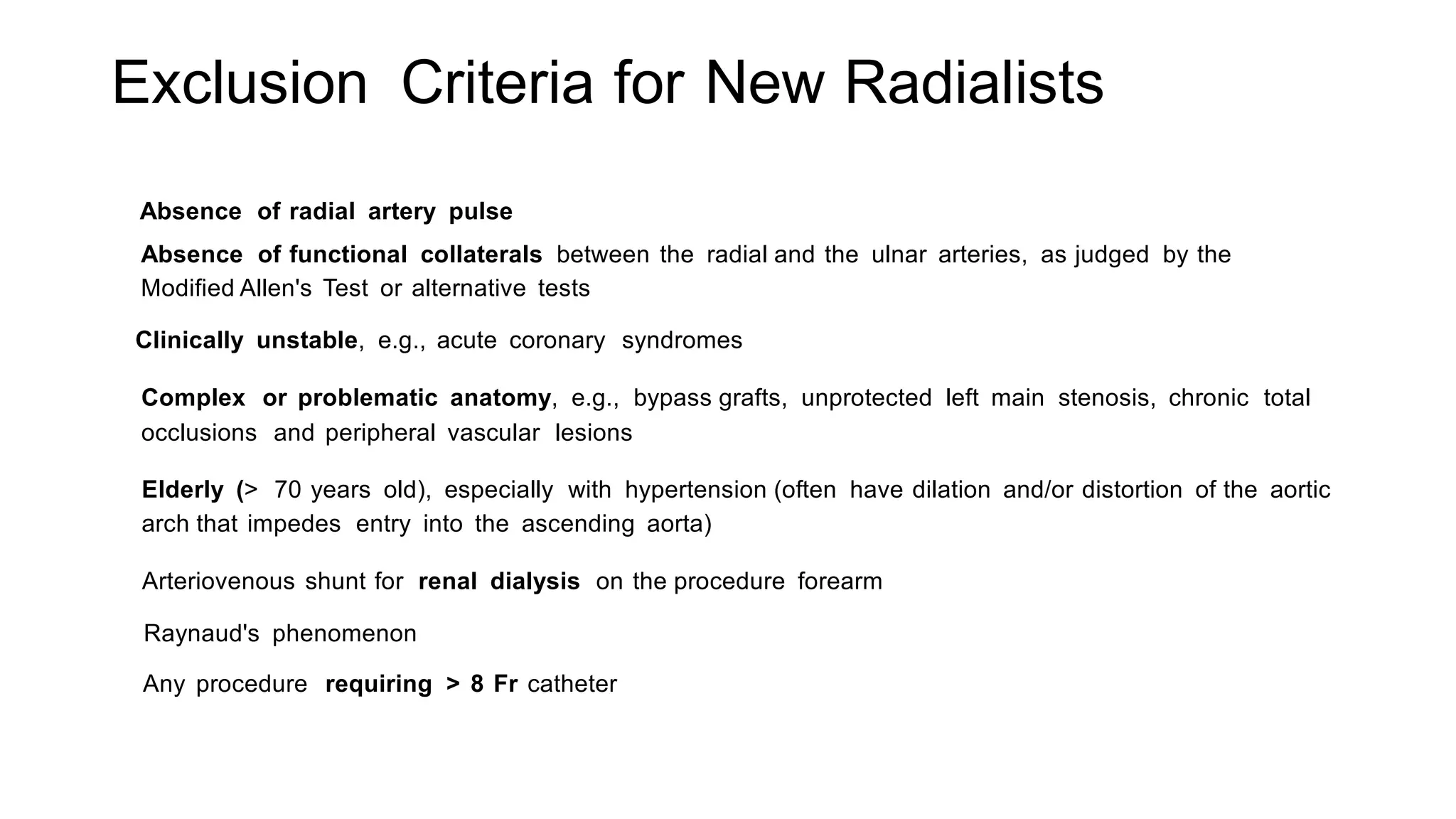
1. Radial artery access is an alternative to femoral artery access for coronary procedures that offers advantages like lower bleeding risks and faster recovery times.
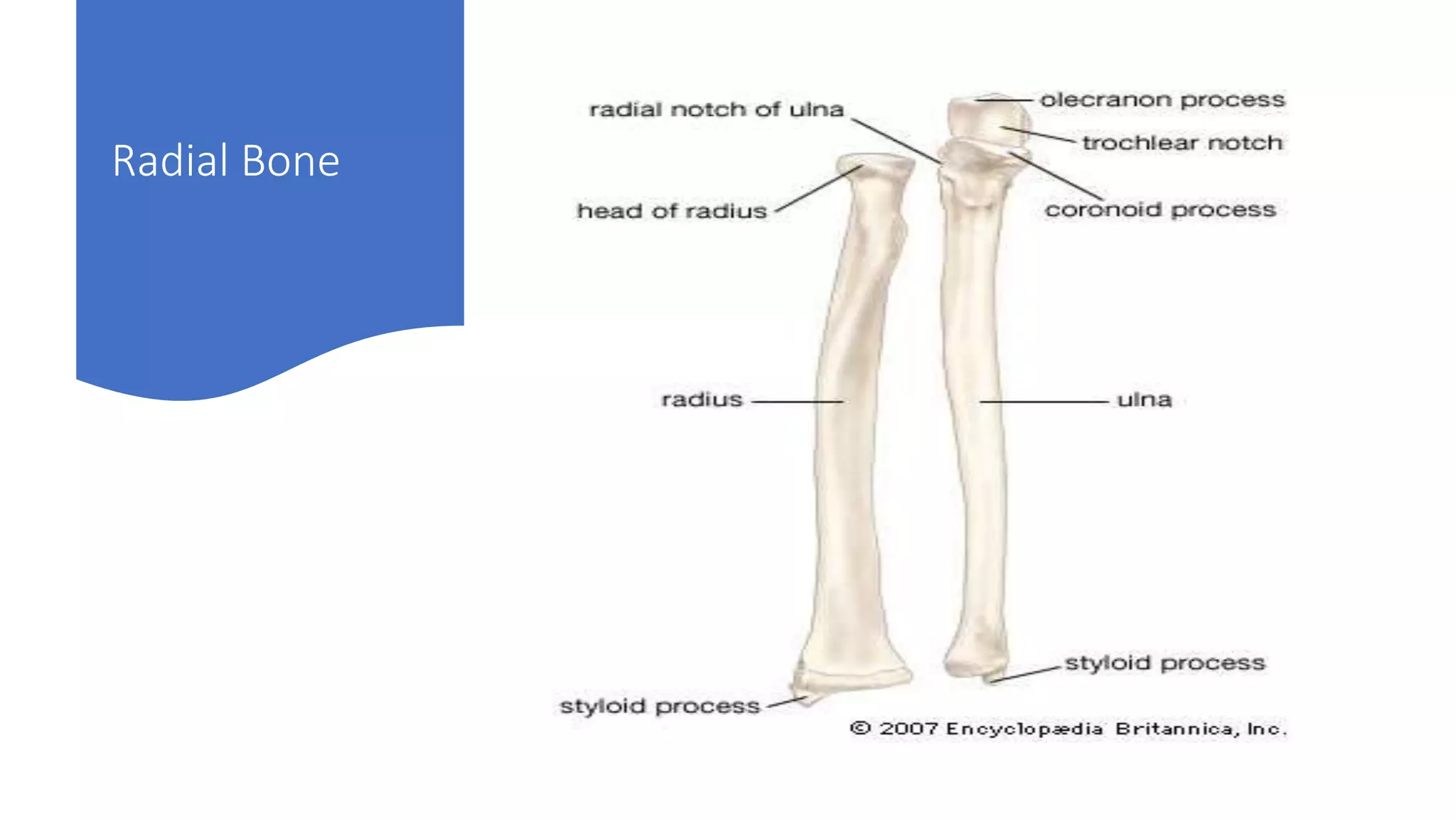
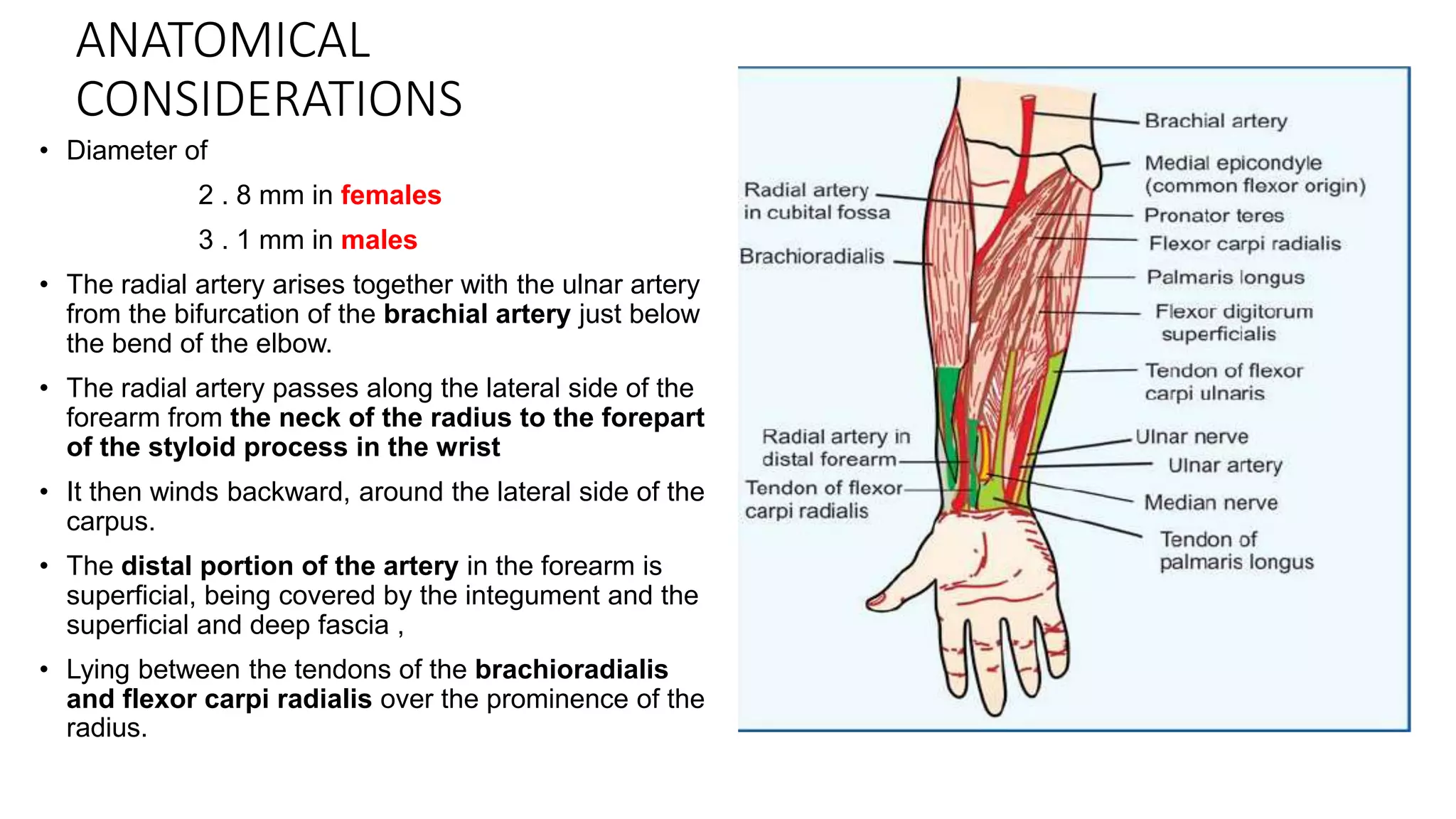
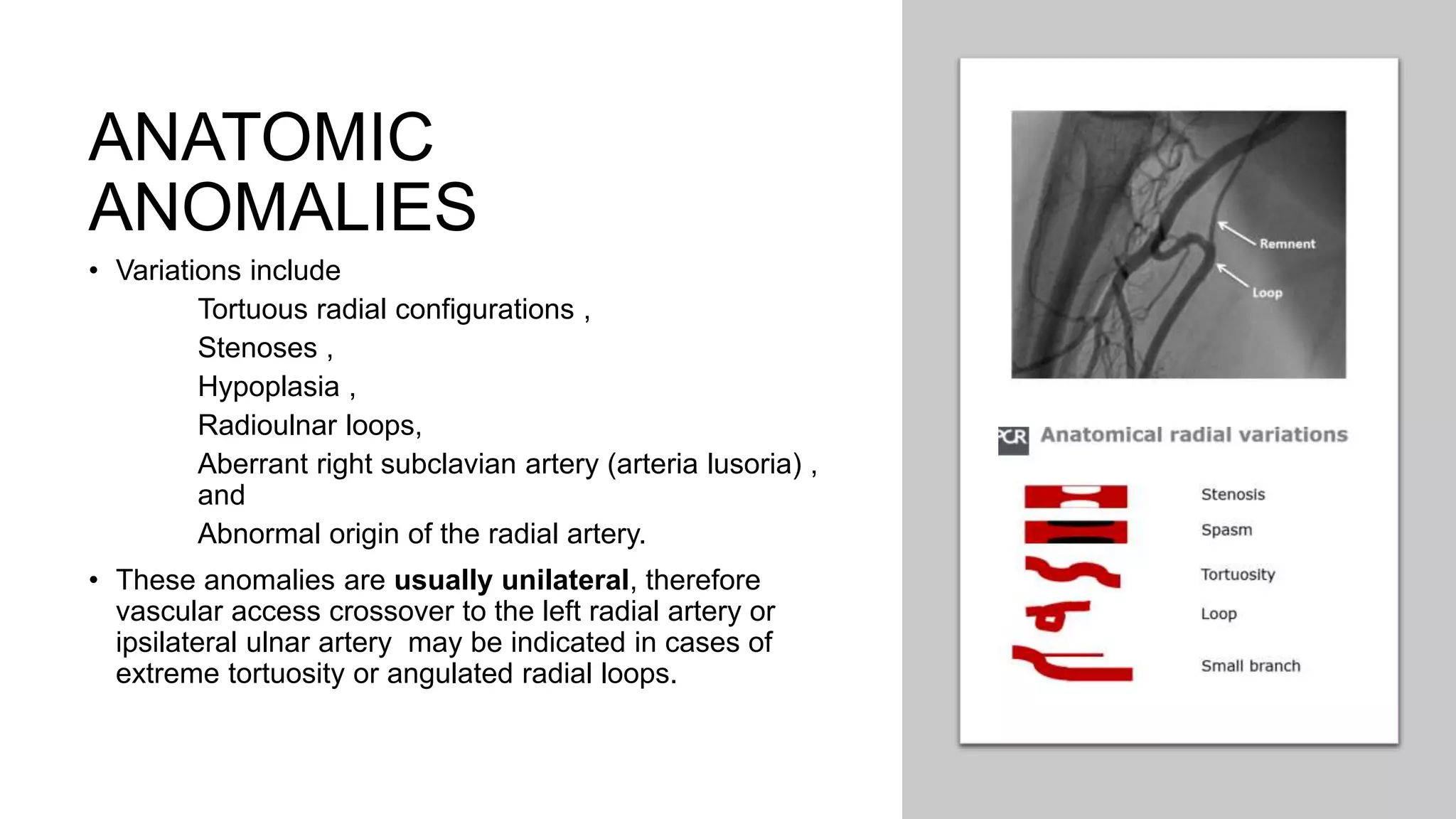
