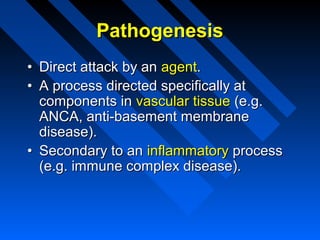
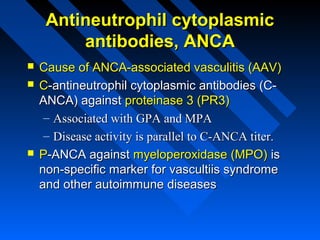
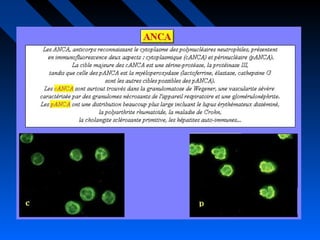
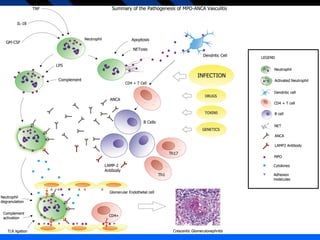
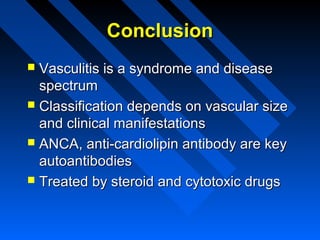
This document provides an overview of vasculitis including:
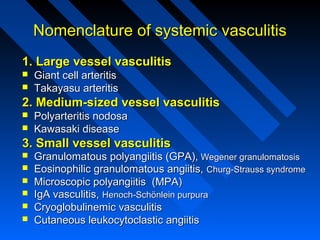
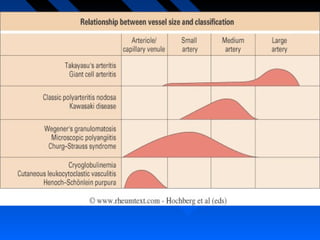
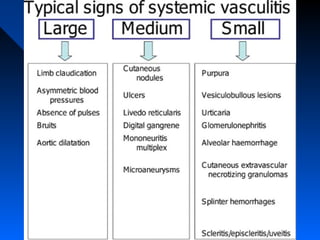
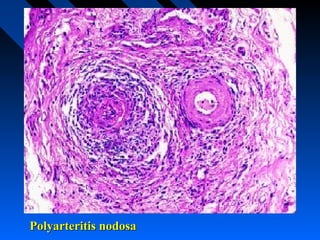
1. It classifies vasculitis based on the size of blood vessels involved - large, medium, or small vessel vasculitis.
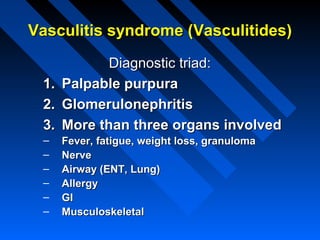
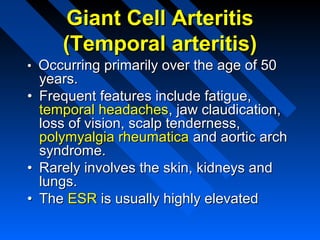
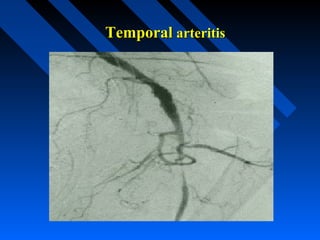
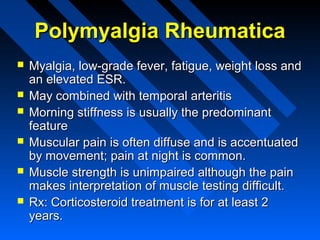
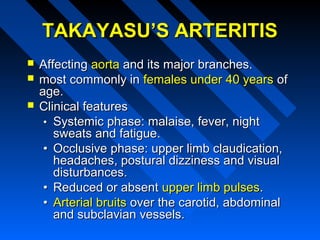
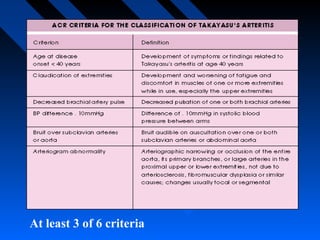
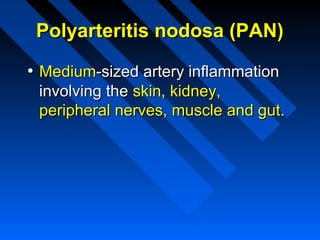
