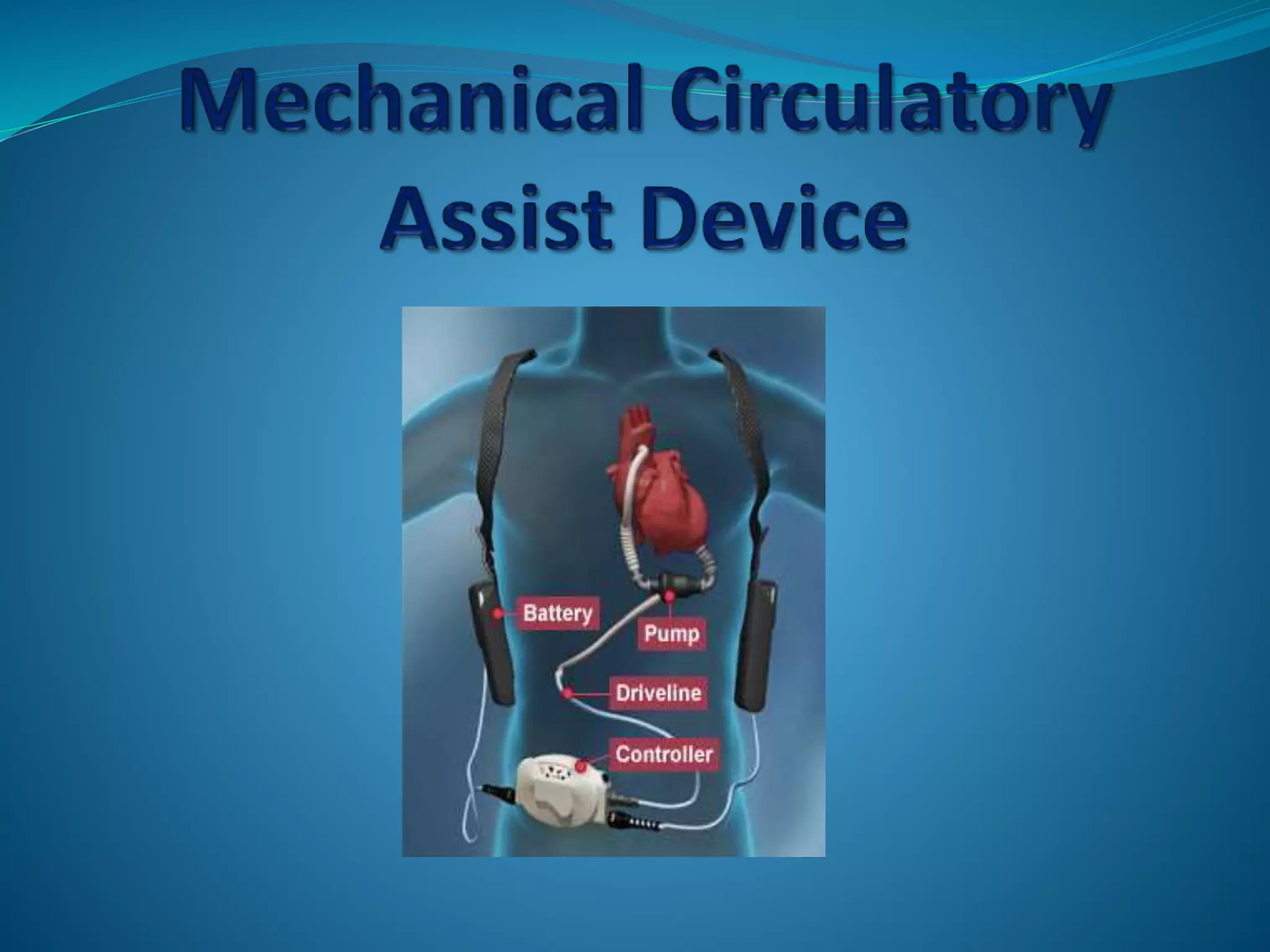
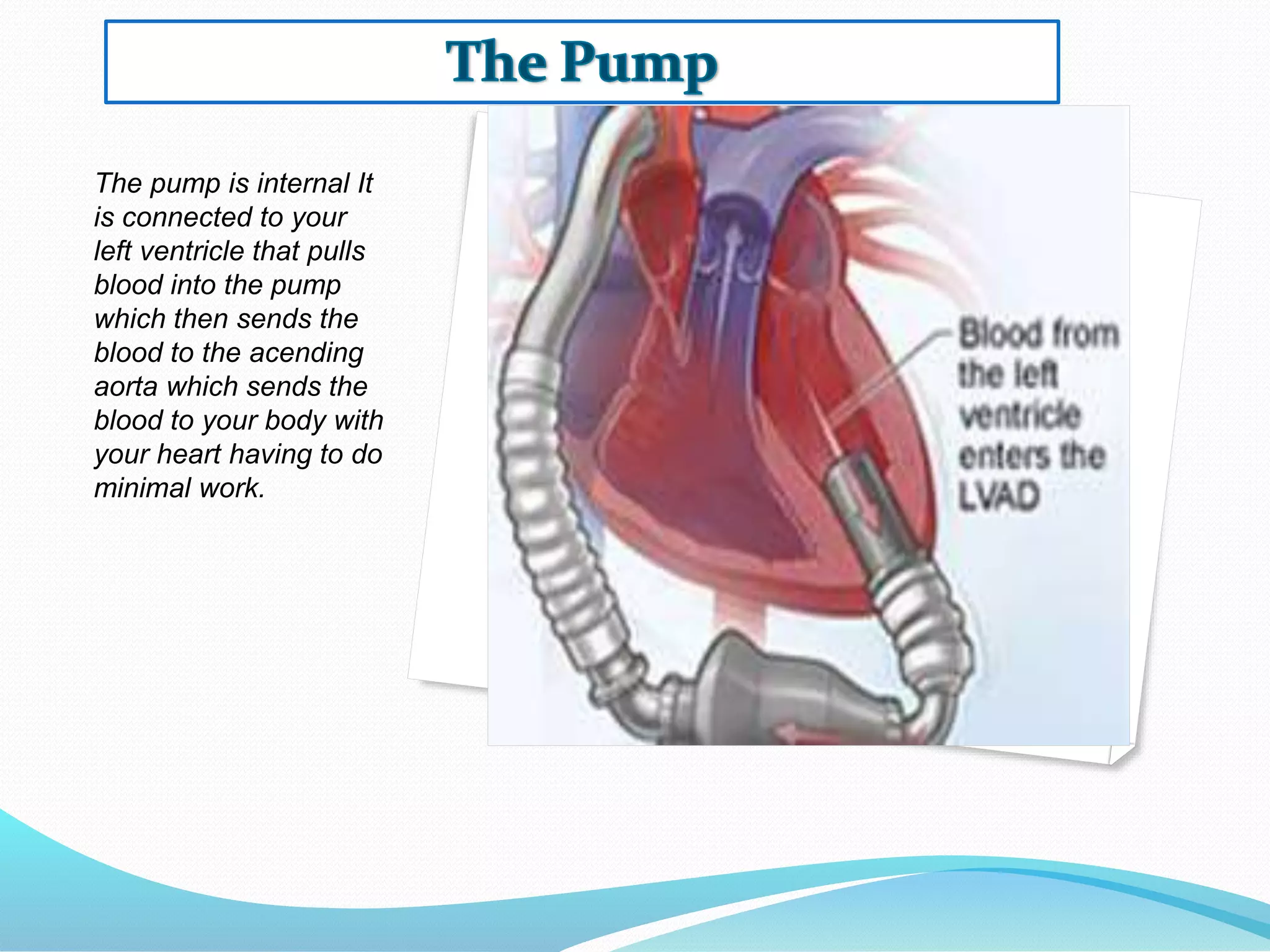
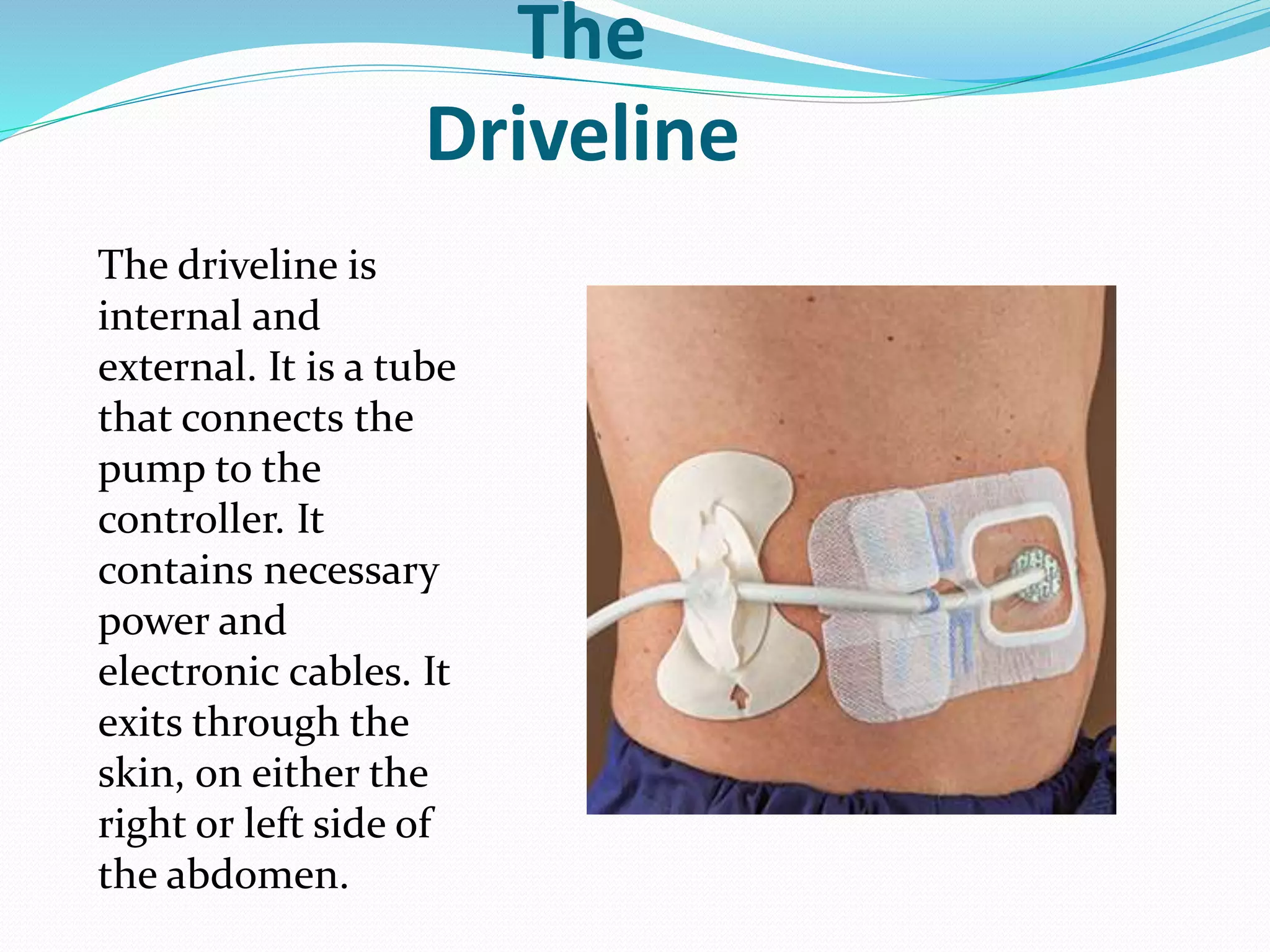
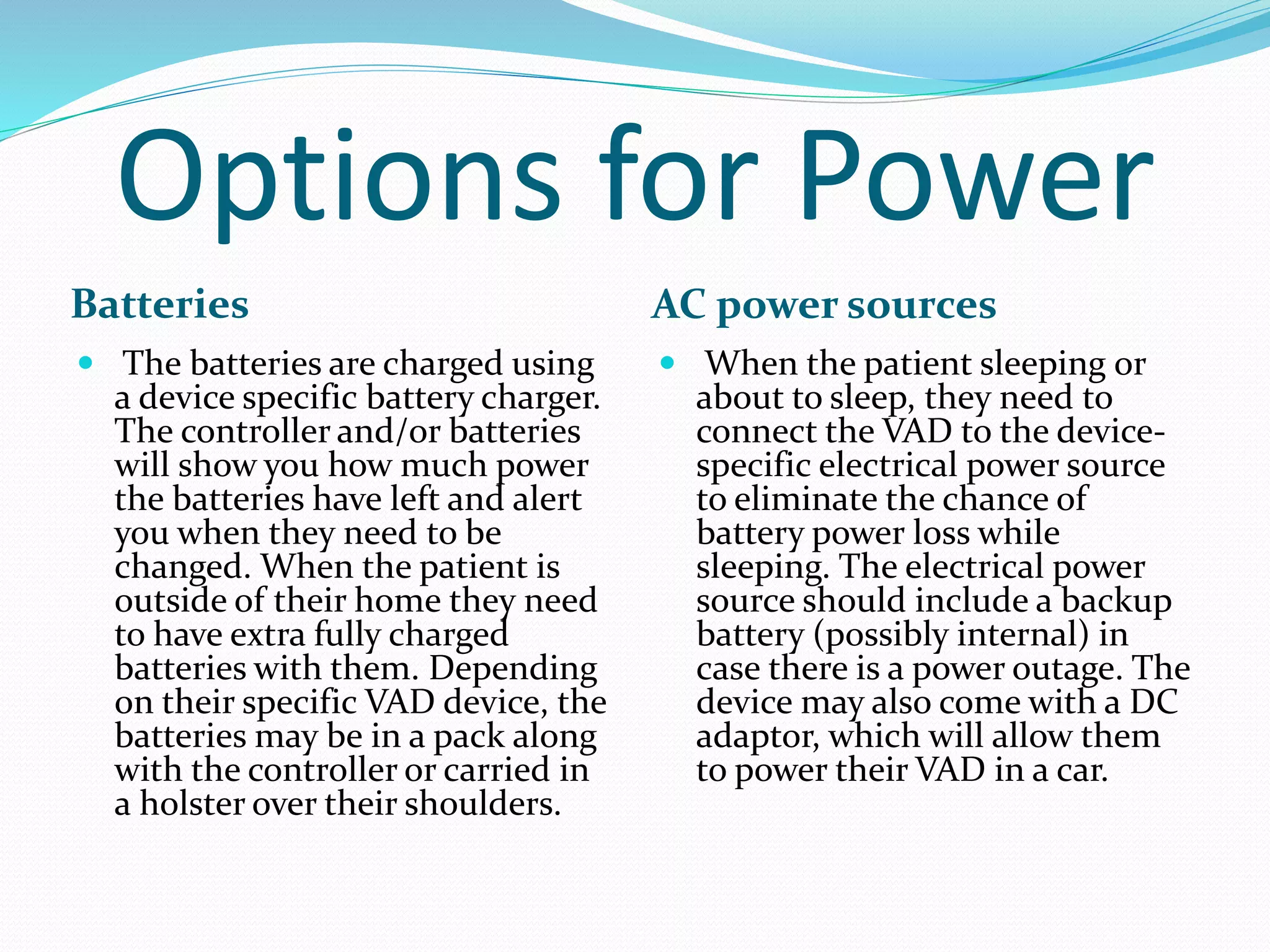