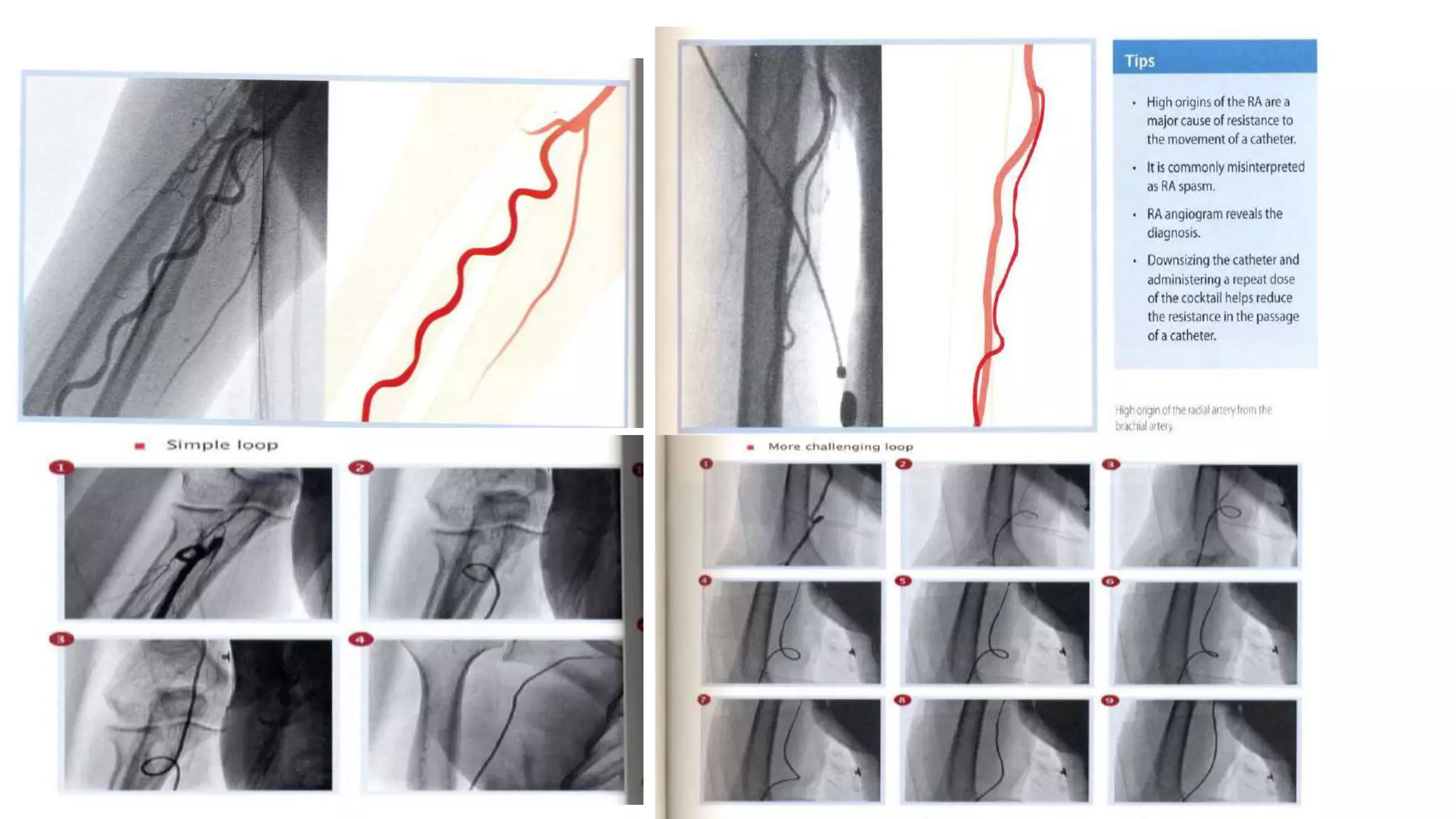
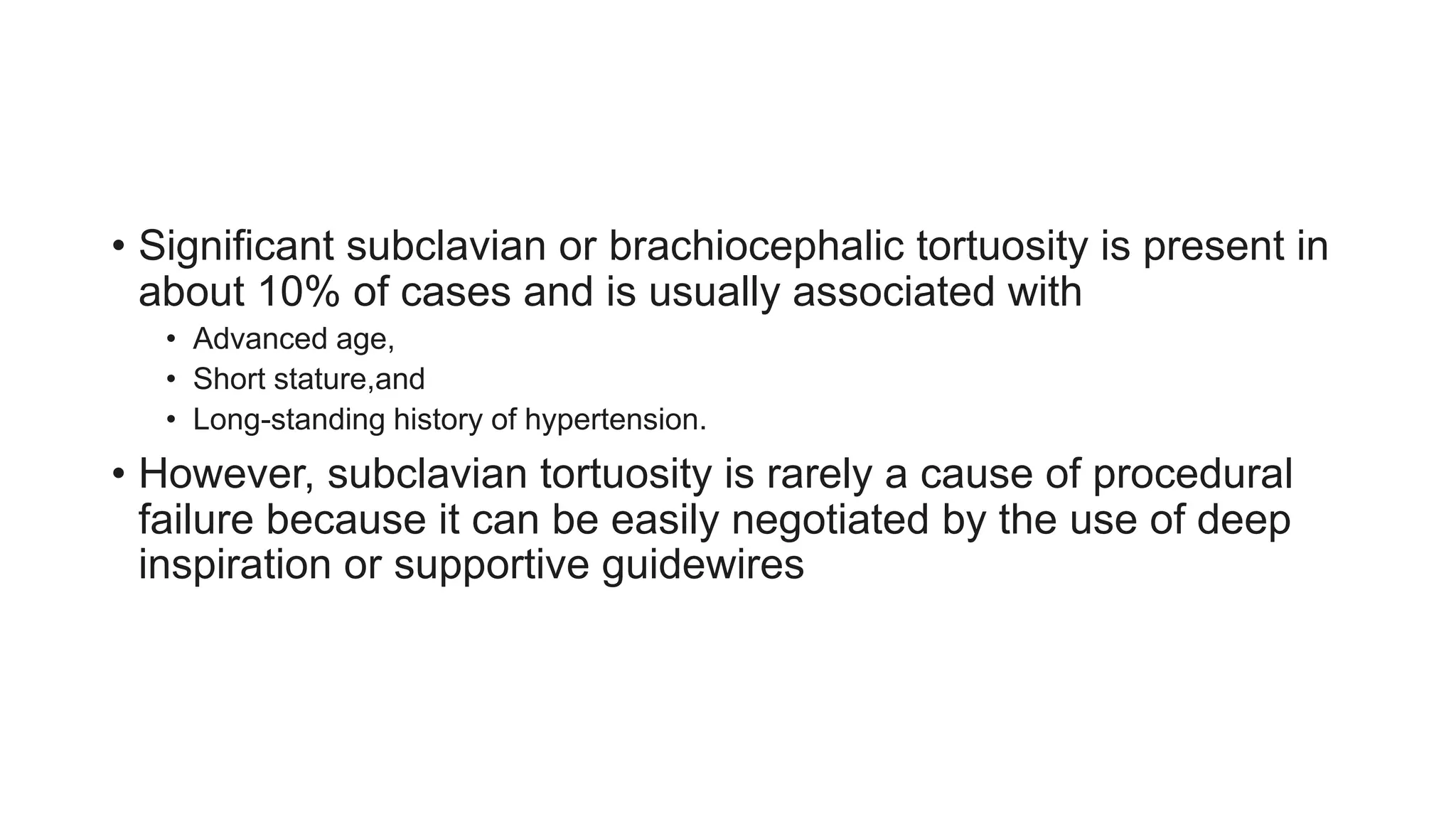
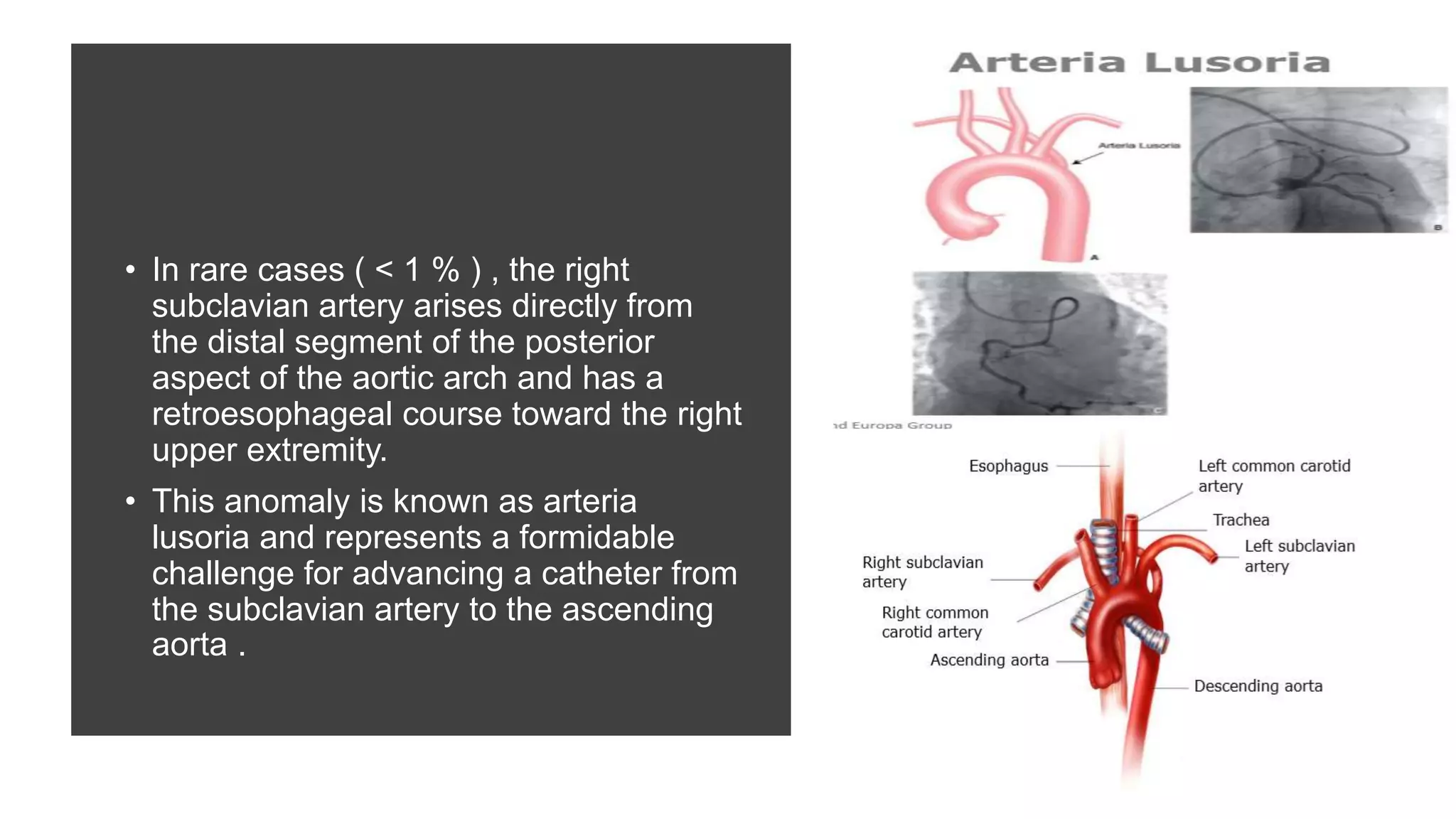
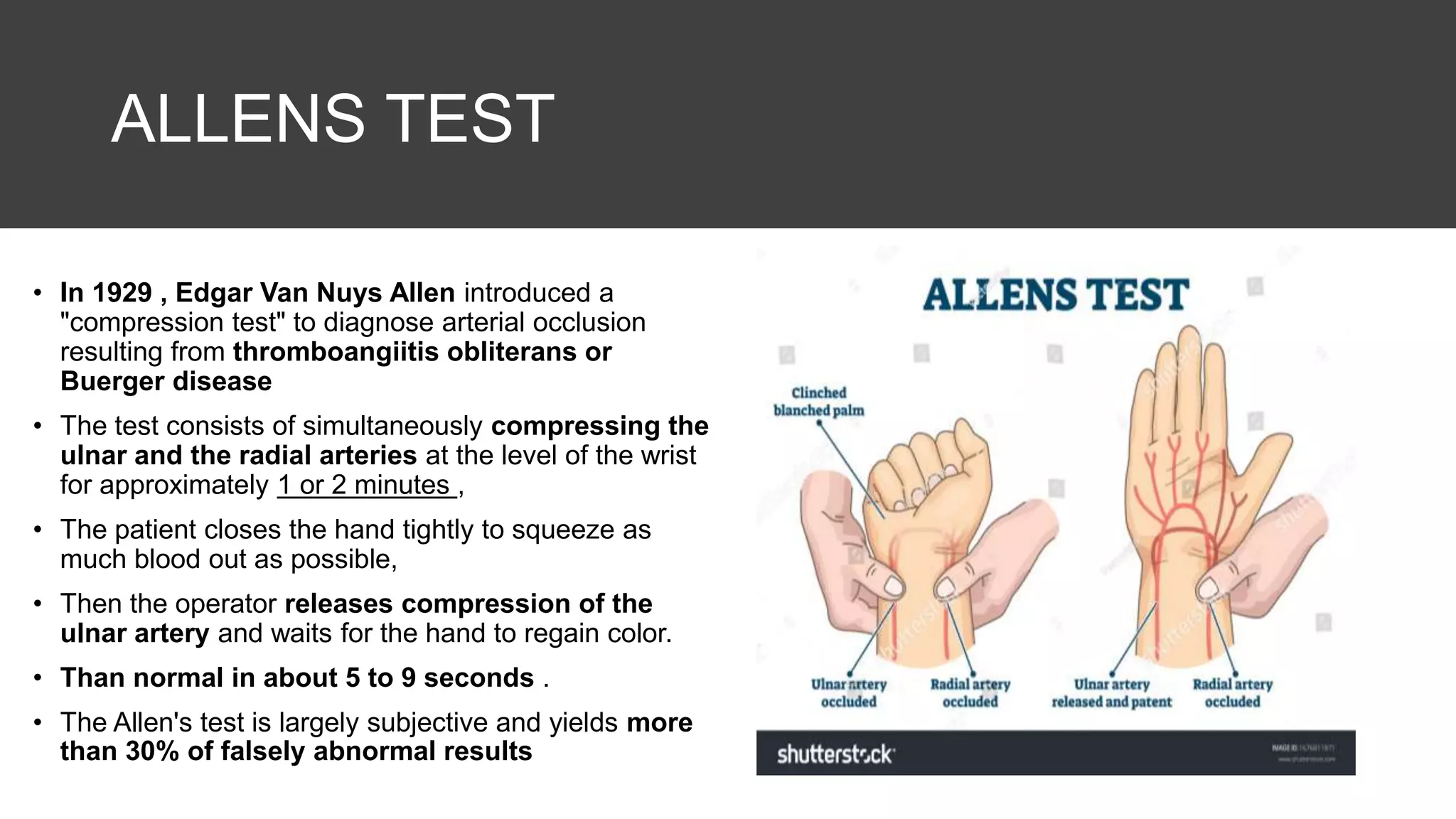
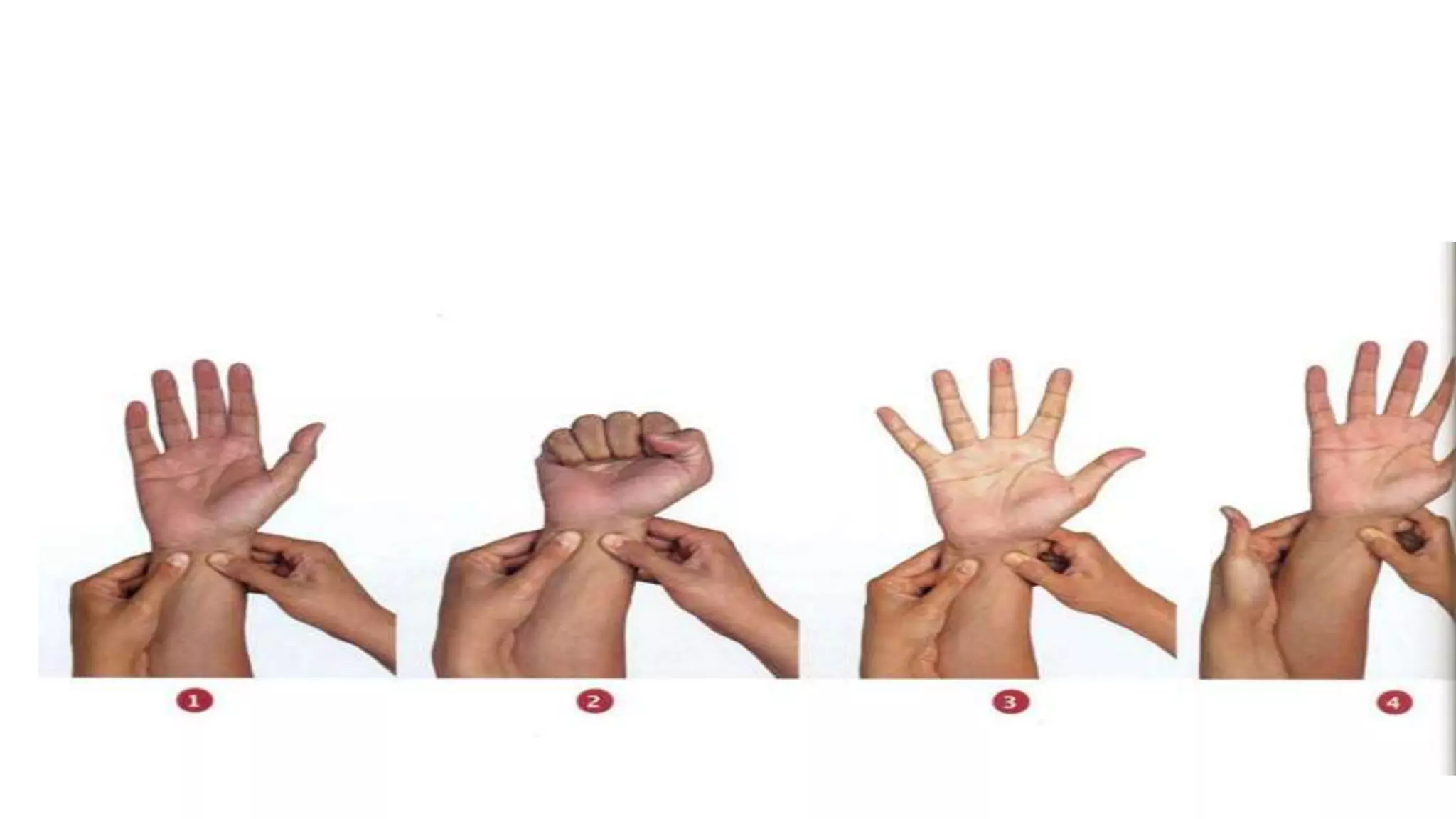
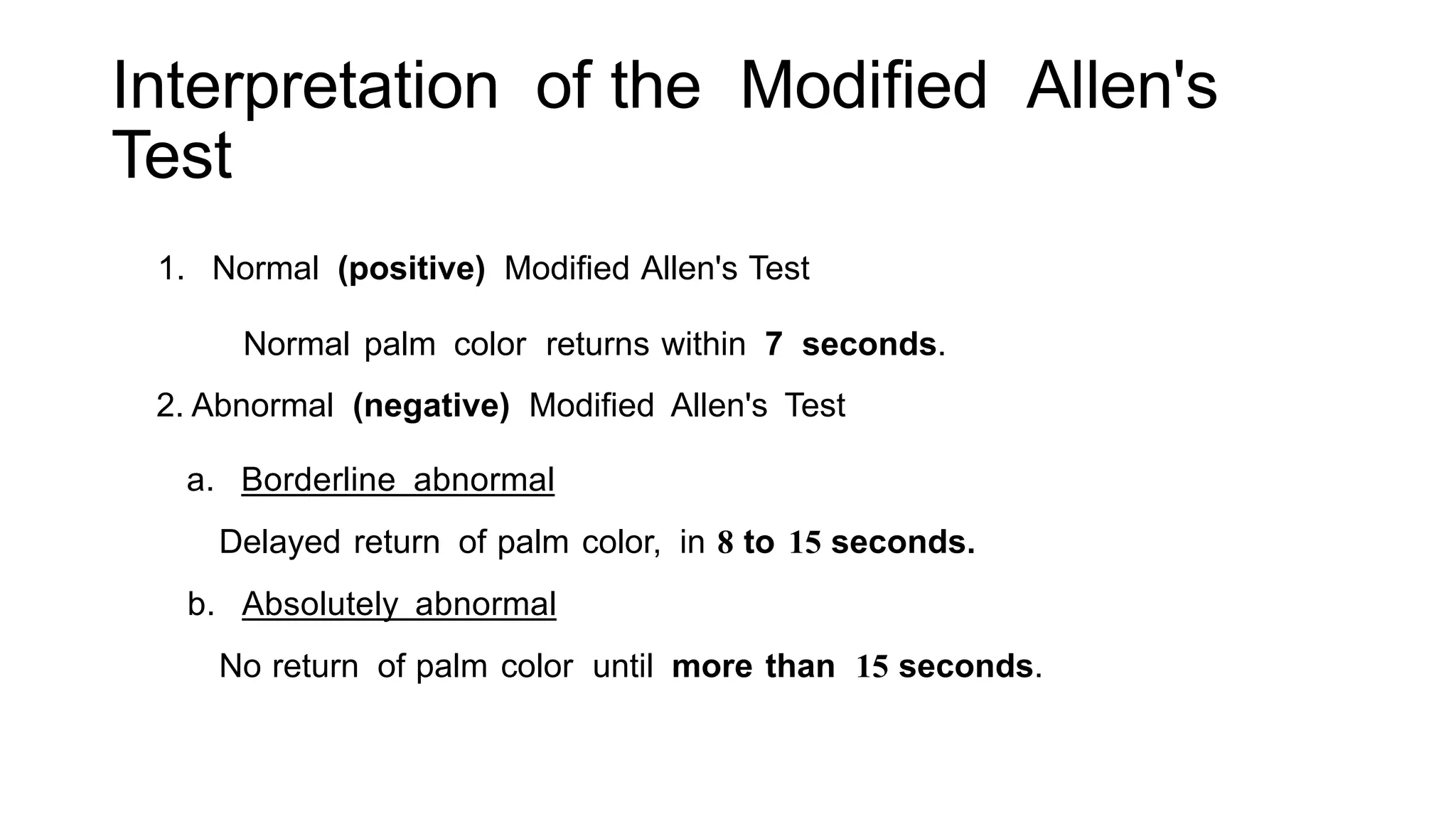
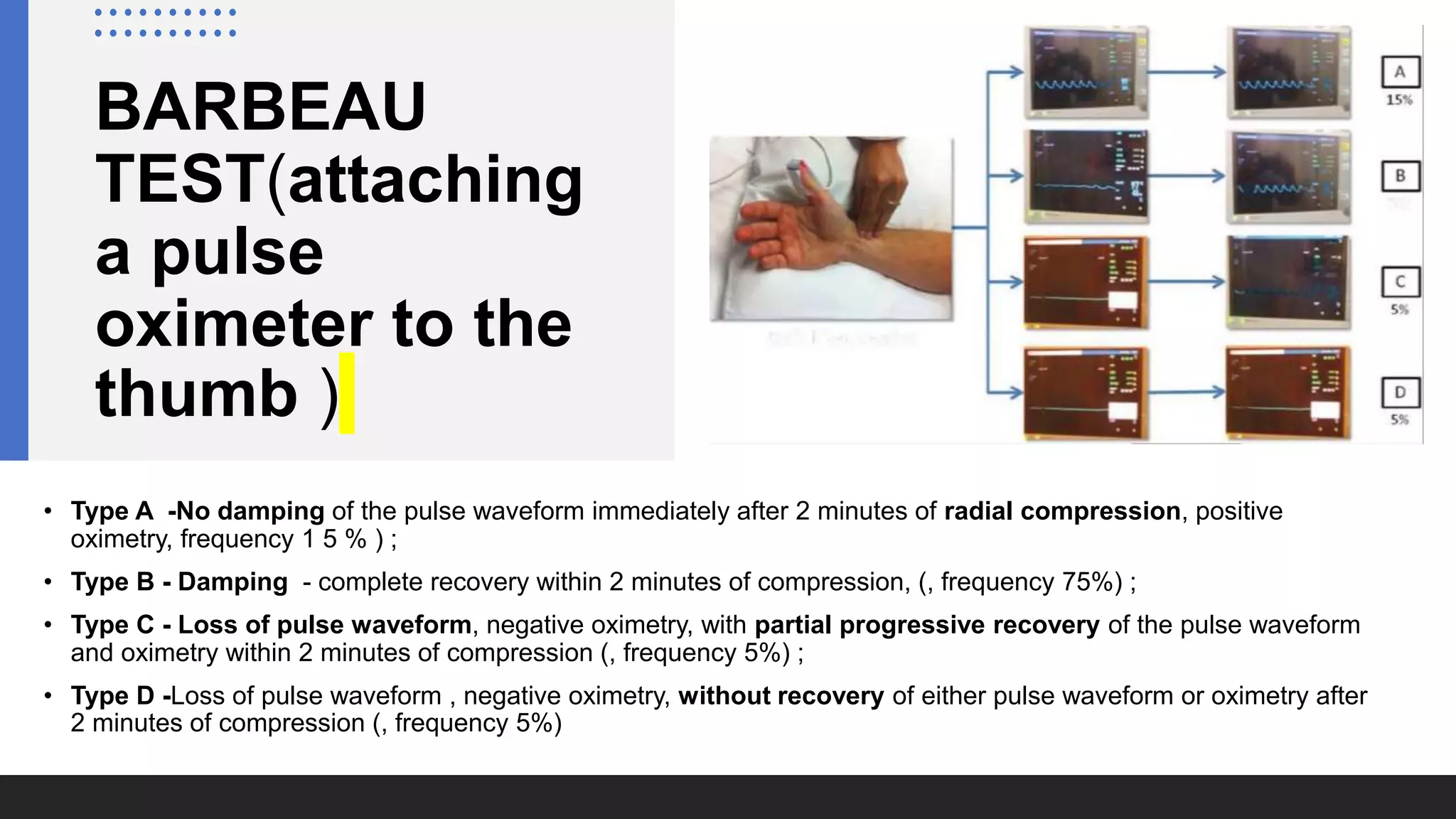
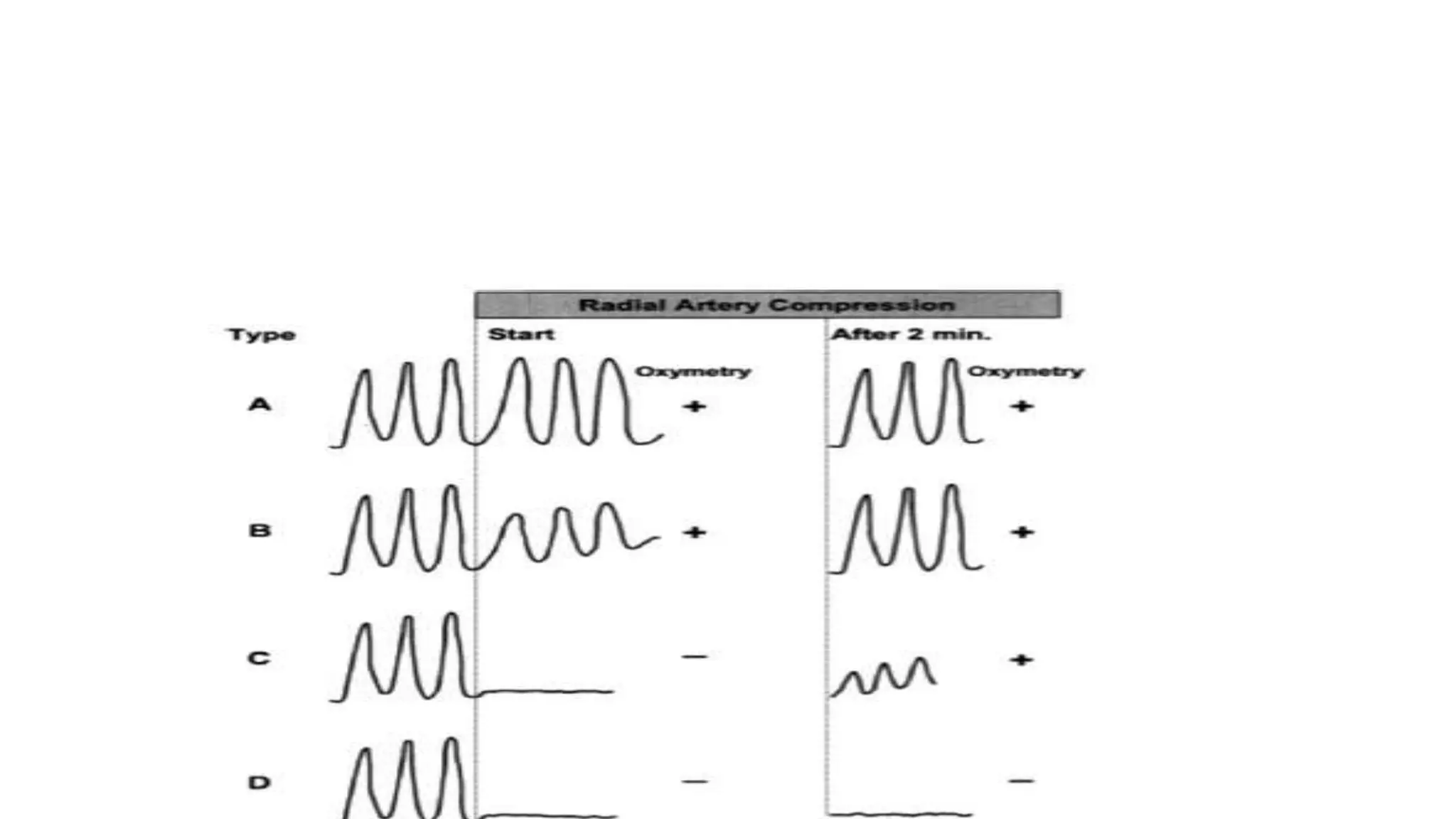
