate mofetil 1.5 g po BID
– Leflunomide 20-30 mg po BID
Vasculitis: Treatment](https://image.slidesharecdn.com/vasculitis-220907105235-b14c5f15/85/vasculitis-pptx-10-320.jpg)
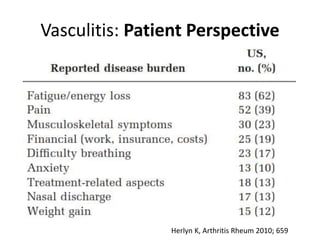
![Vasculitis: Patient Perspective
Pain
Disease-Specific
• Sensory neuropathy
• Cutaneous ulcerations
• Arm claudication
Non-specific
• [Arthritis]
• Vertebral fracture
Fatigue
Vasculitis-induced
• Loss of proprioception
Glucocorticoid-induced
• Muscle loss, Weight gain
• Emotional liability
Immunosuppression-induced
• Cognitive impairment
• Drug-associated fatigue](https://image.slidesharecdn.com/vasculitis-220907105235-b14c5f15/85/vasculitis-pptx-19-320.jpg)