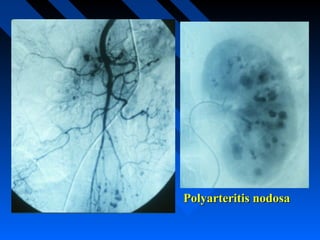
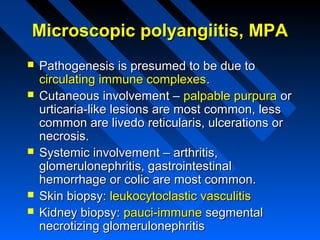
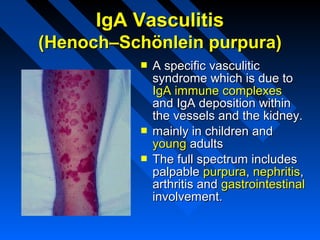
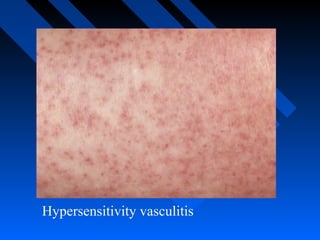
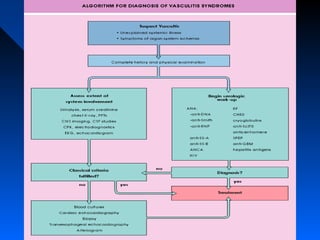
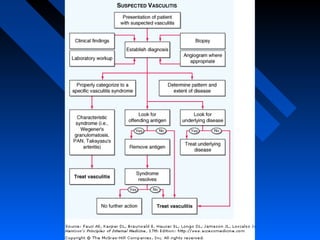
2. It describes several specific types of vasculitis like Takayasu's arteritis, Kawasaki disease, granulomatosis with polyangiitis, and IgA vasculitis.
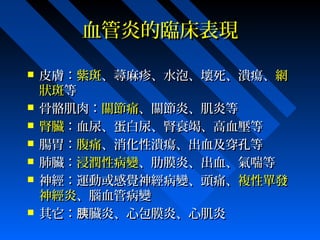
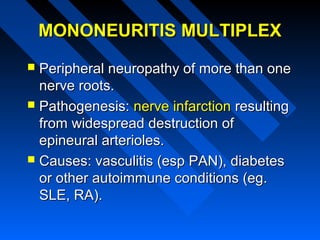
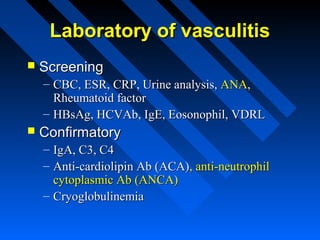
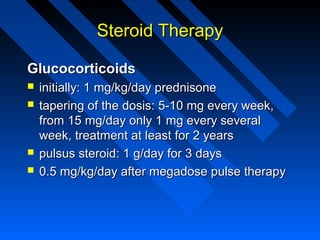
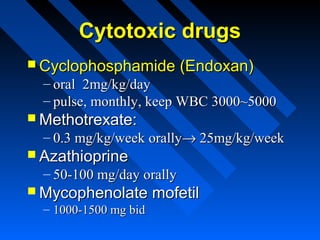
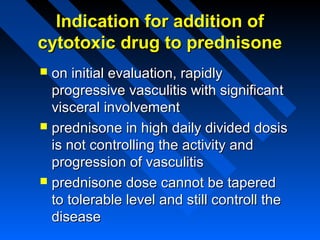
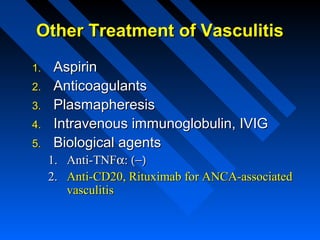
3. Clinical manifestations, diagnosis, and treatment options for vasculitis are discussed with an emphasis on using steroids and cytotoxic drugs to treat vasculitis.