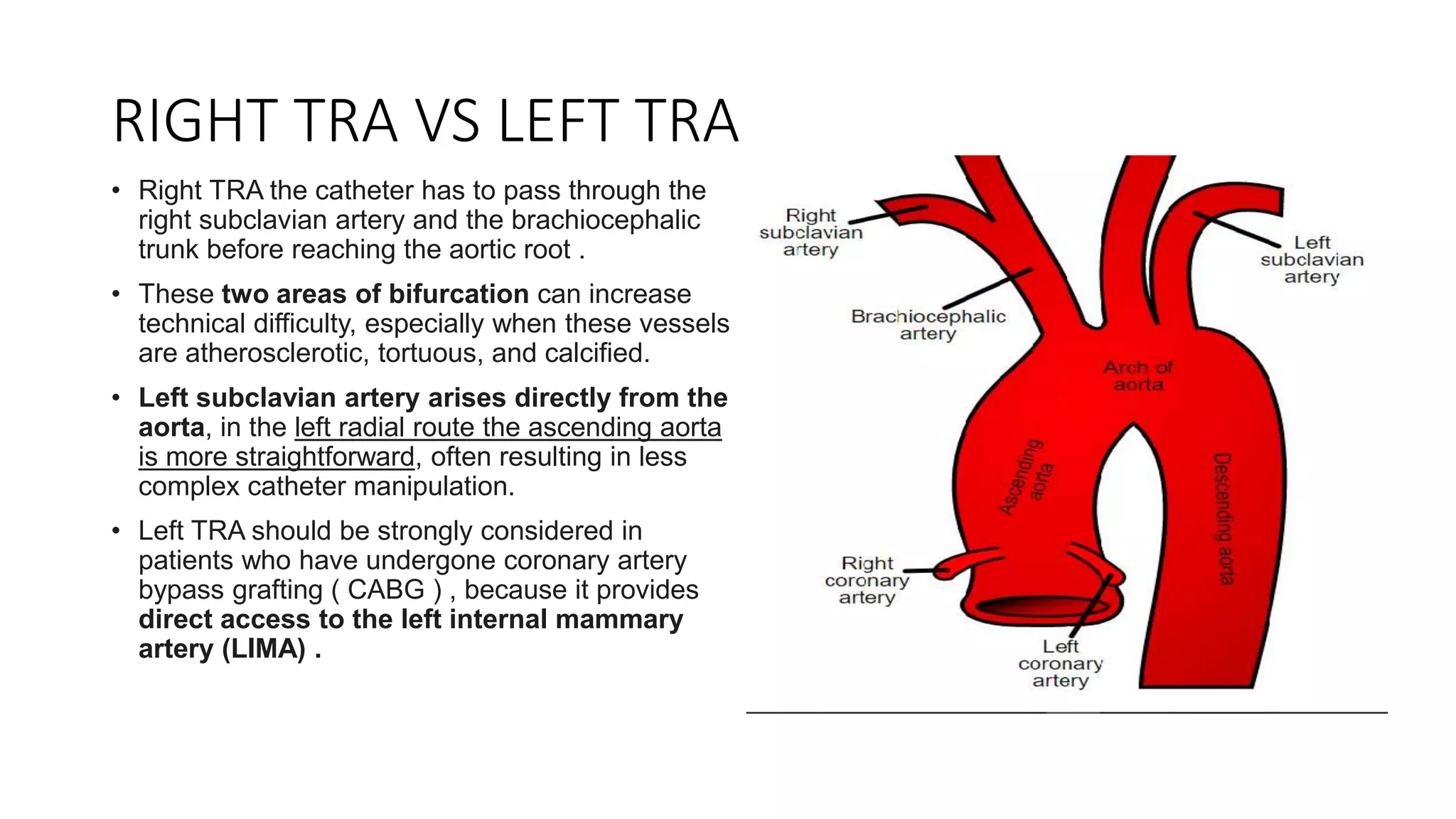
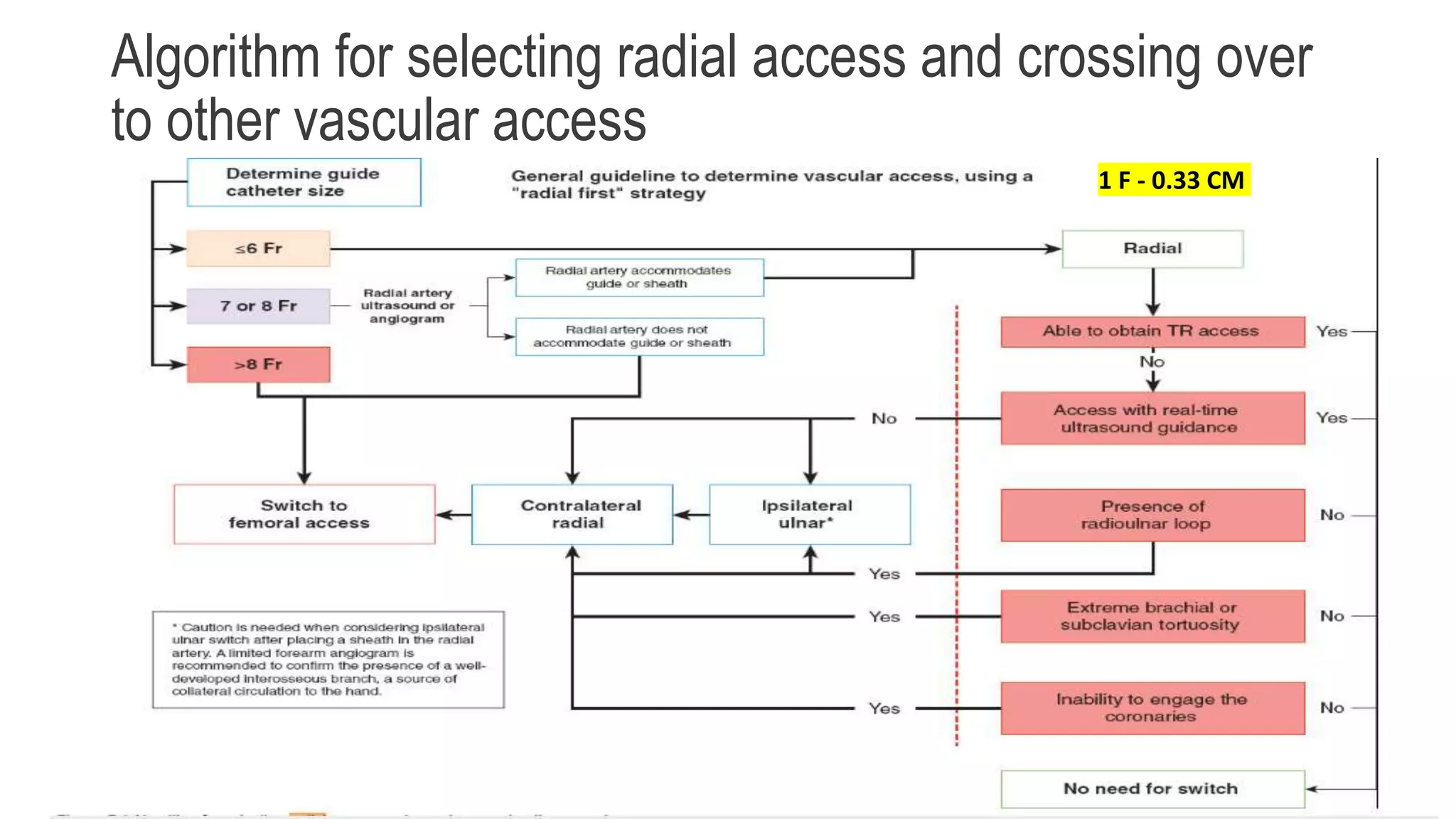
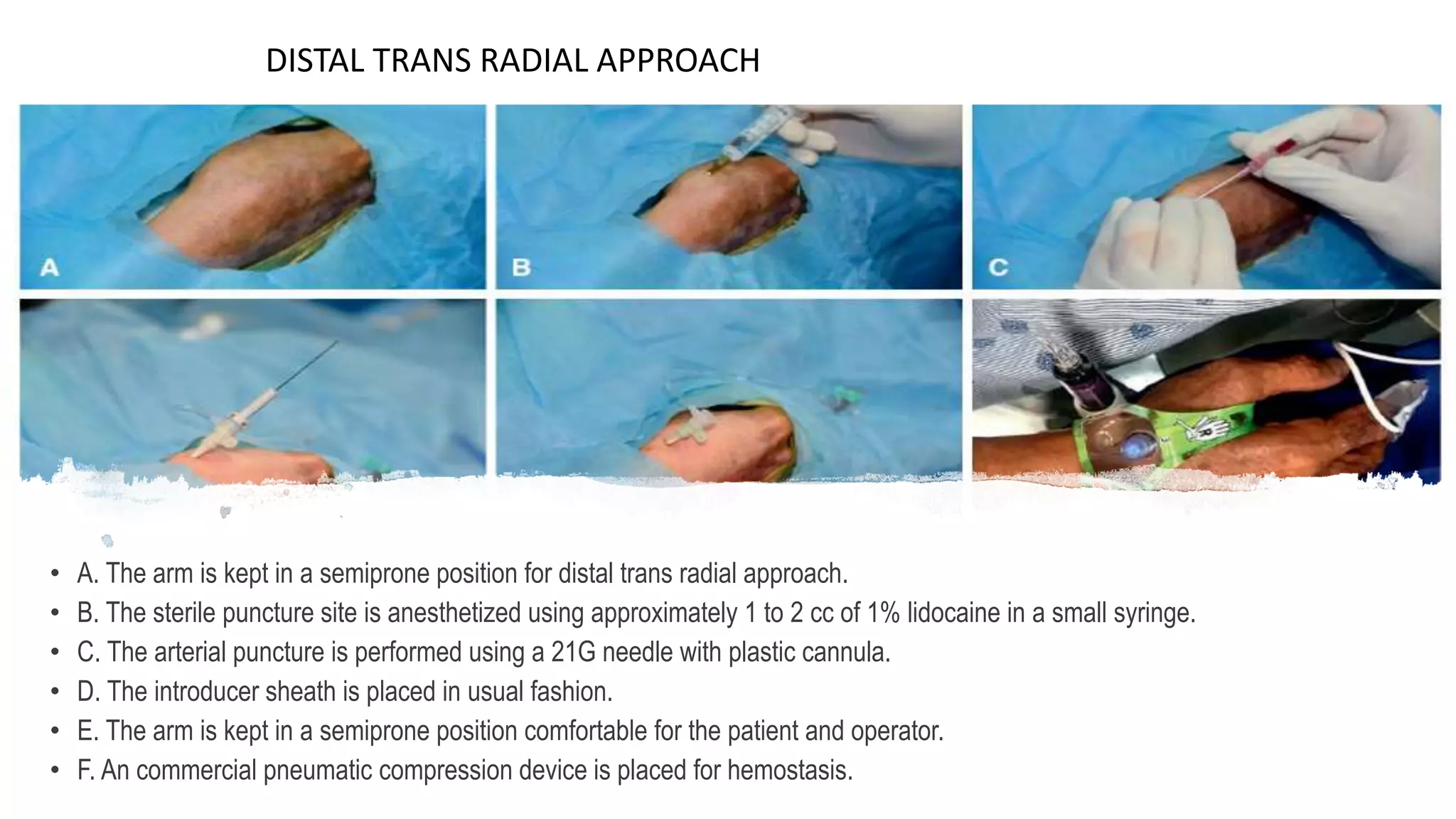
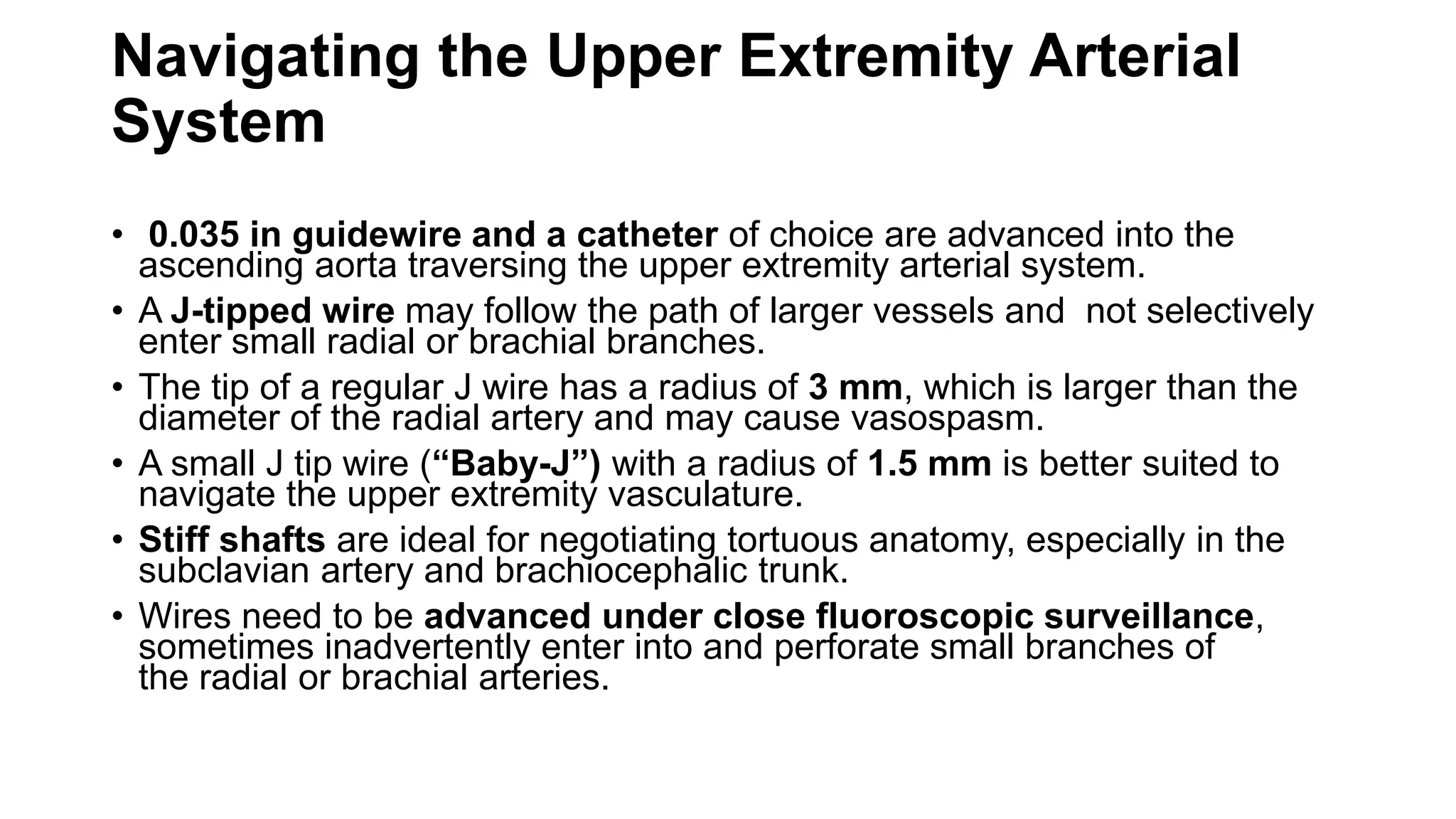
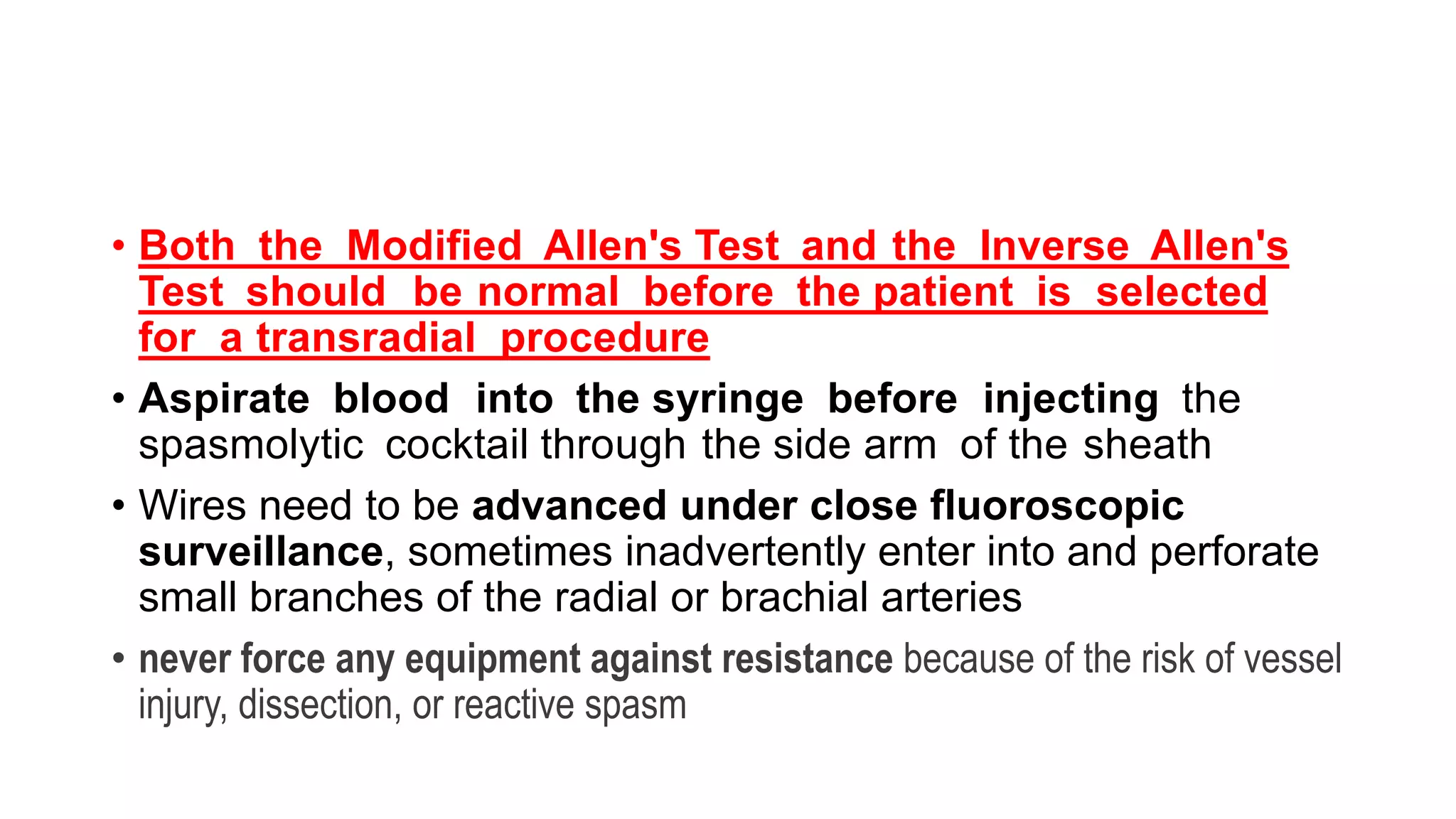
2. The radial artery anatomy and variations like tortuosity must be considered to select appropriate patients and techniques.
