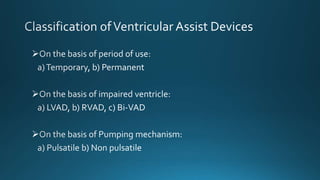
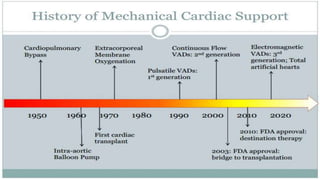
This document discusses left ventricular assist devices (LVADs) including:
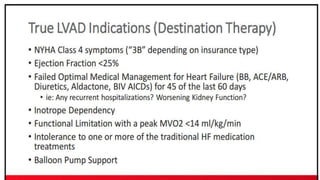
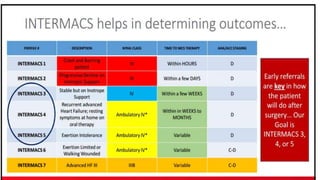
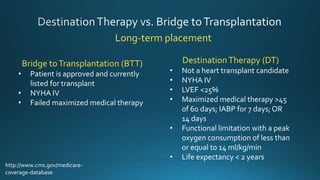
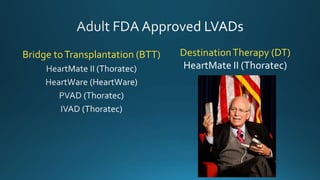
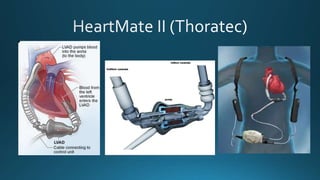
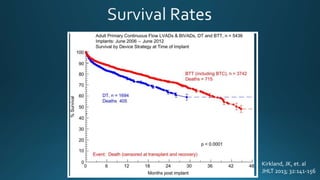
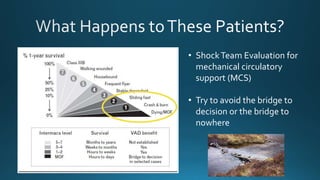
- Types of LVAD support including bridge to transplantation, destination therapy, and devices like the HeartMate II.
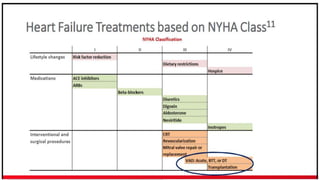
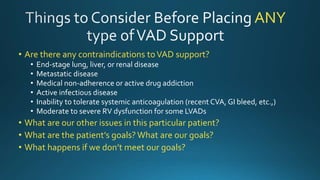
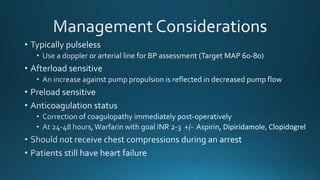