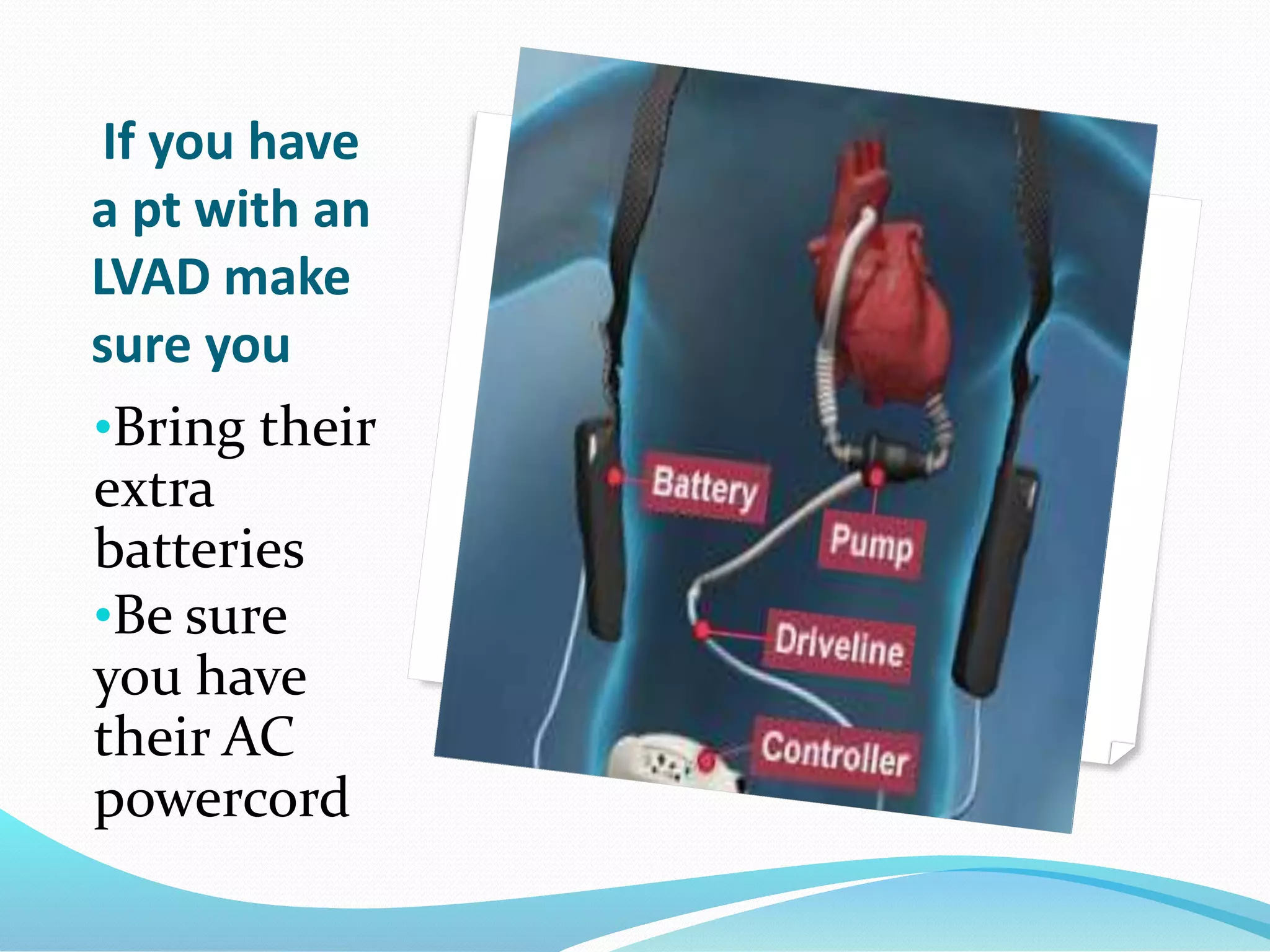
The Left Ventricular Assist Device (LVAD) is a mechanical pump that takes blood from the left ventricle of the weakened heart and pumps it to the body, similar to a normal heart. The LVAD has four main components - an internal pump, internal/external driveline, external controller, and batteries. The pump is placed in the heart and connected to the ventricle and aorta. The driveline connects the pump to the controller. The controller operates and monitors the pump. Batteries power the device and must be recharged. When assessing a patient with an LVAD, listen for pump sounds, check for alarms, identify the device type, treat any medical issues, and transport