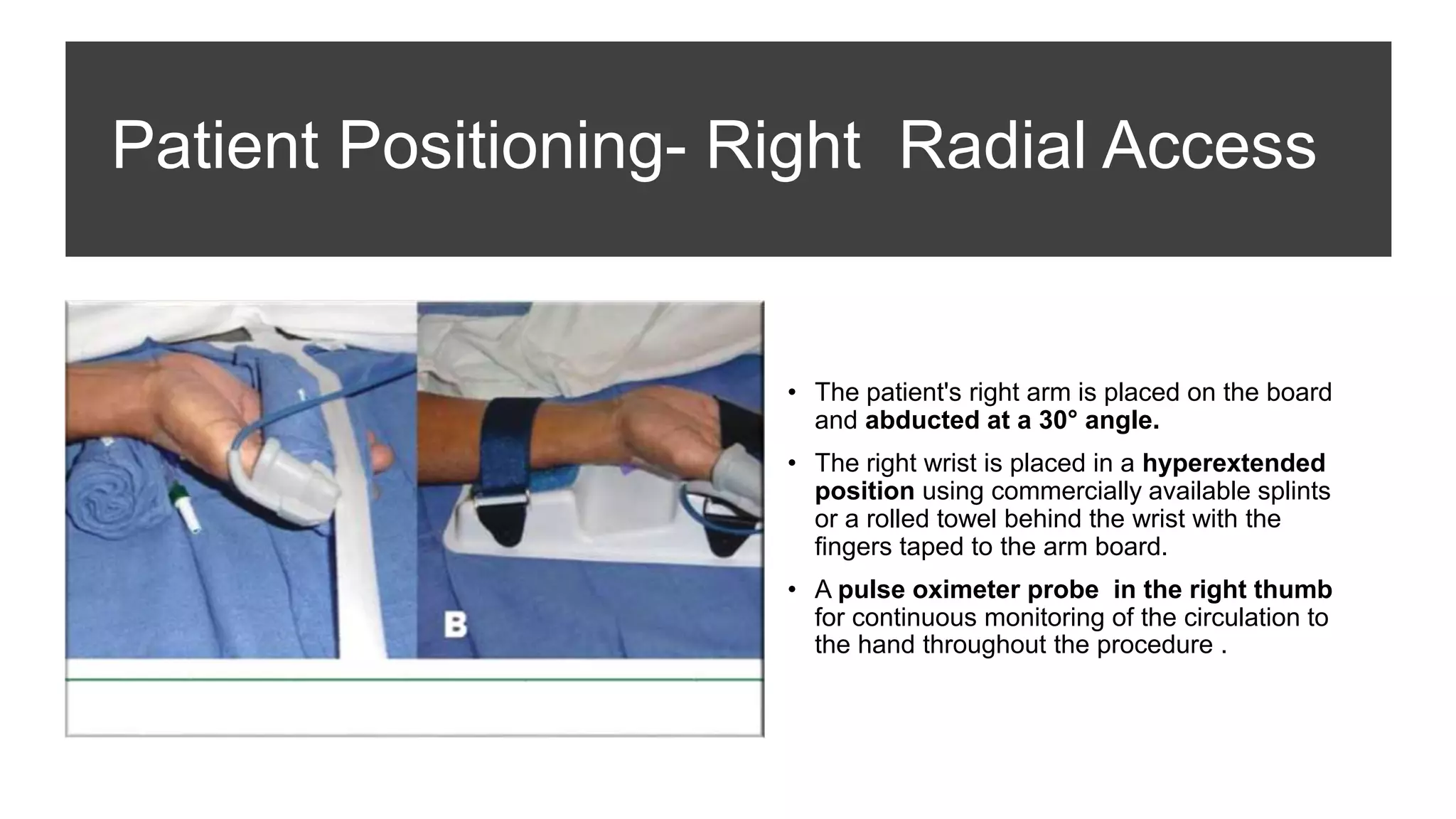
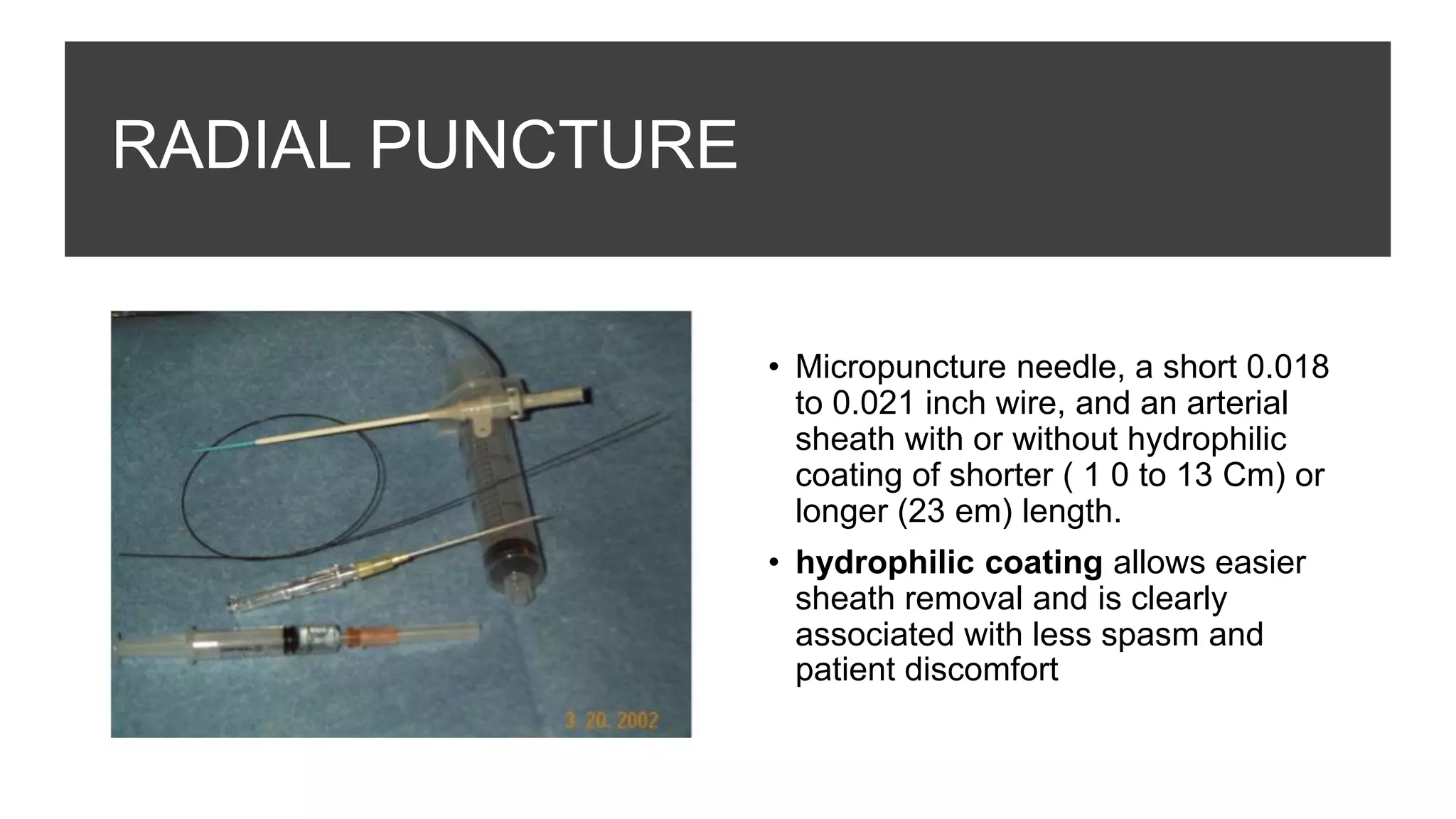
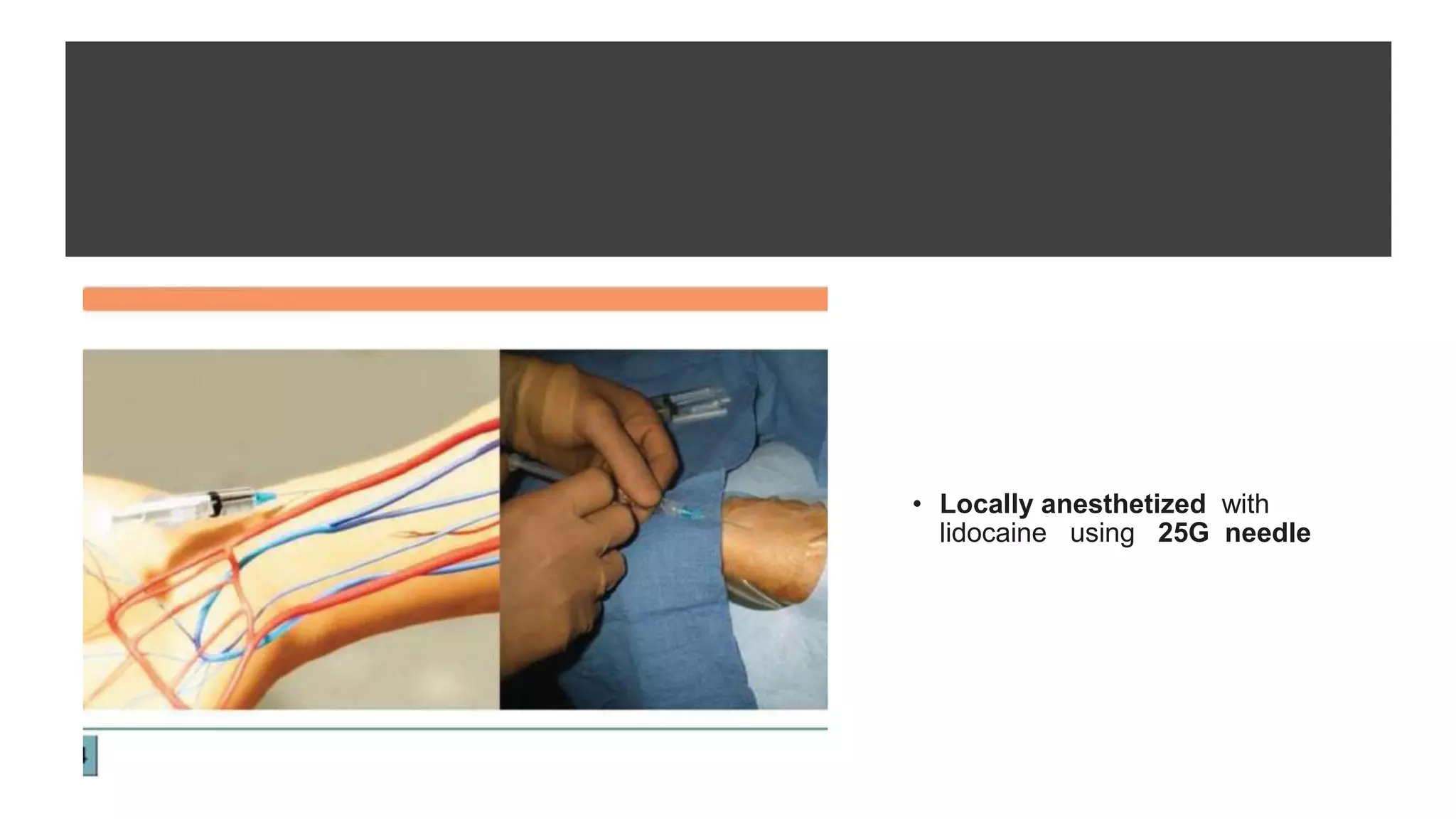
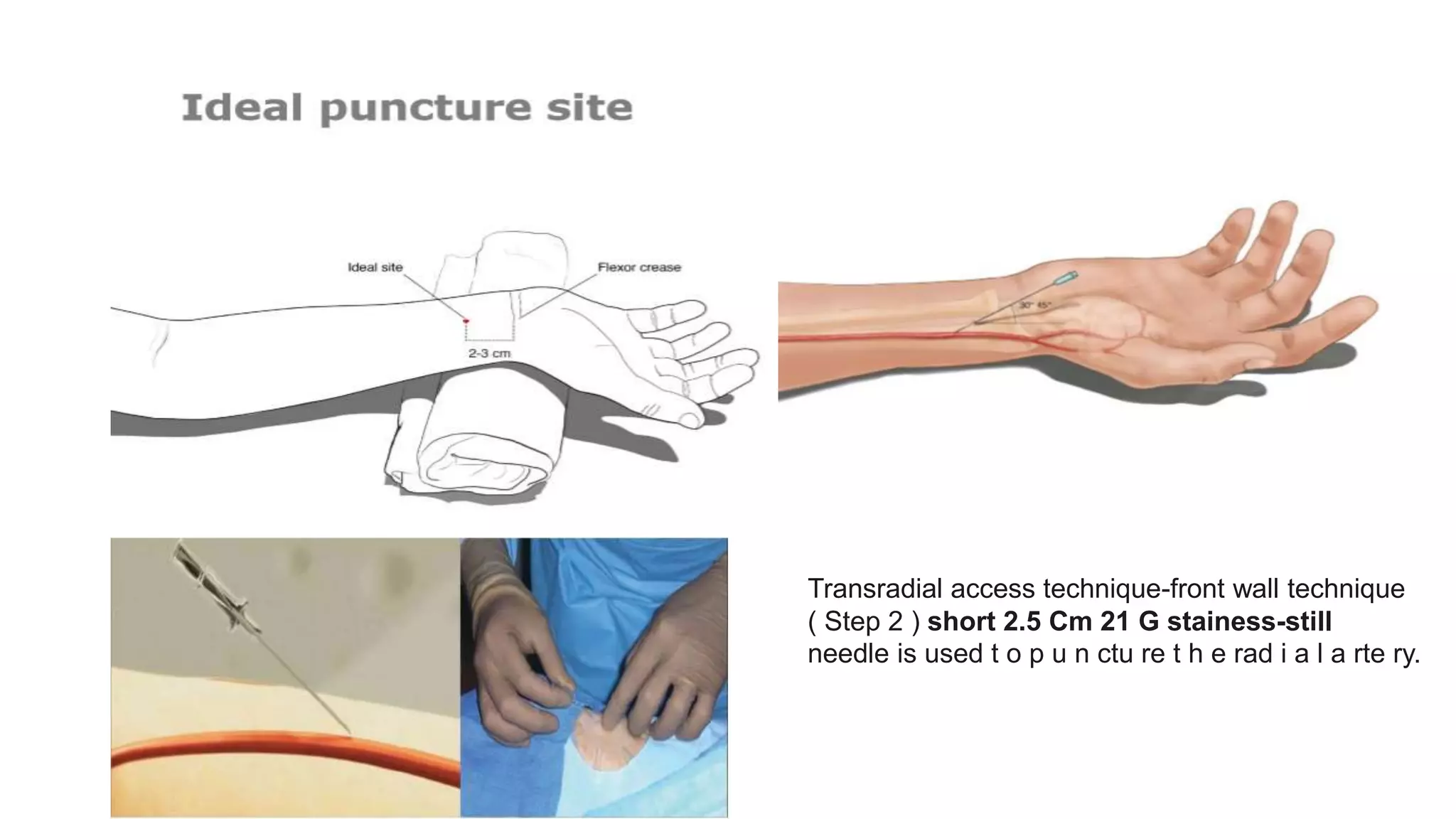
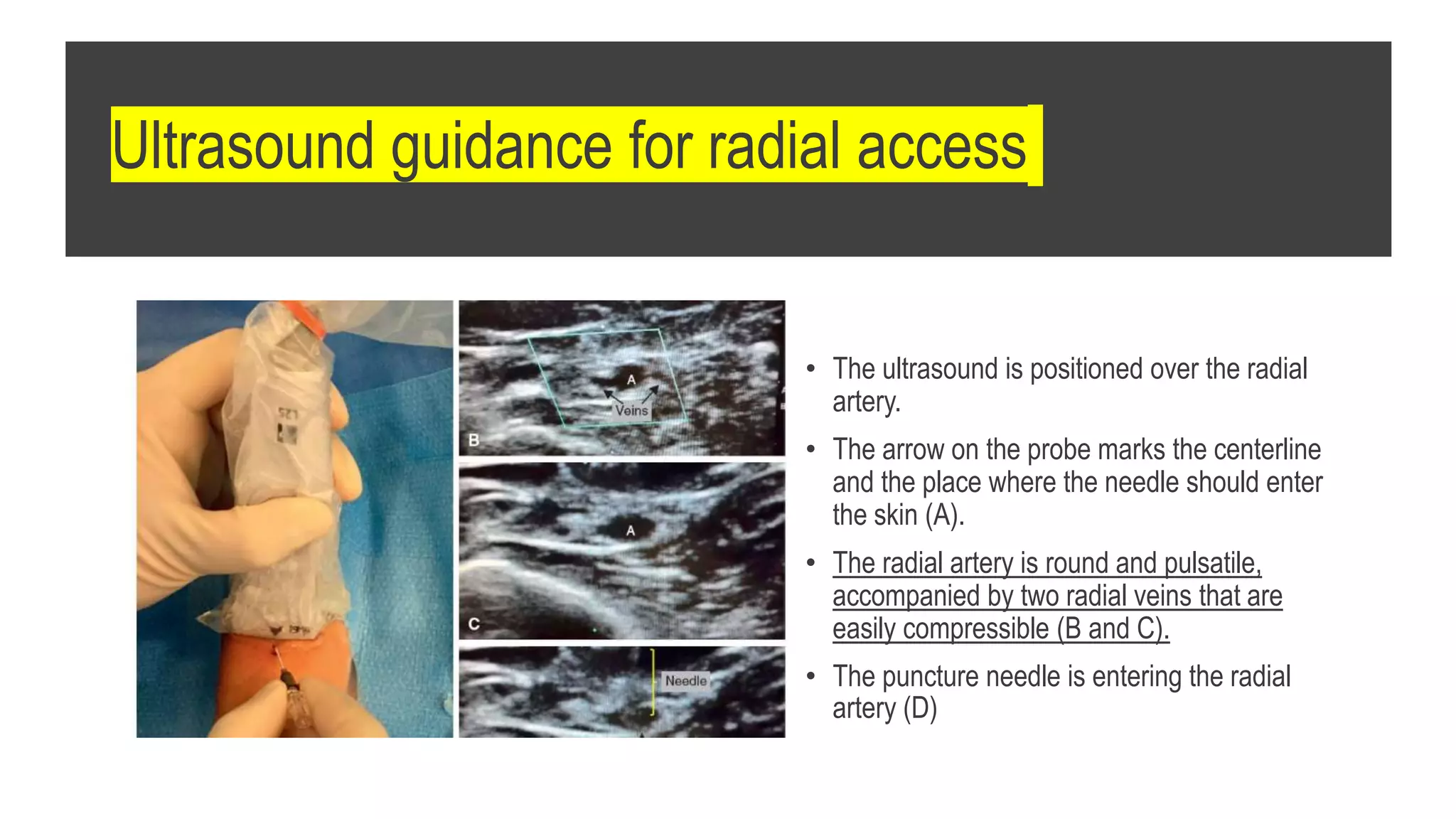
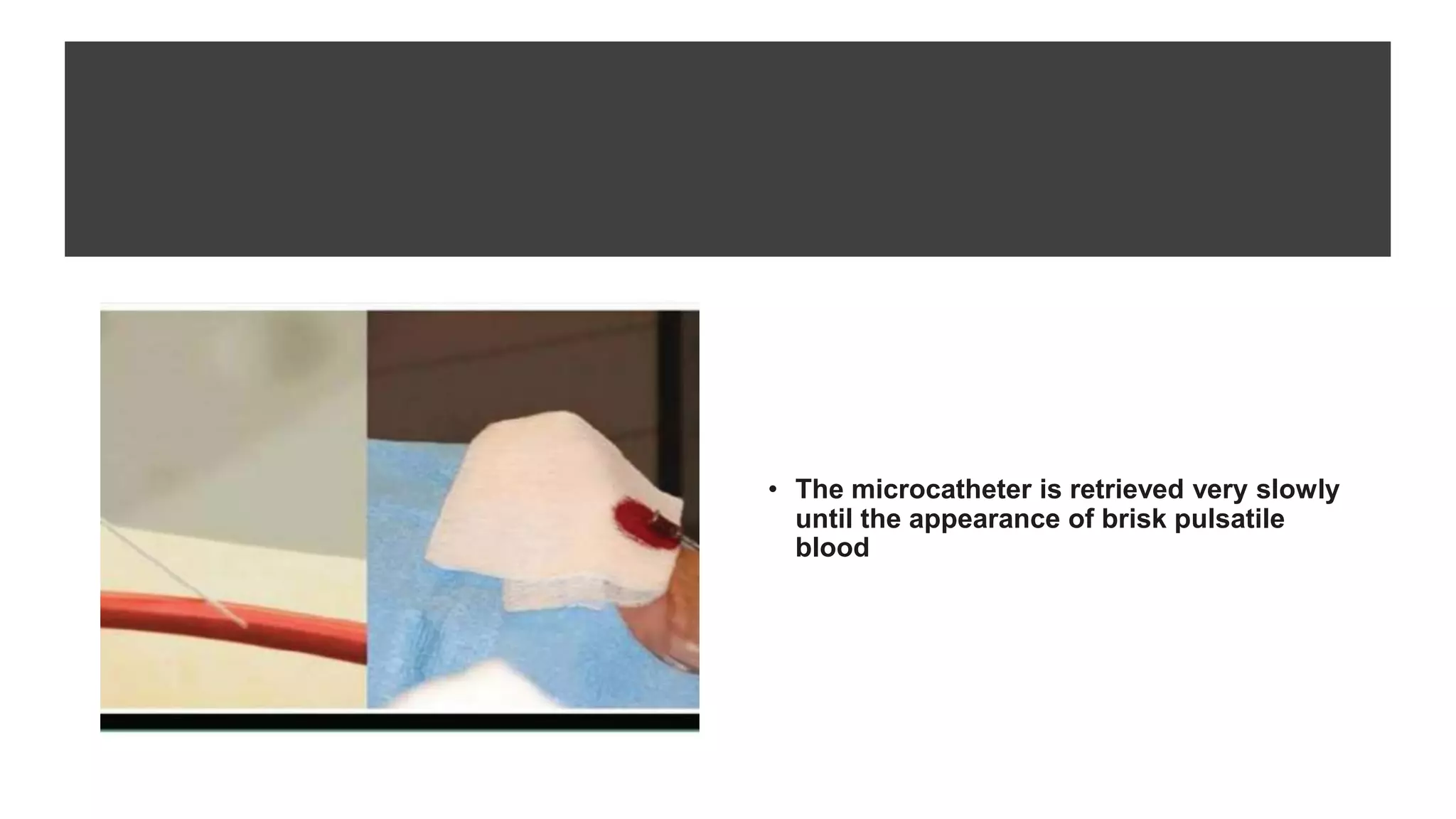
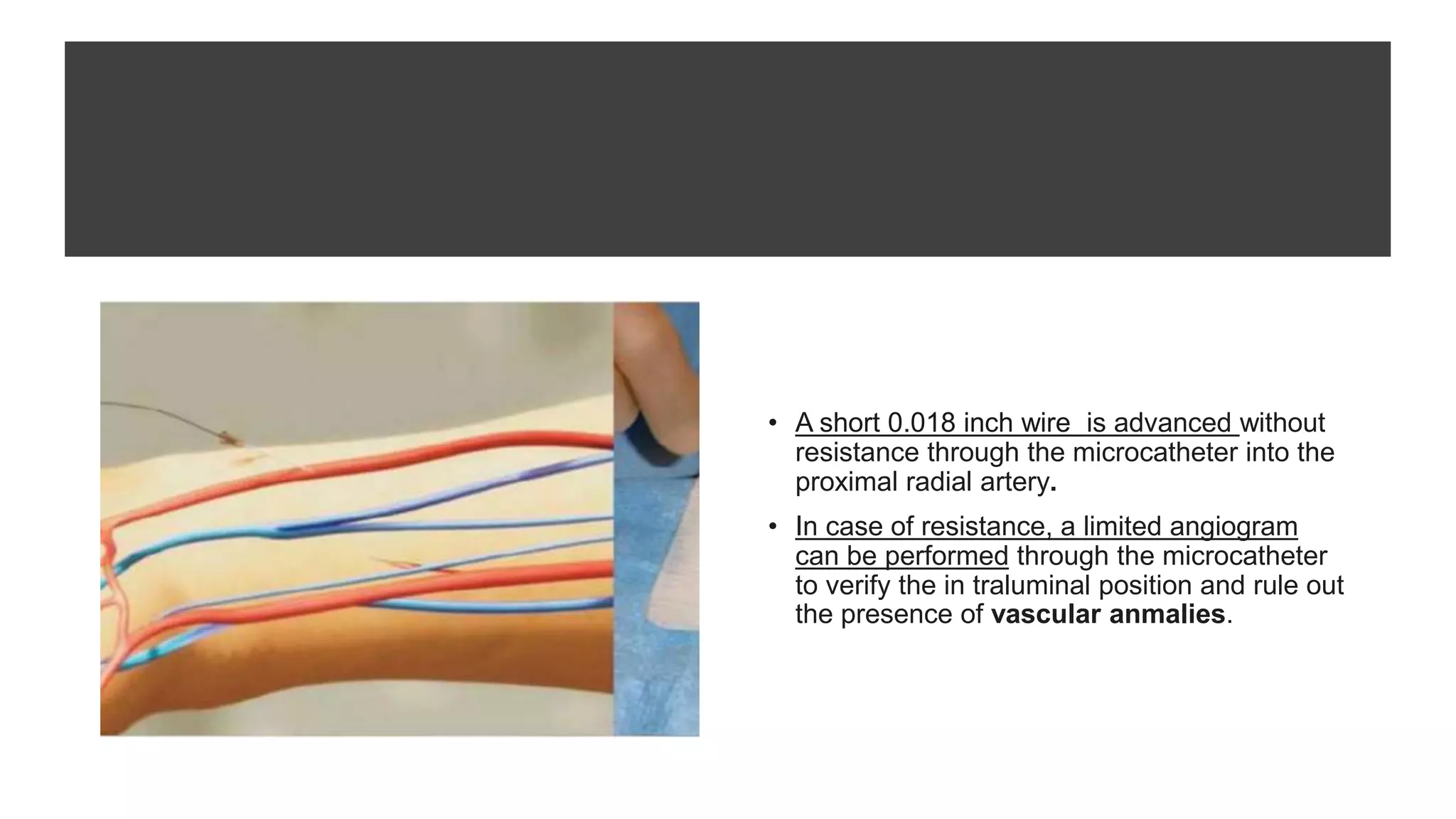
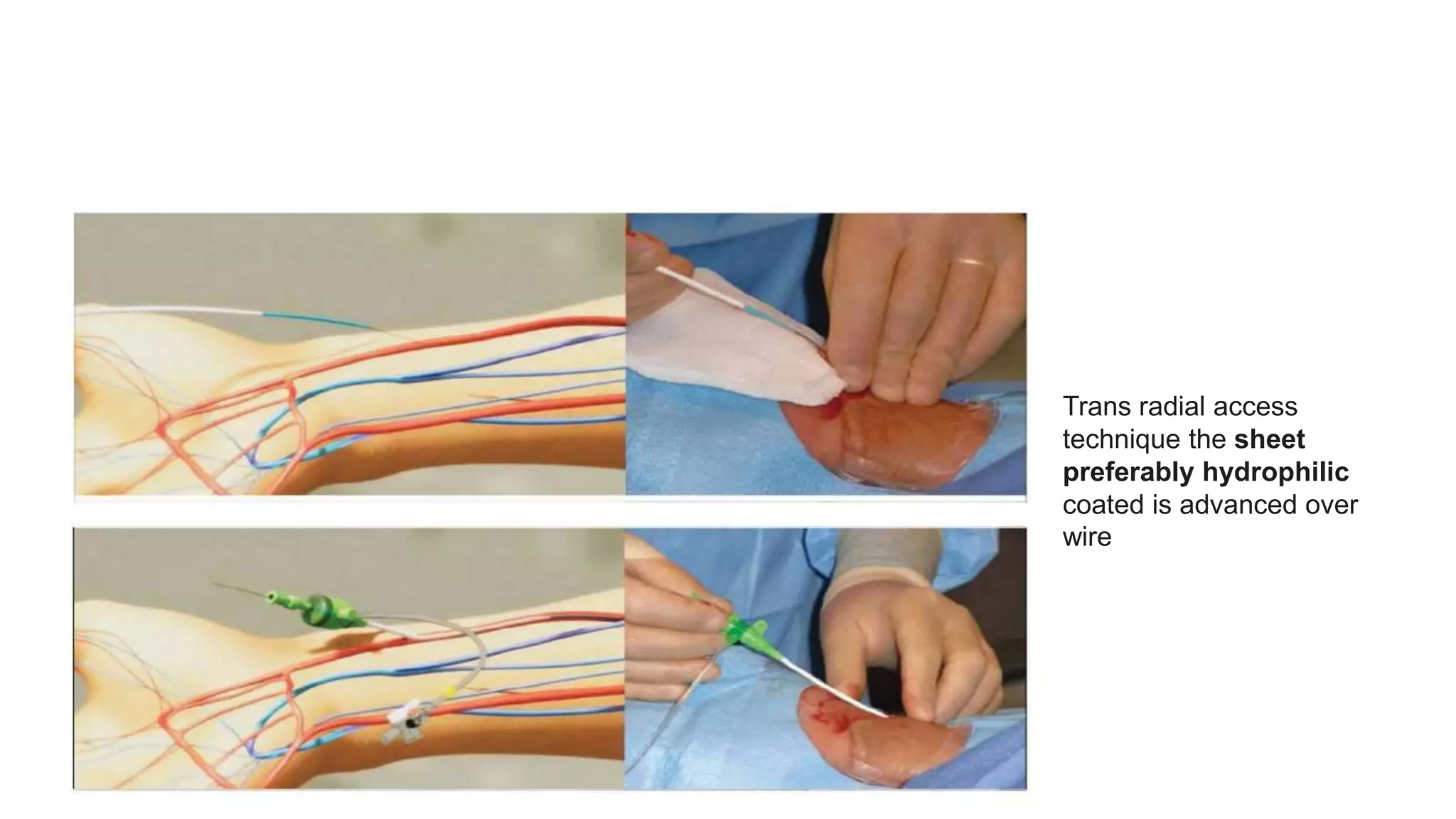
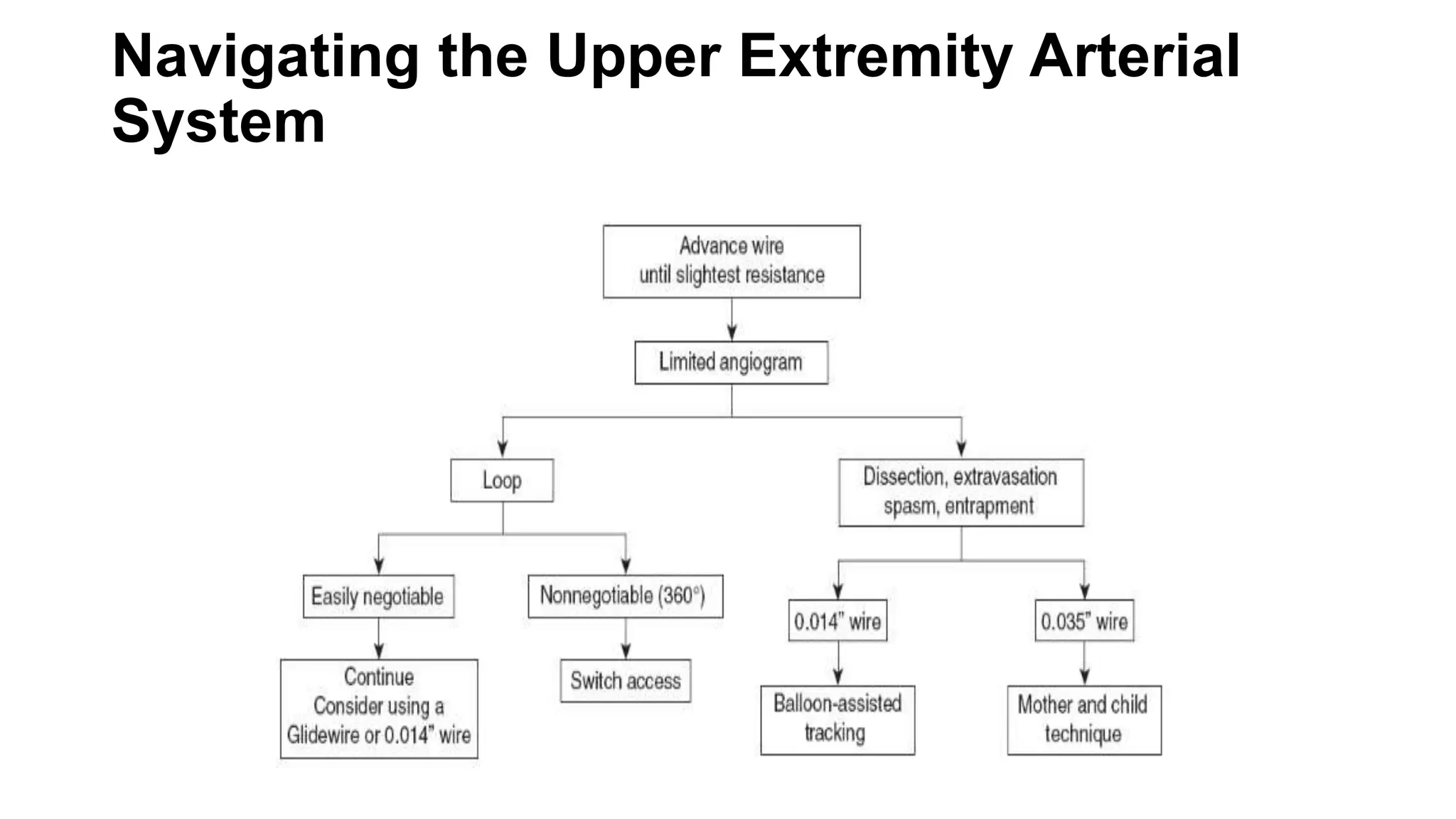
