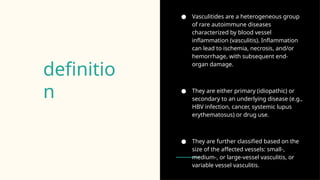
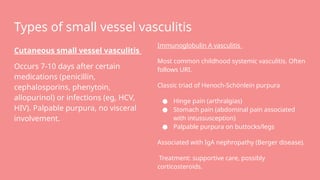
Vasculitides are rare autoimmune diseases characterized by inflammation of blood vessels, leading to potential organ damage and classified by vessel size. The document details large-, medium-, and small-vessel vasculitis, including specific conditions like giant cell arteritis, Takayasu arteritis, Kawasaki disease, and polyarteritis nodosa, along with their epidemiology, clinical features, and management strategies. Treatment generally includes glucocorticoids and immunosuppressants, with specific therapies based on the type and underlying causes.