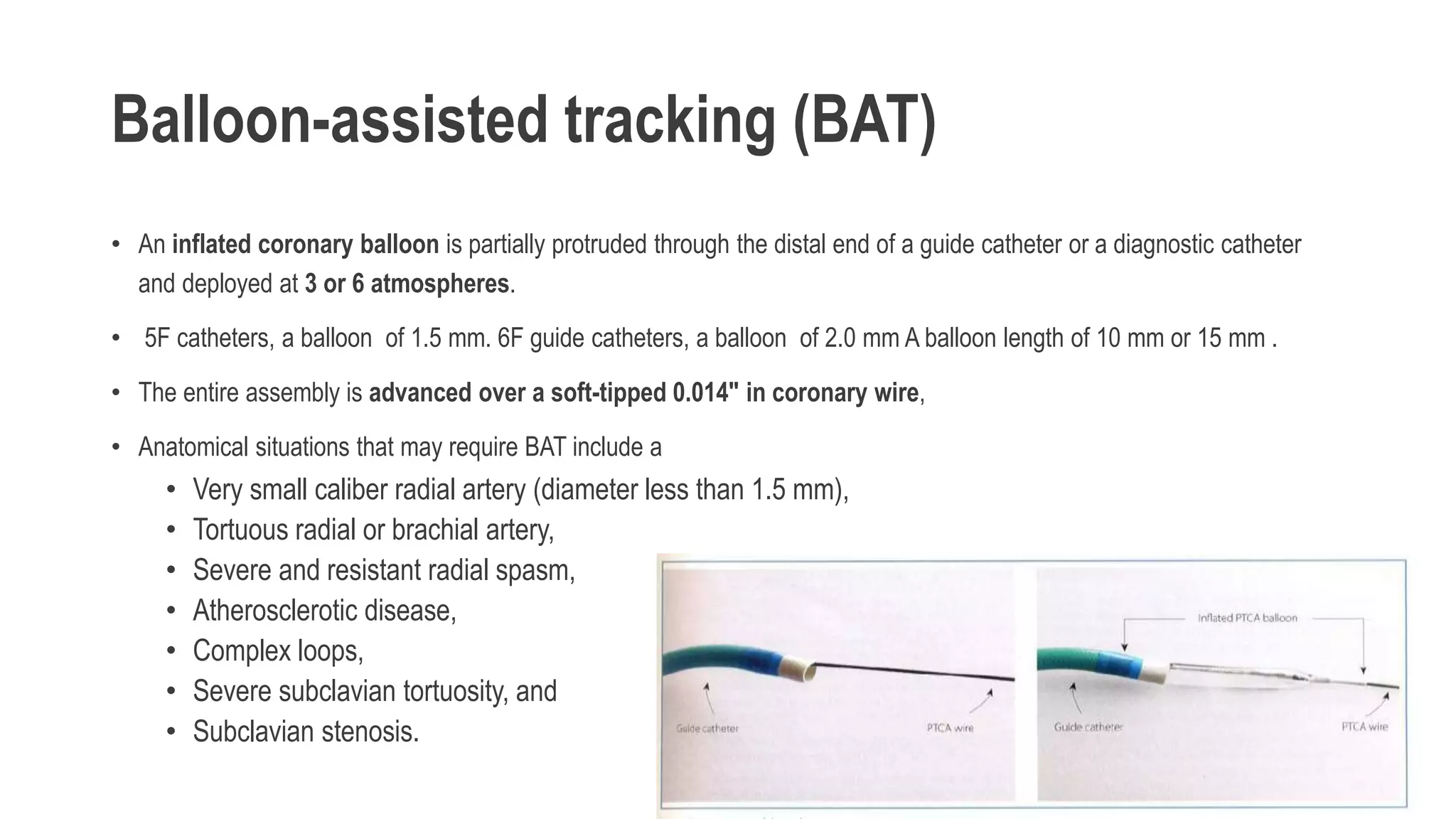
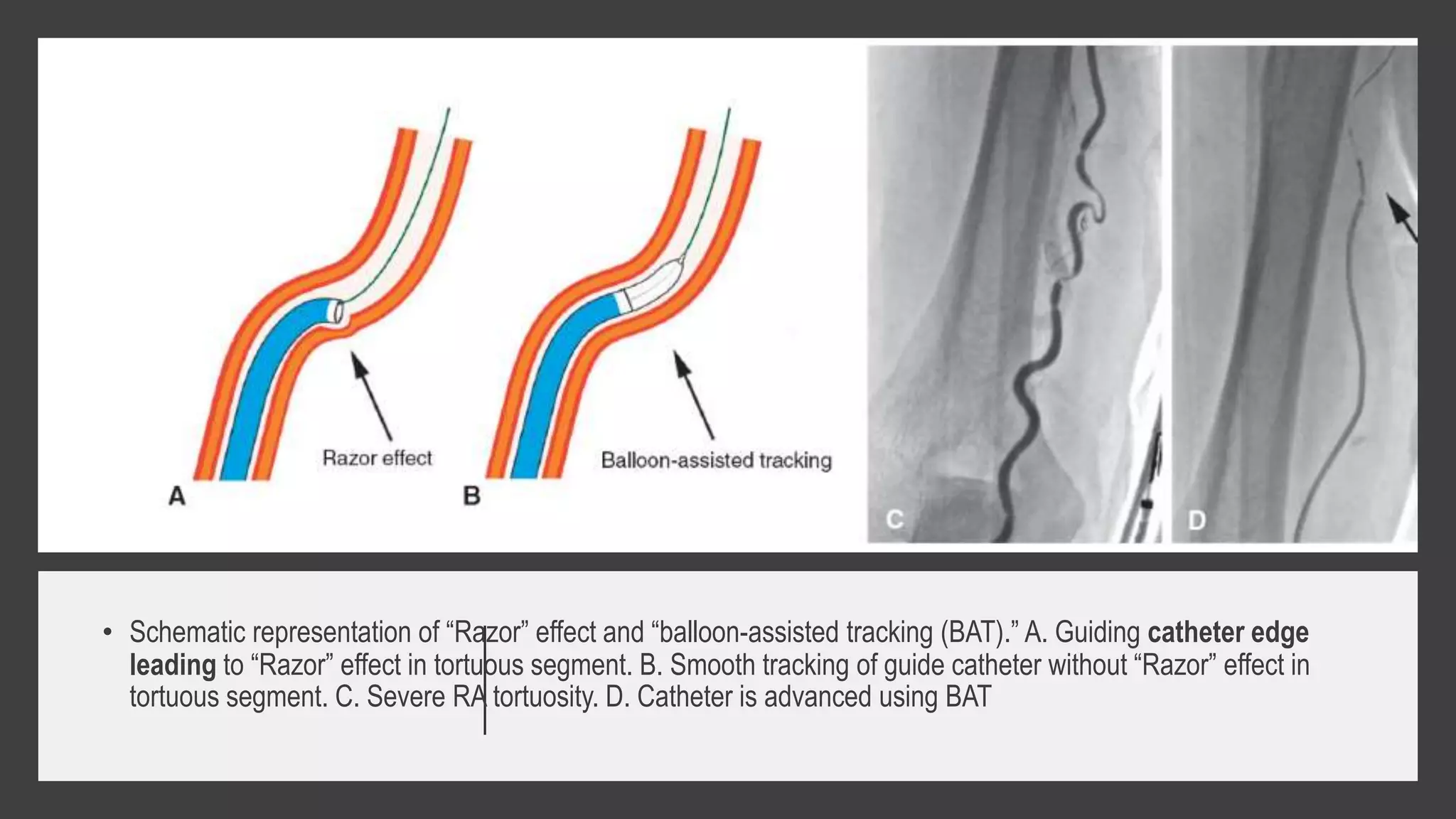
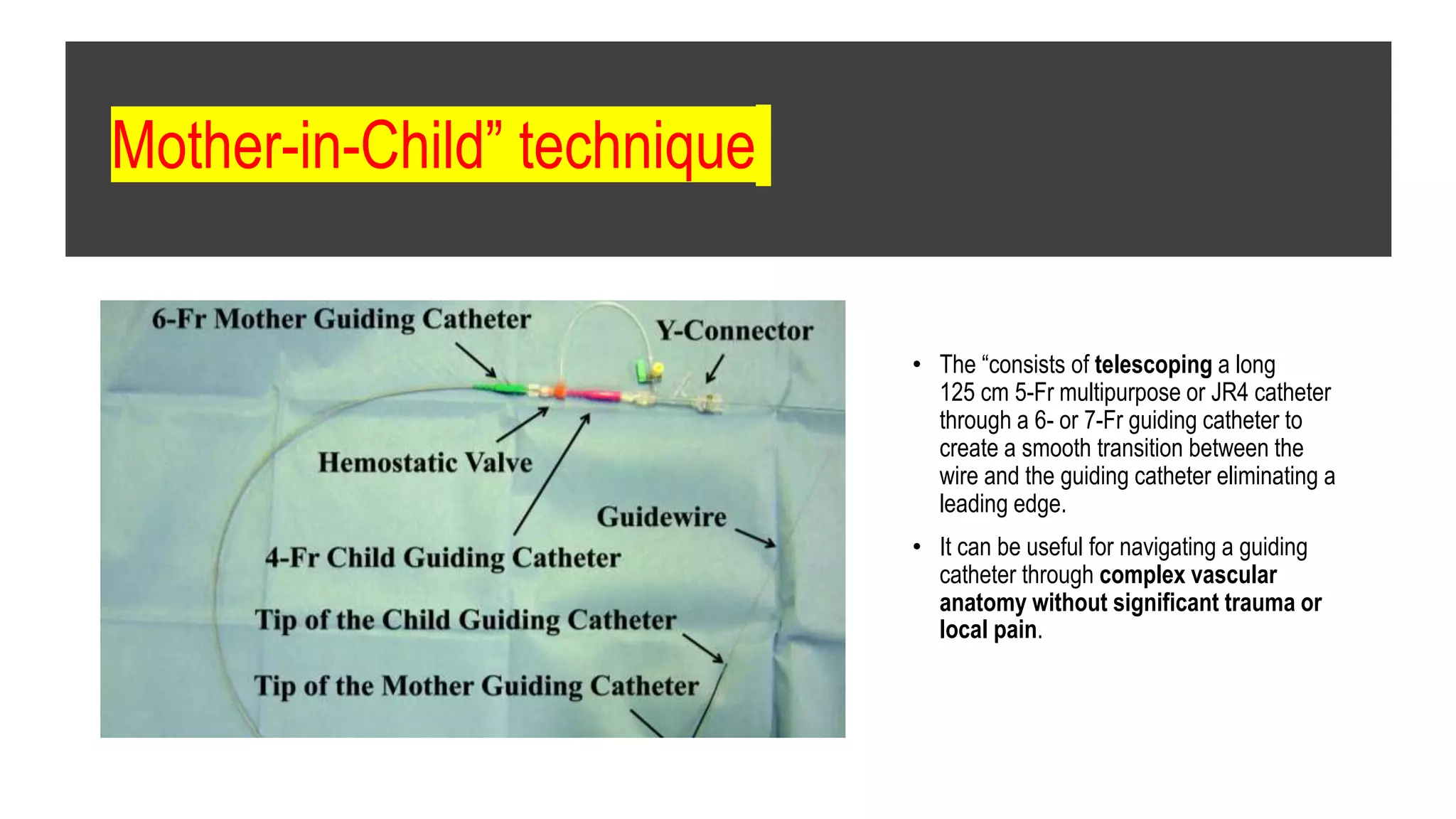
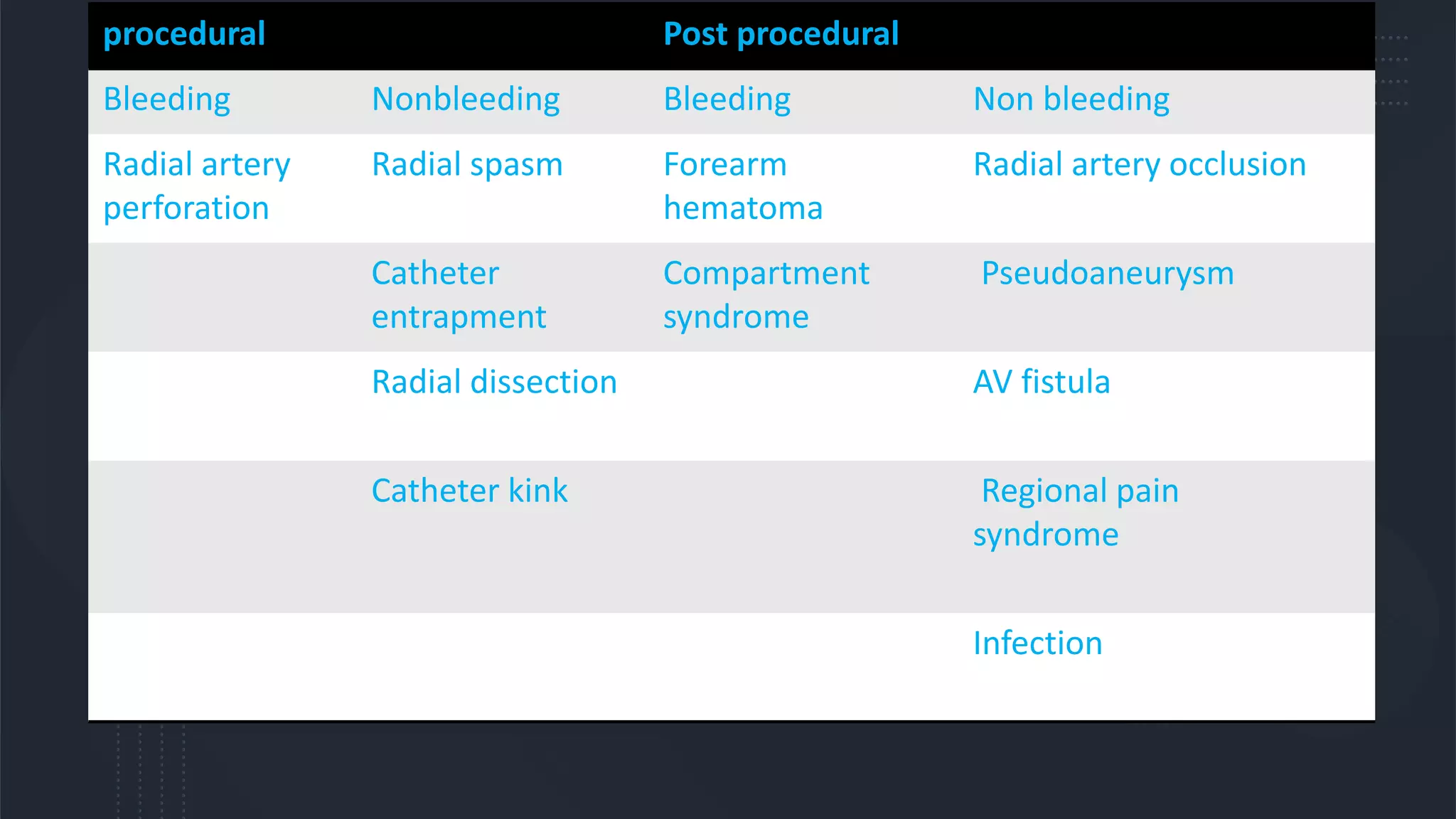
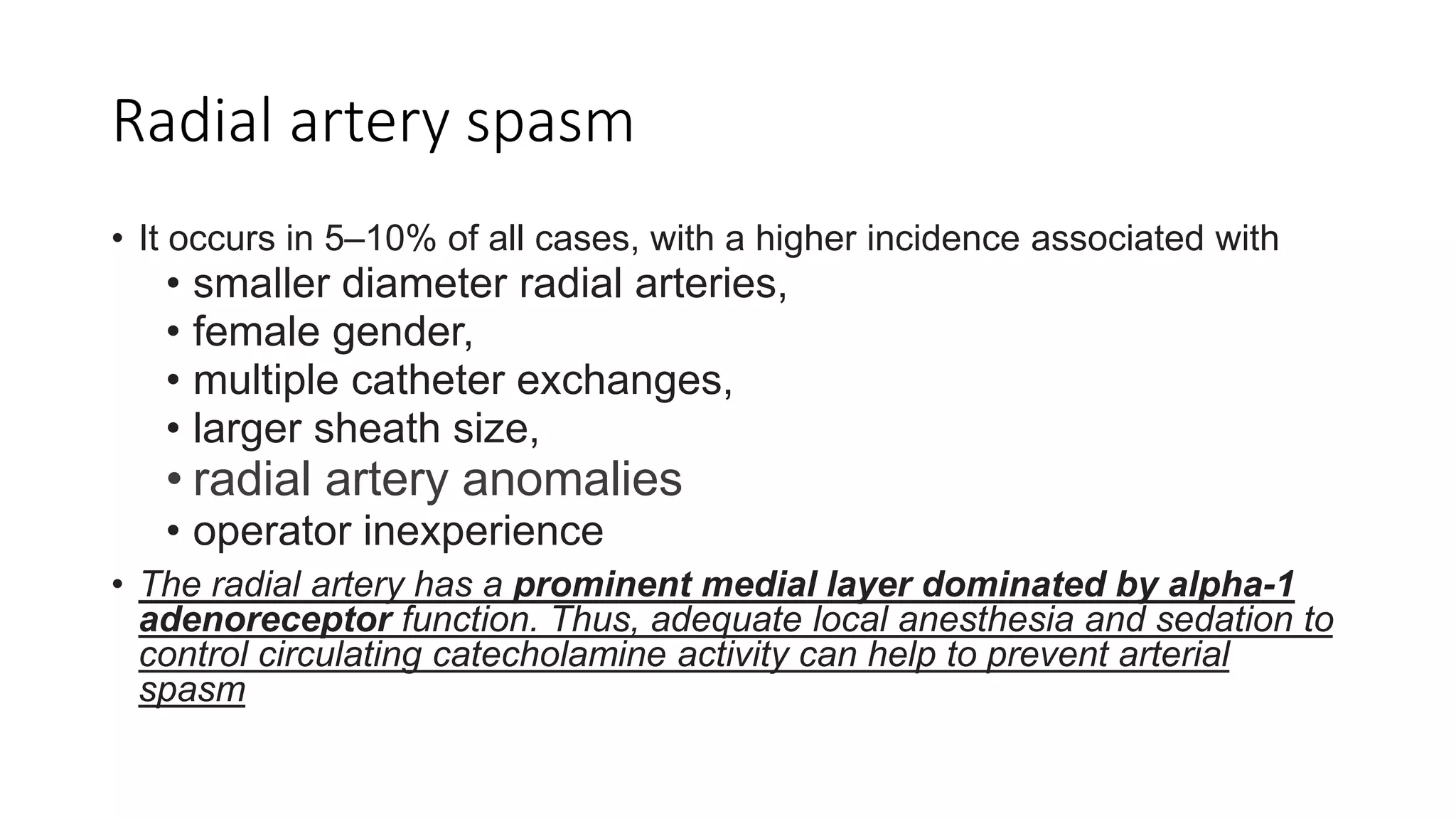
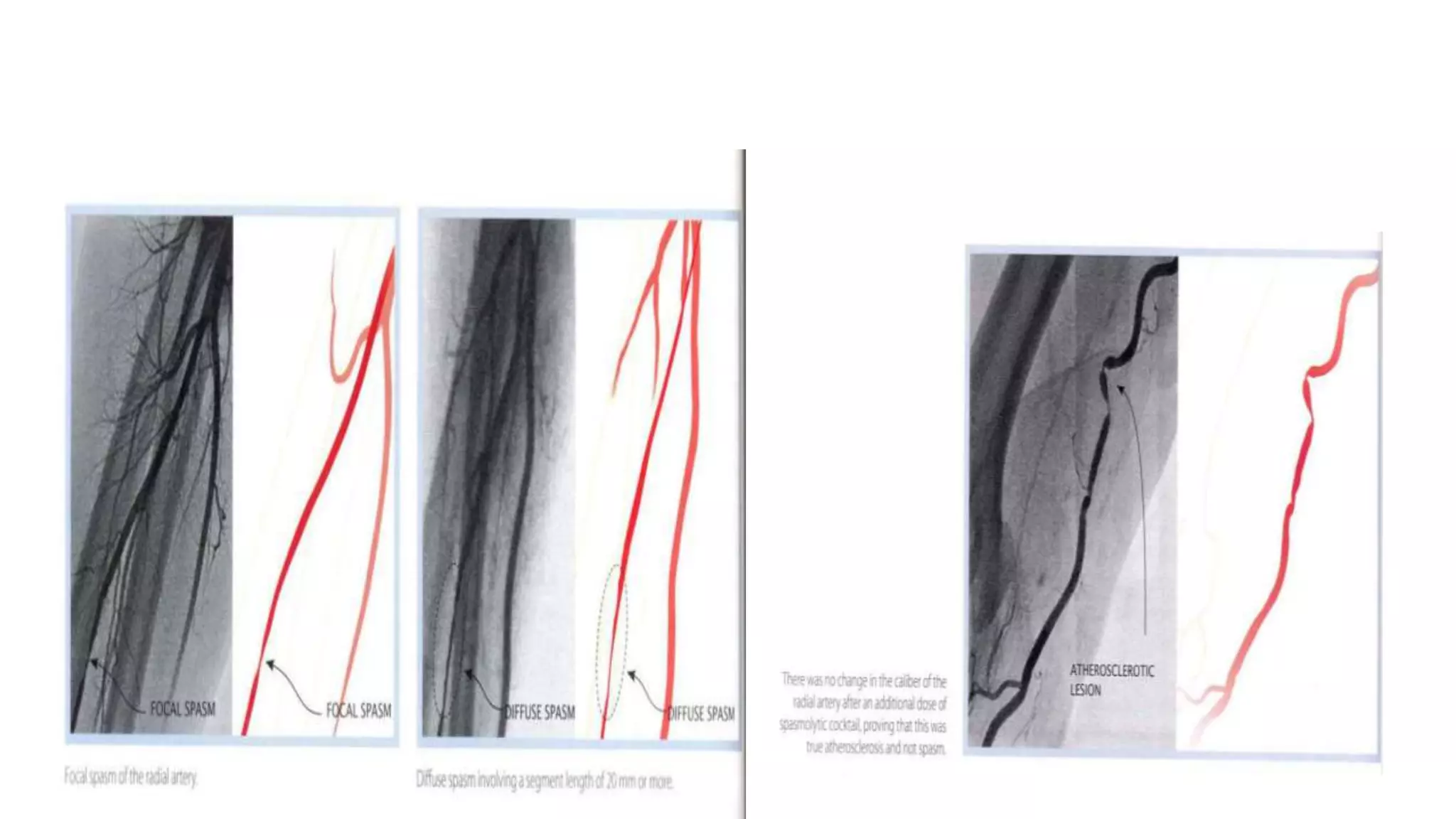
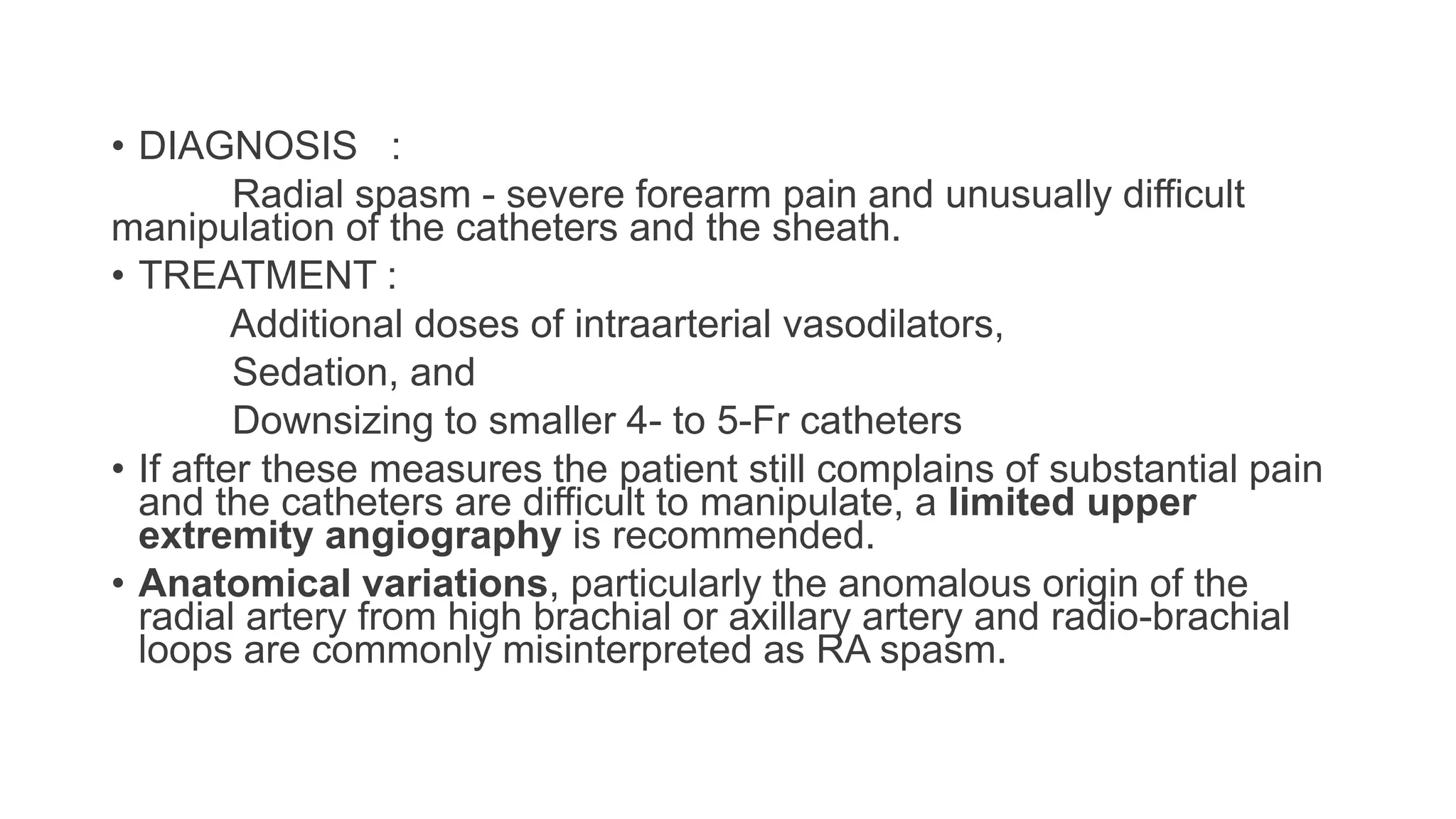
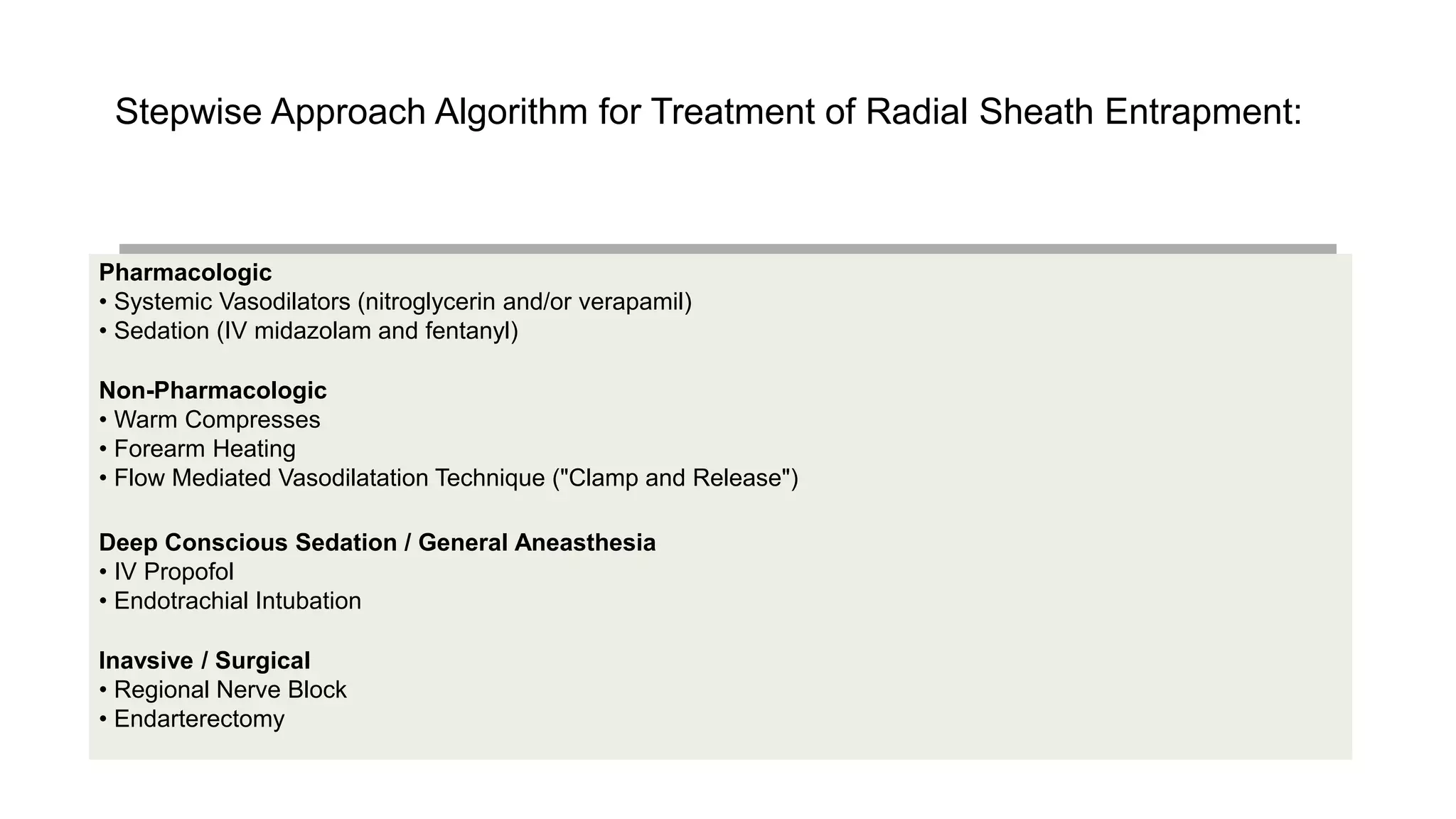
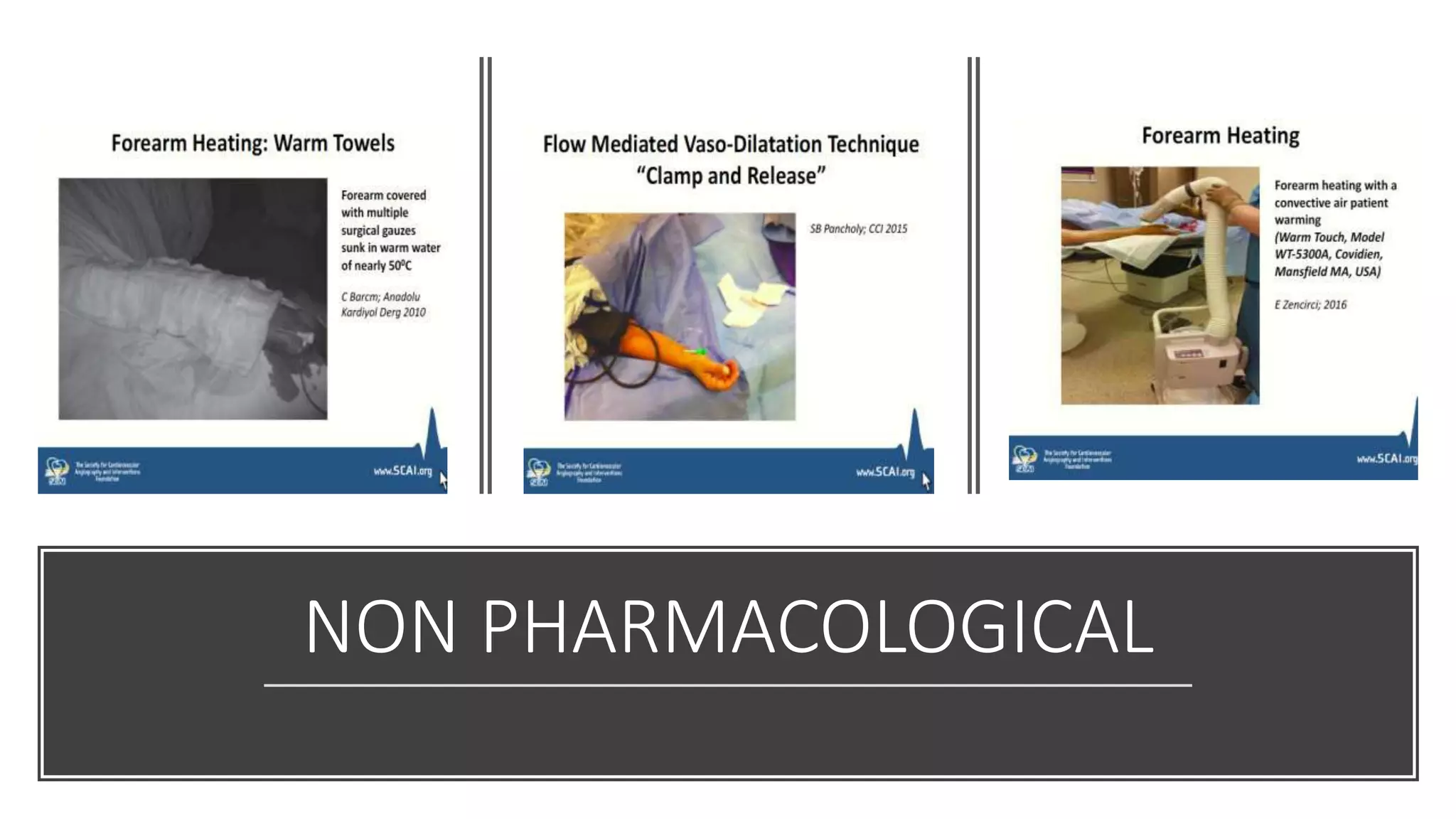
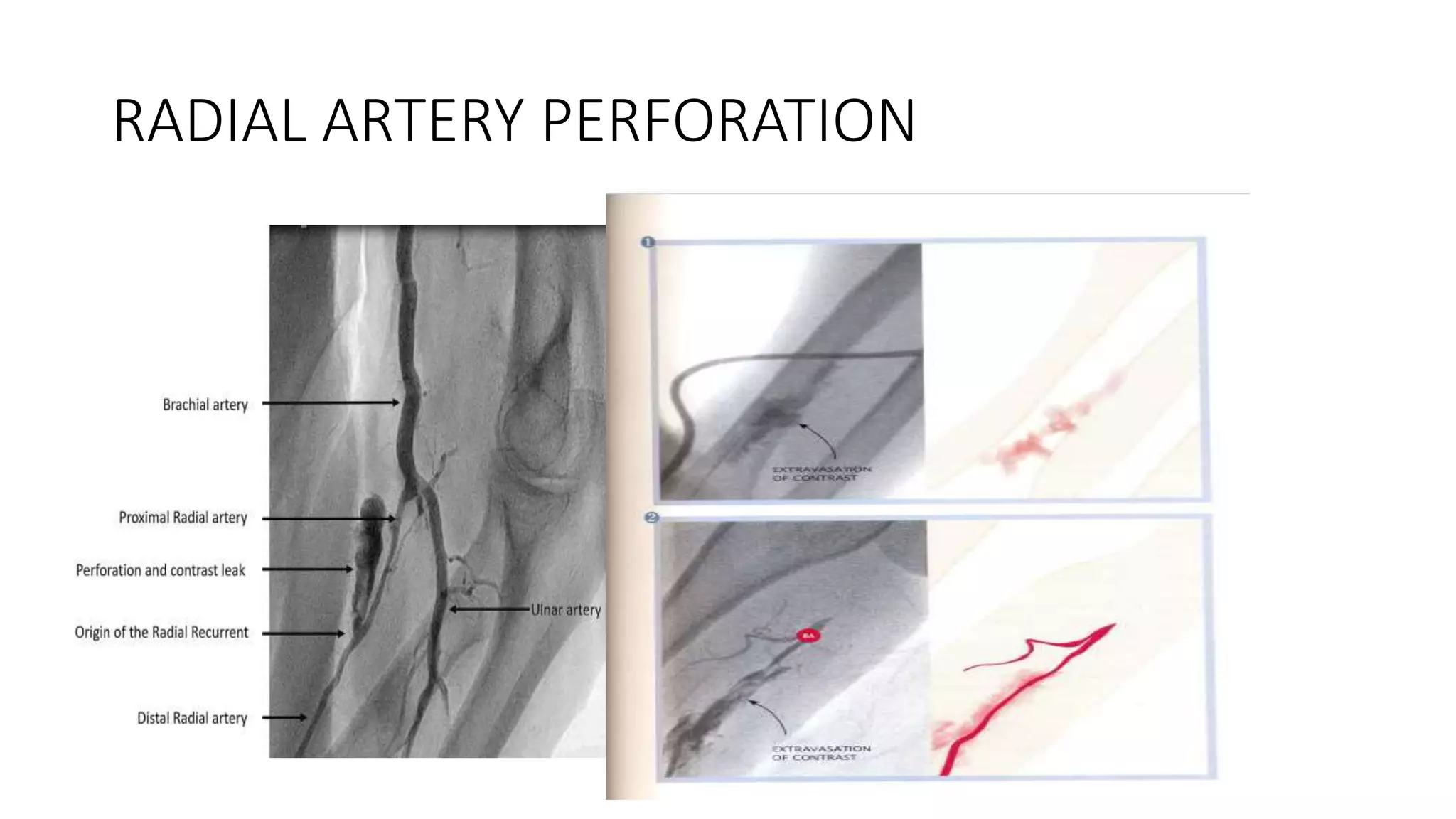
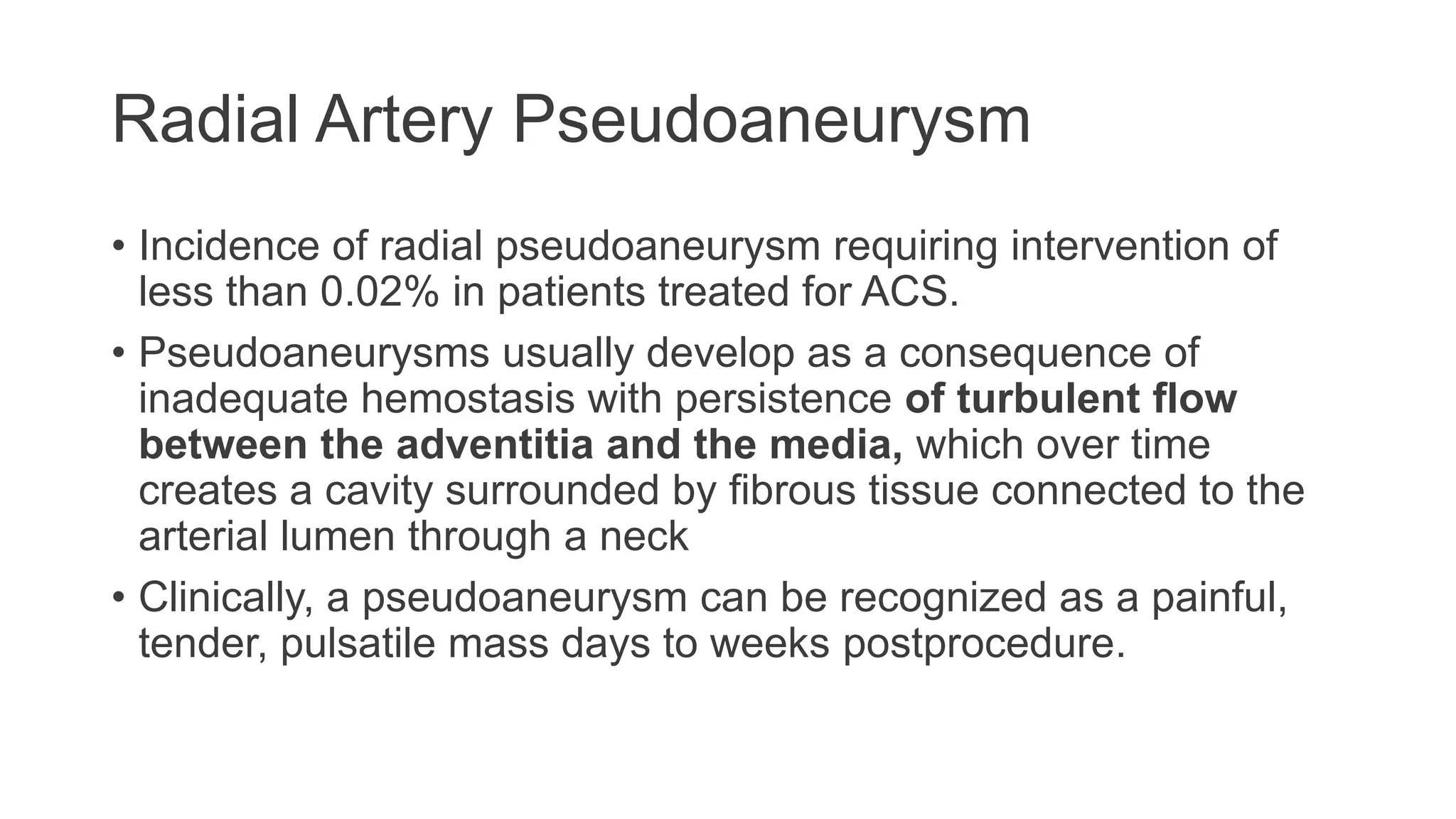
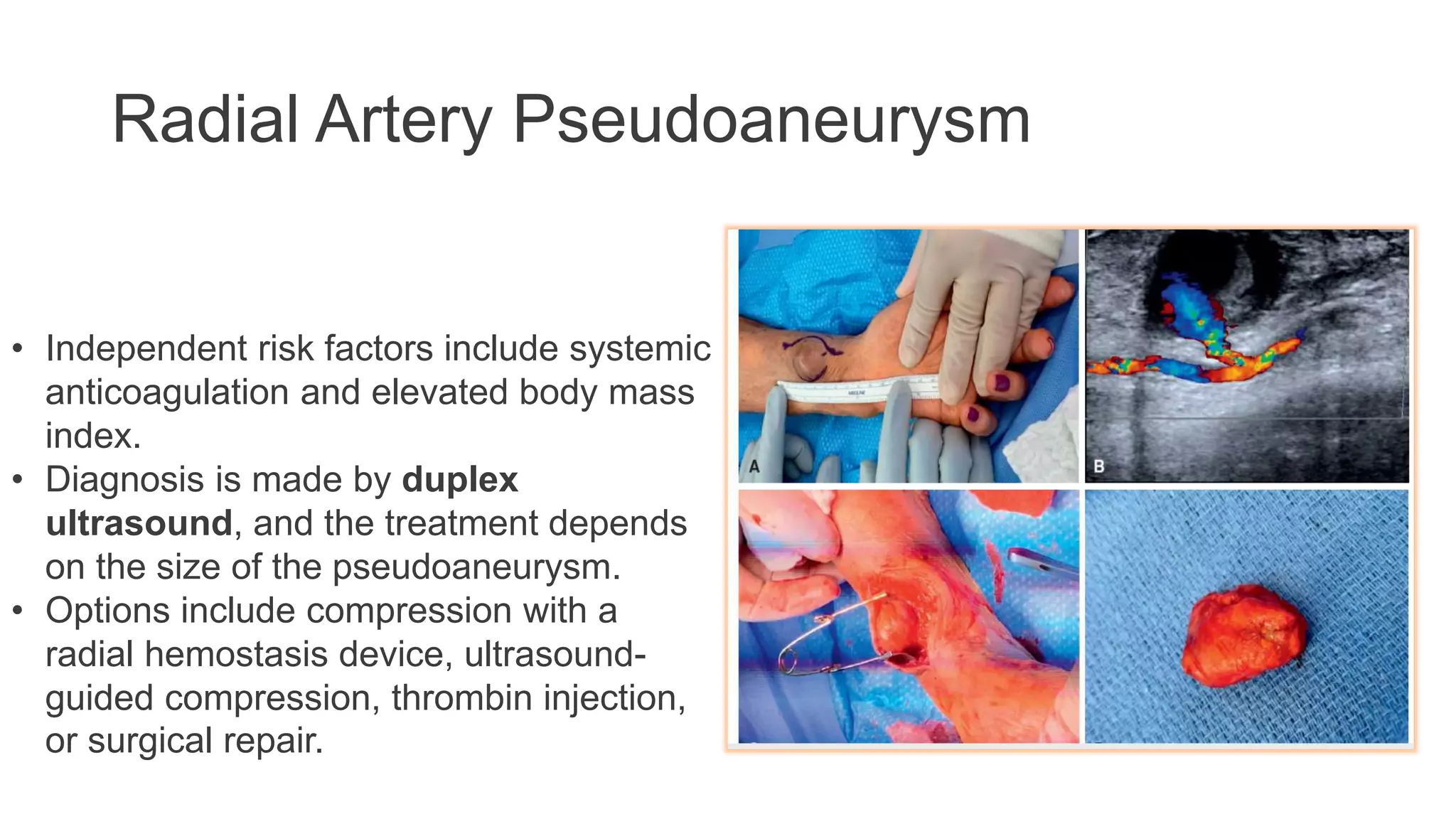
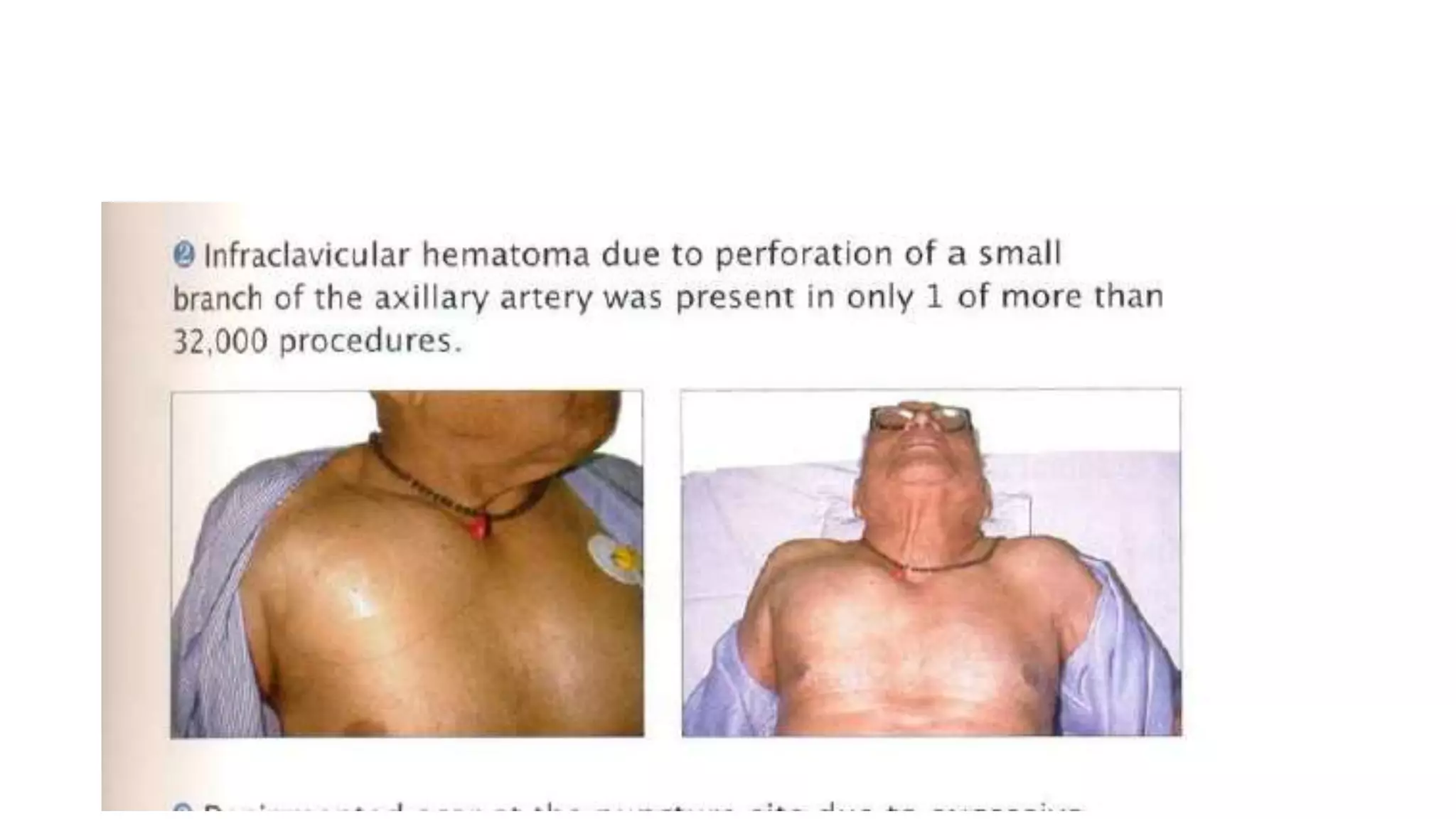
3. Radial artery puncture and navigation of wires and catheters through the arm requires specialized techniques to prevent complications like spasm or dissection.
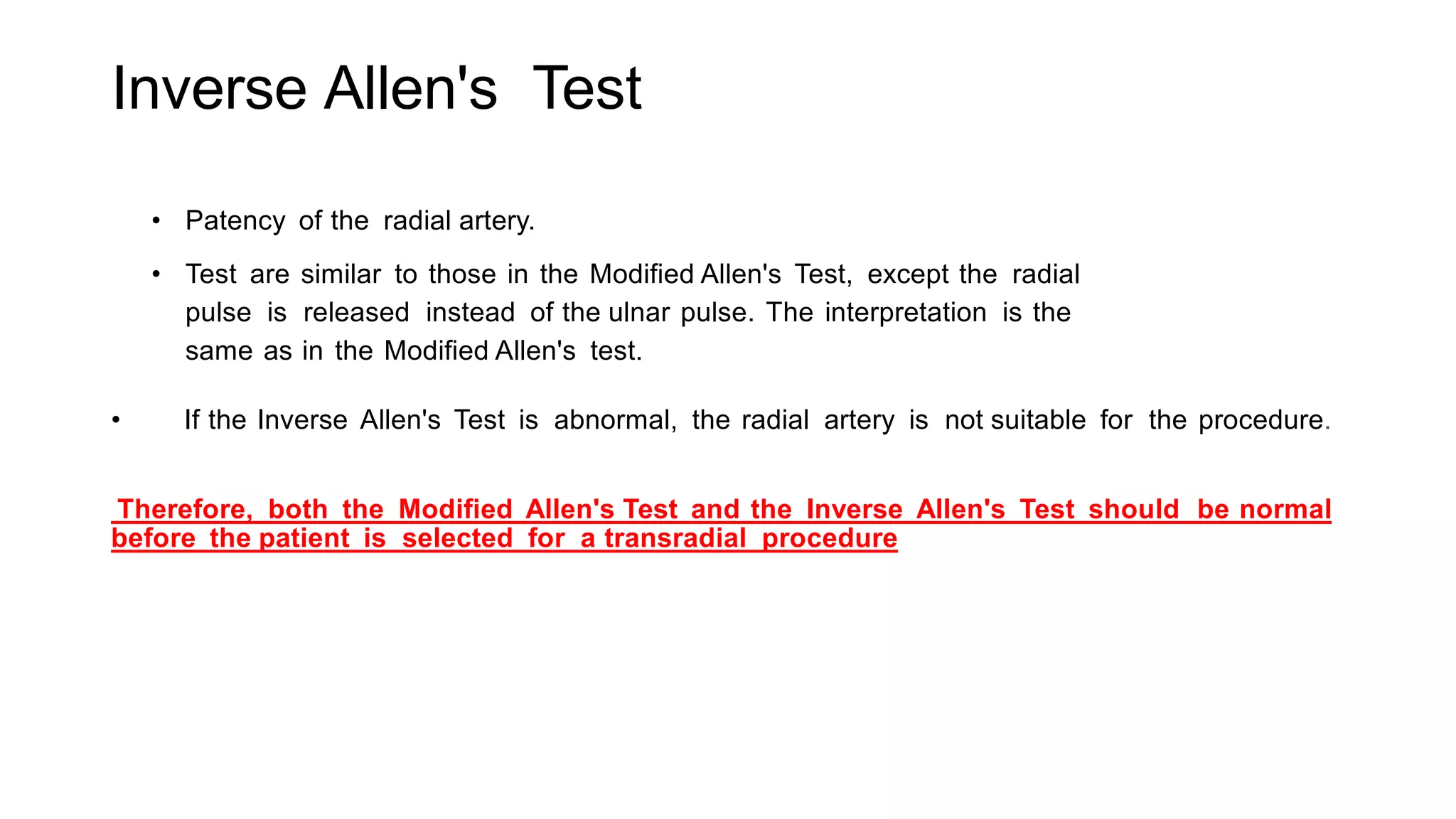
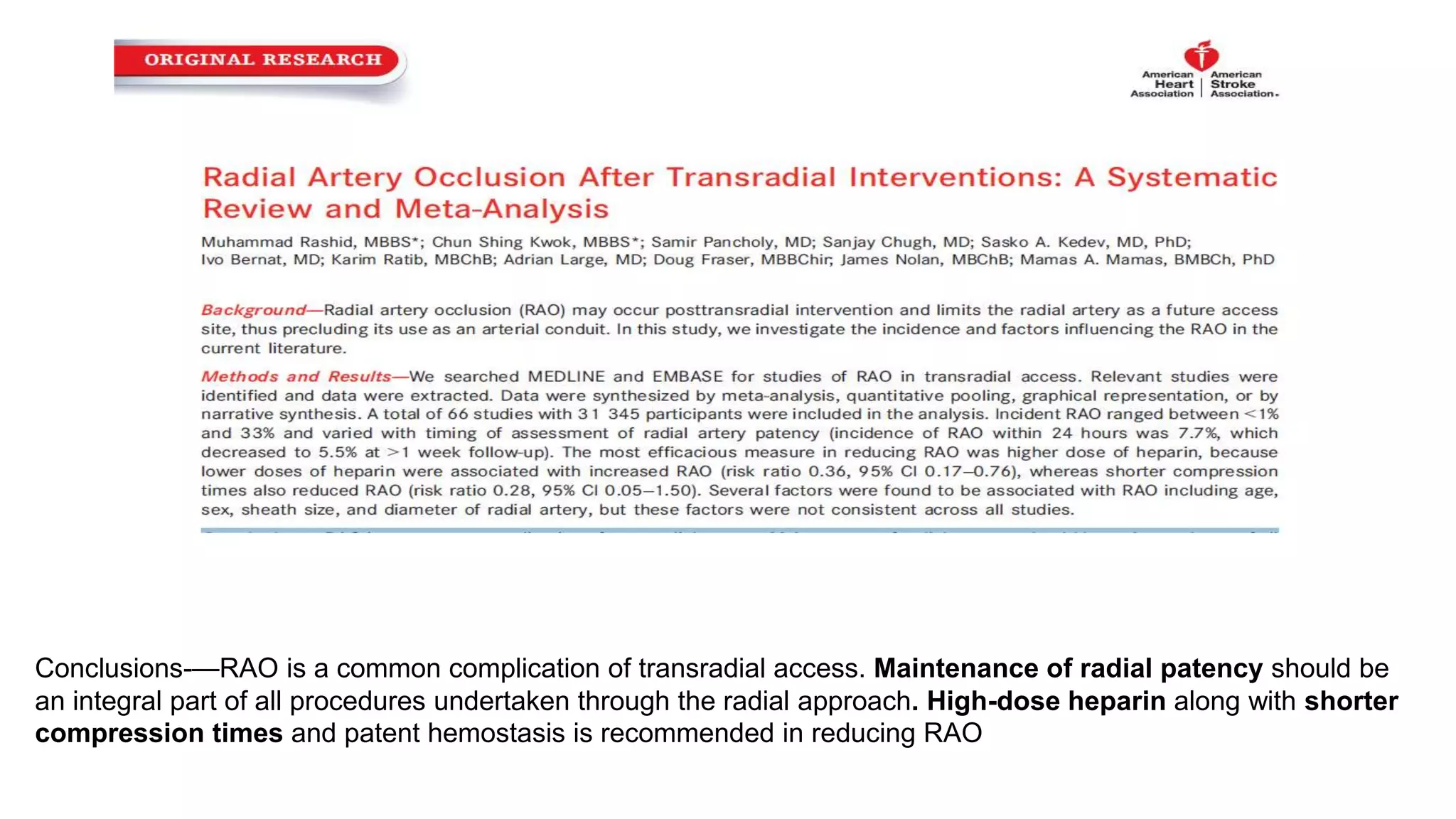
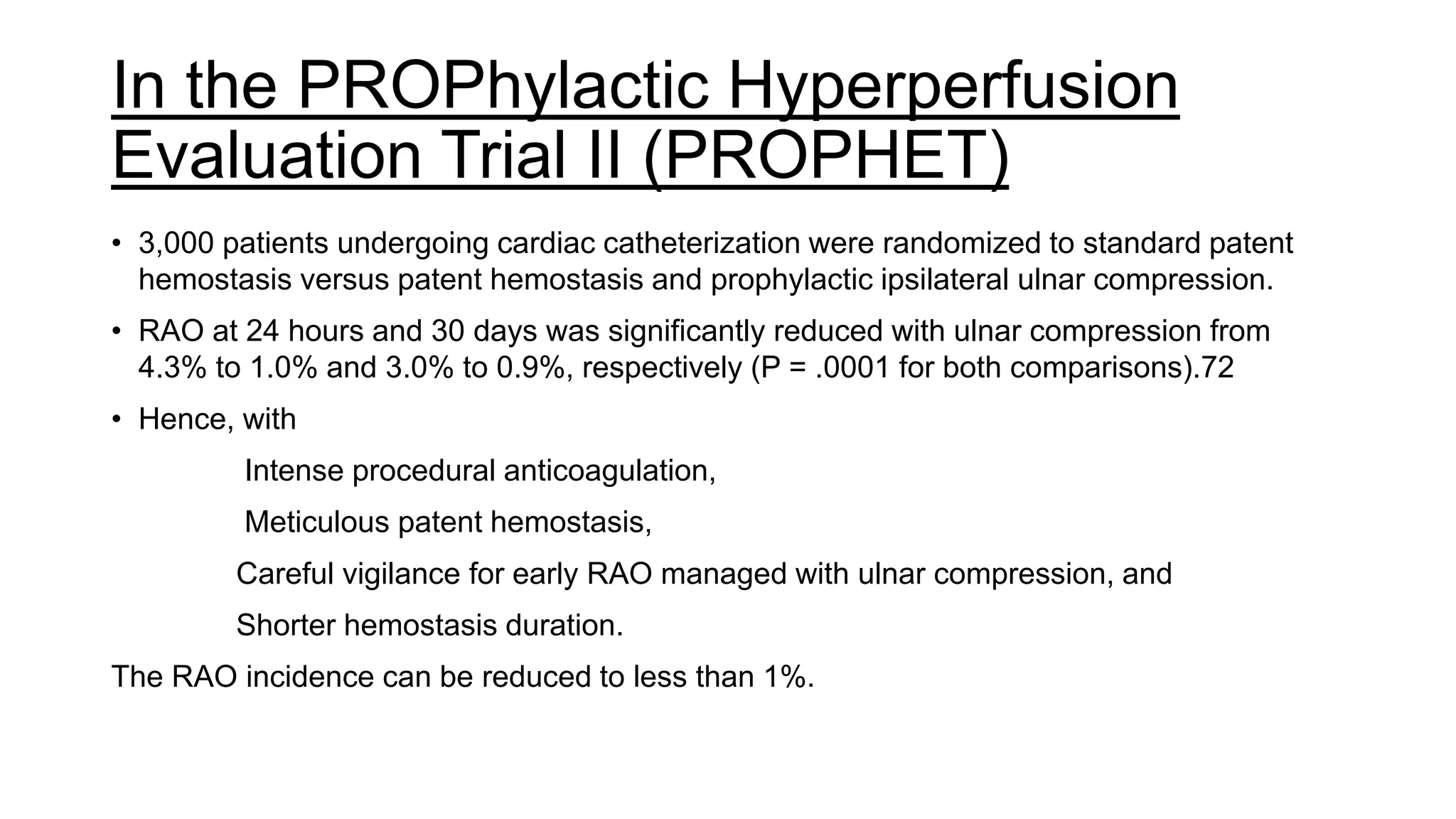
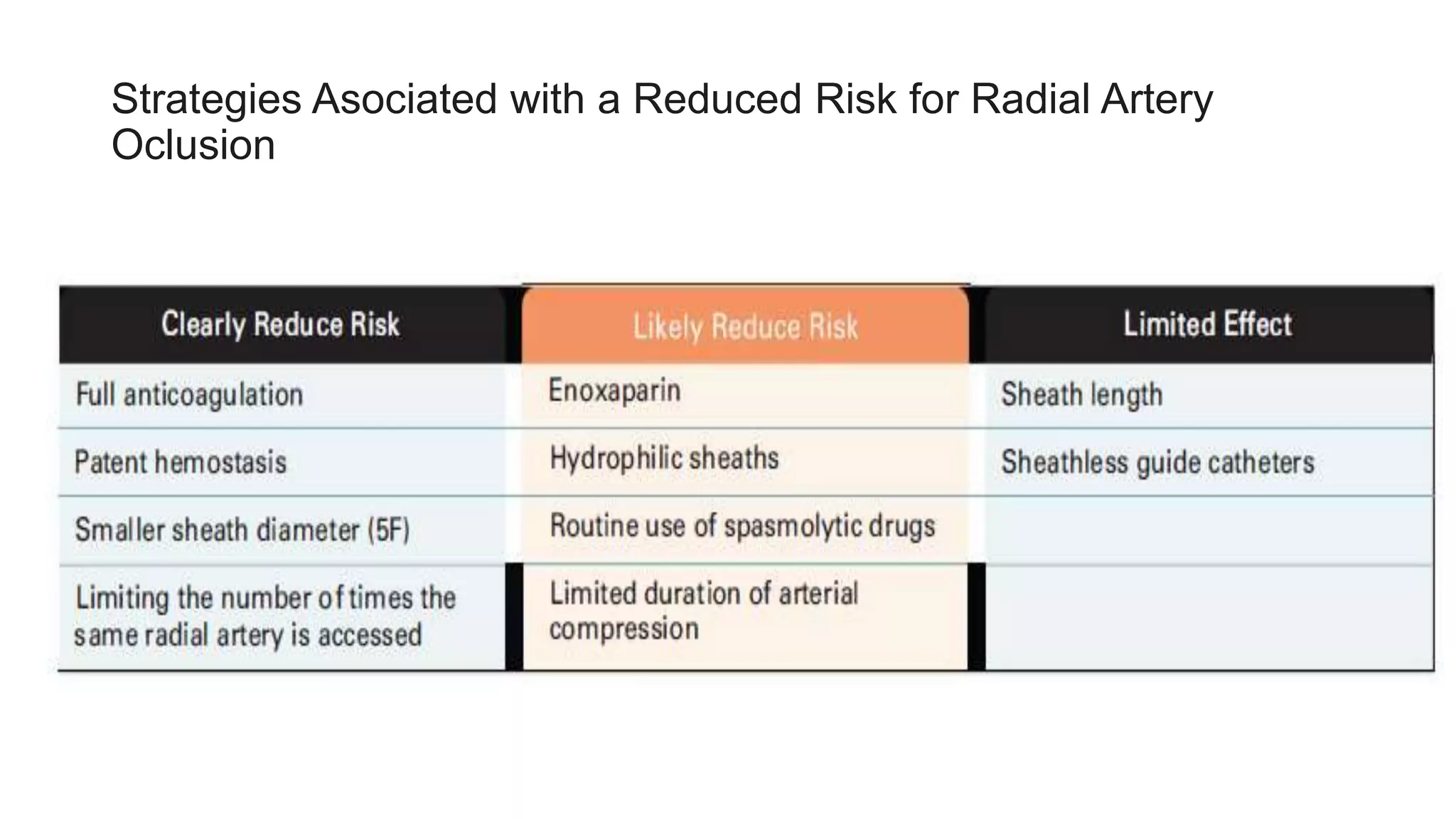
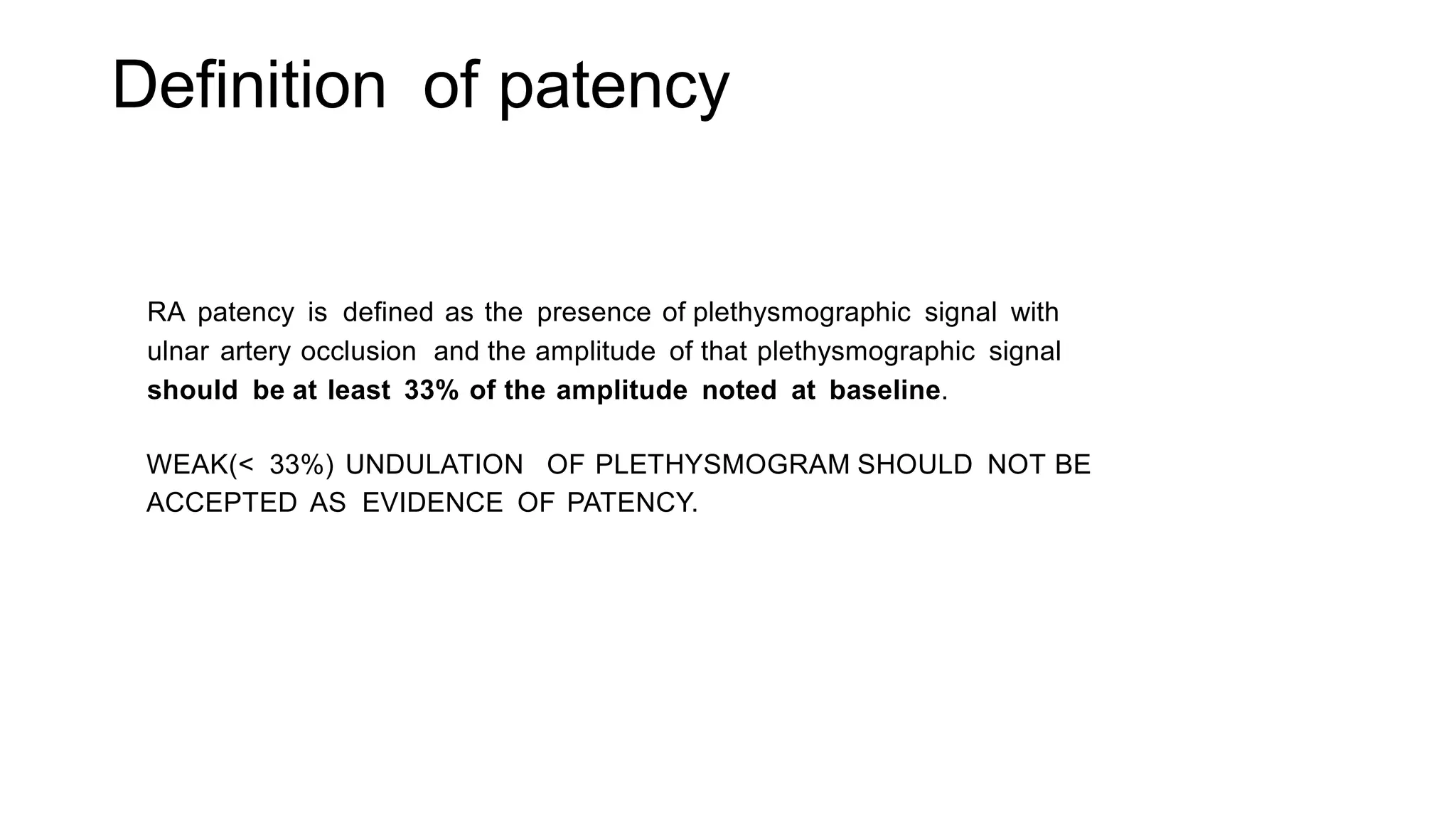
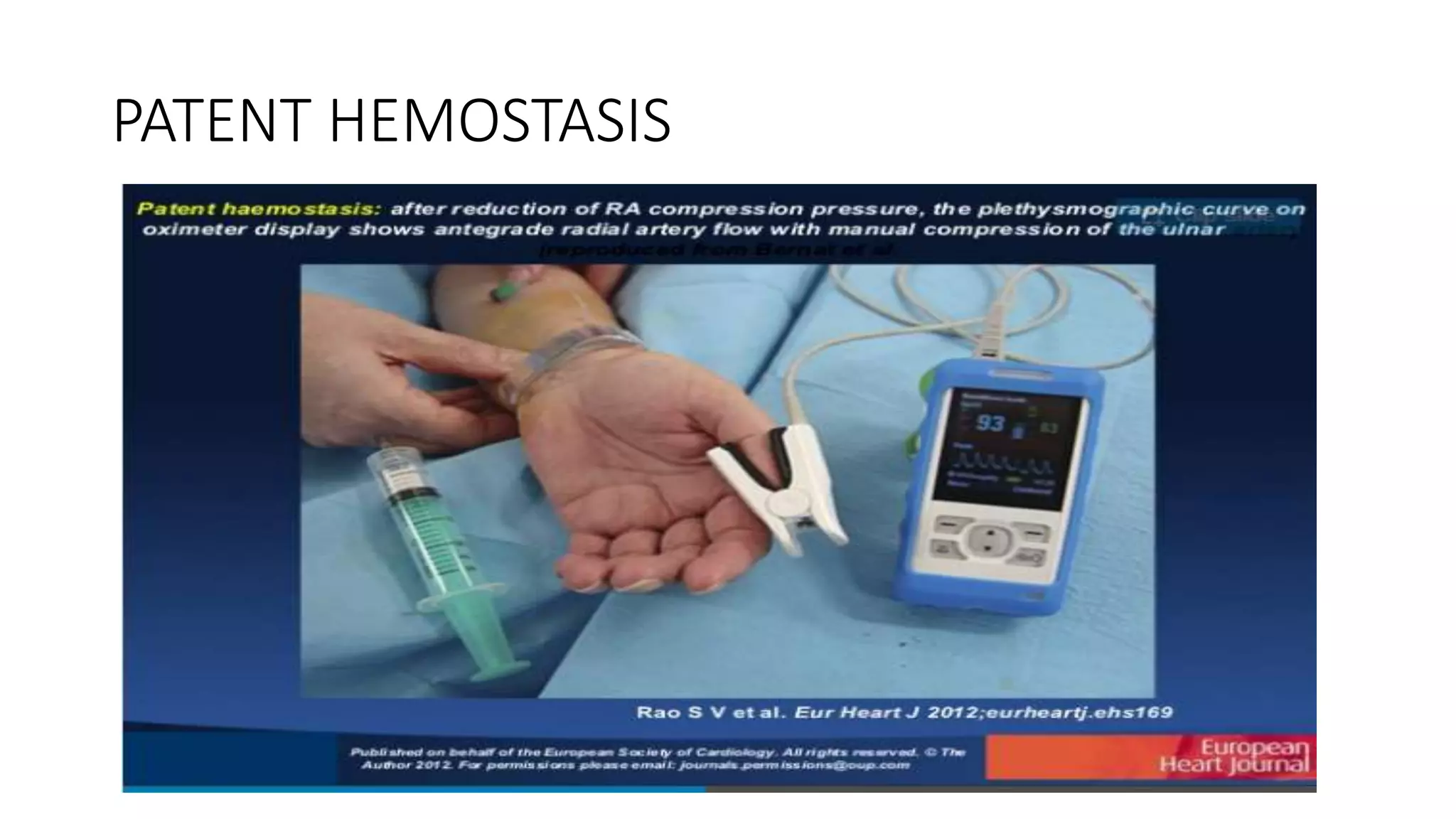
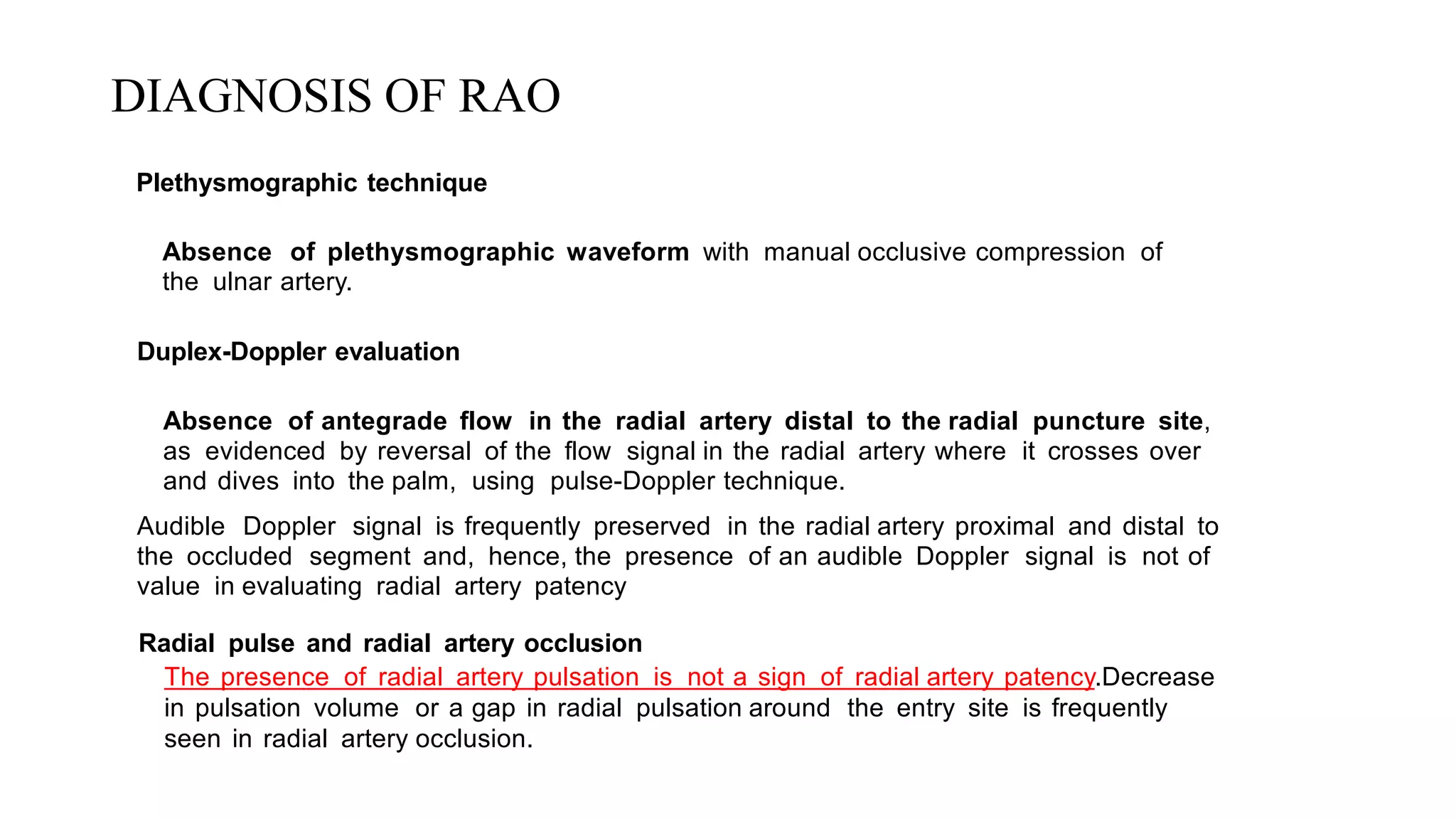
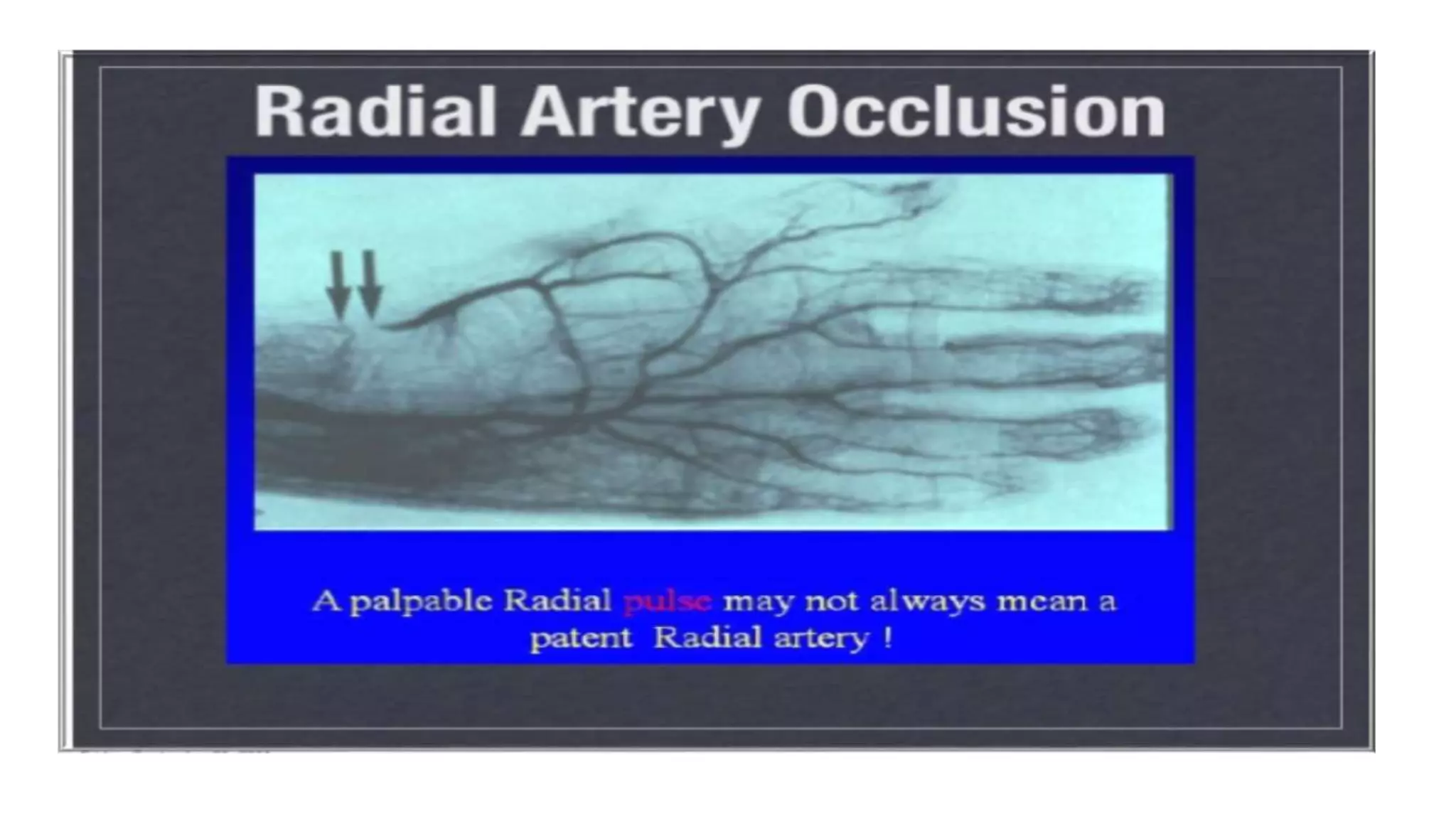
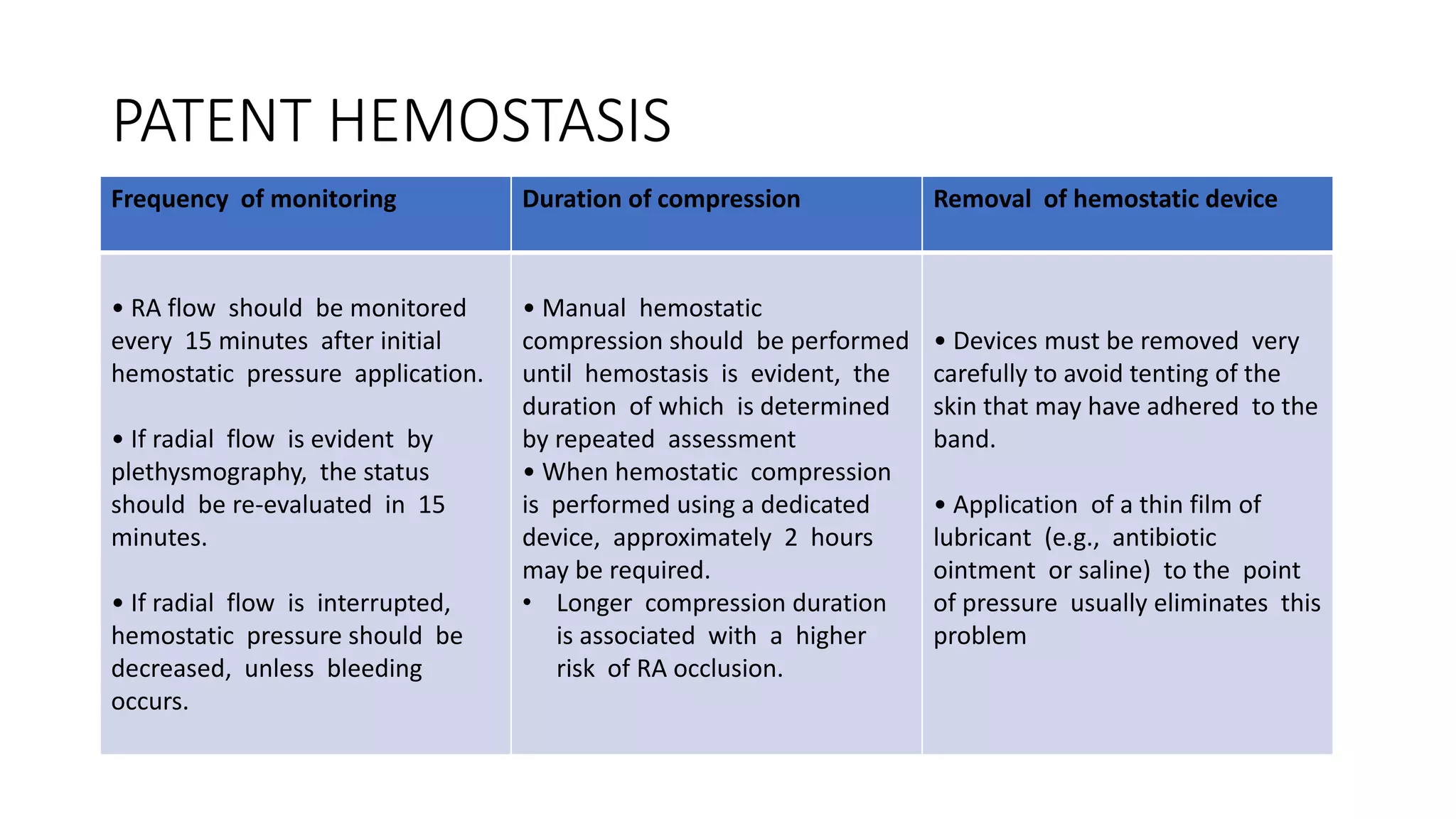
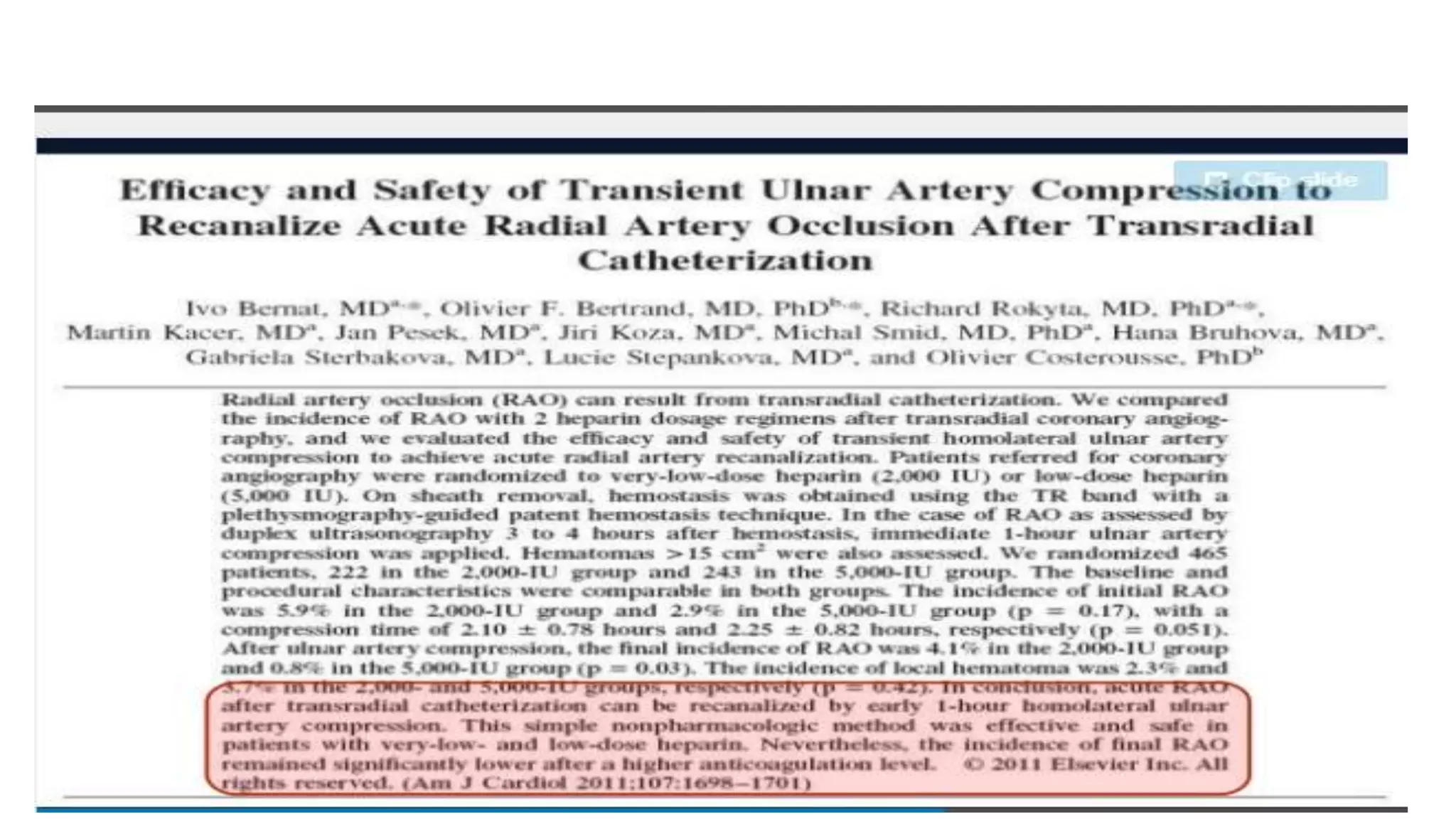
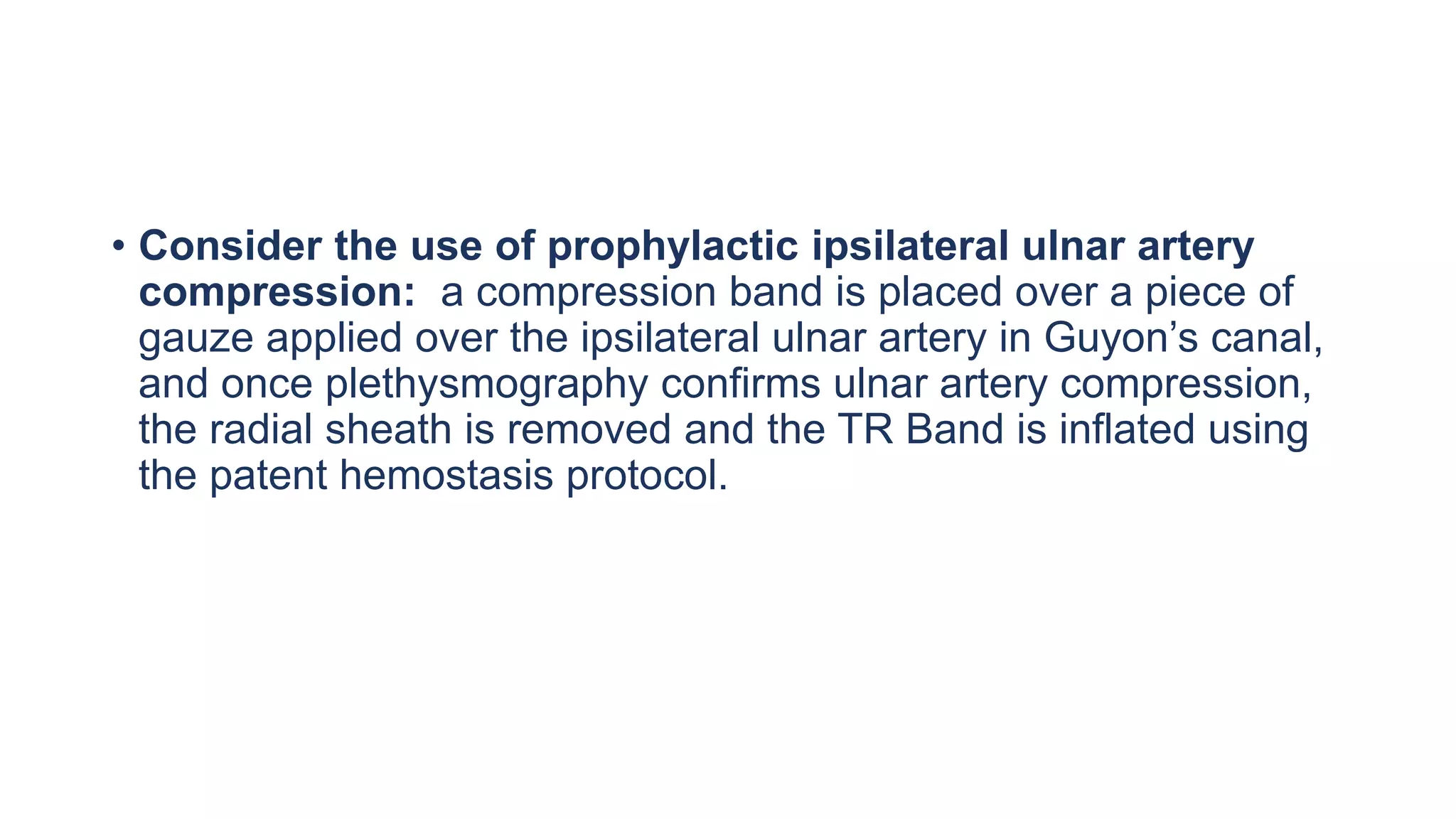
4. Maintaining radial artery patency with anticoagulation, proper compression, and monitoring is important to prevent radial artery occlusion following the procedure.