- Contraindications and patient criteria for LVAD support.
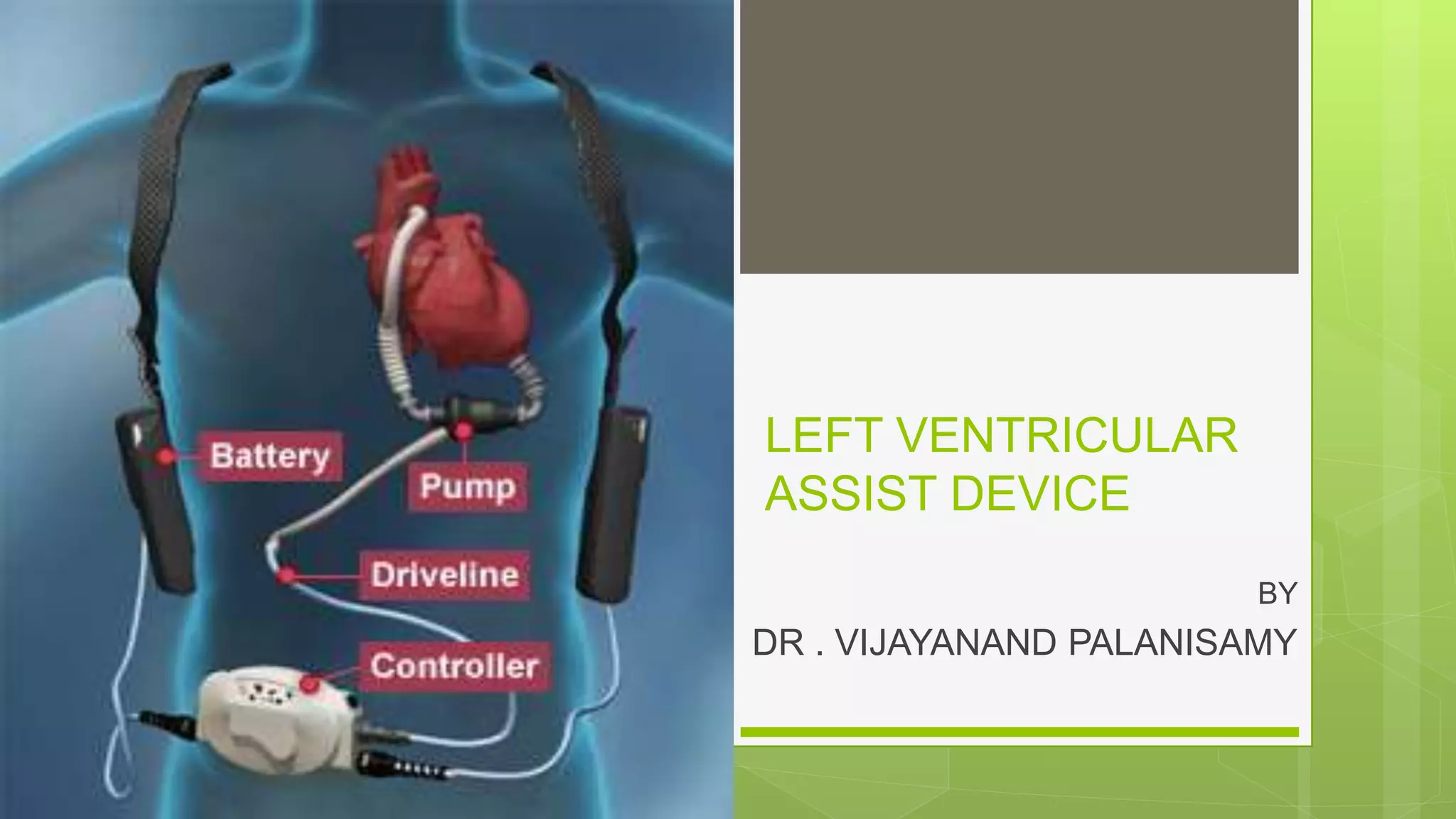
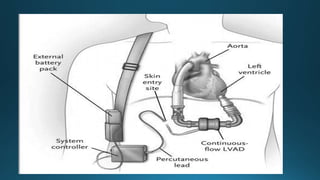
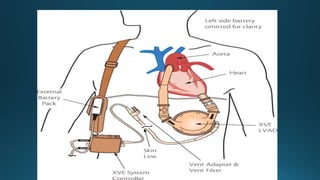
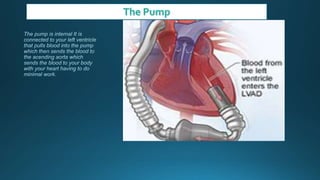
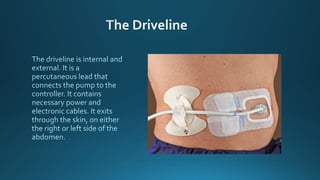
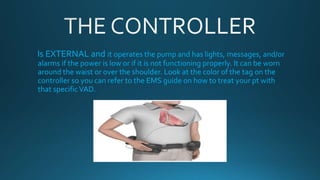
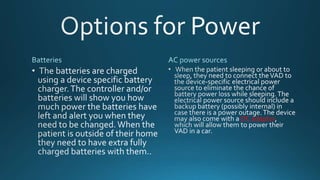
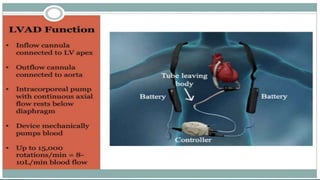
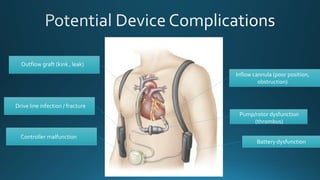
- Components and functions of the LVAD including the external controller.
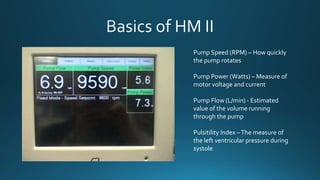
- Monitoring of pump parameters on the controller.
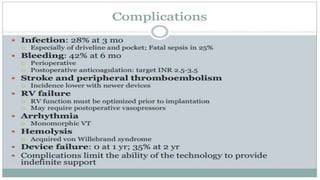
- Potential complications of LVAD support.
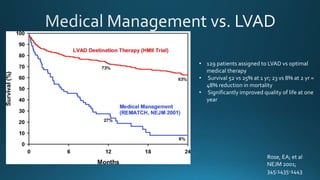
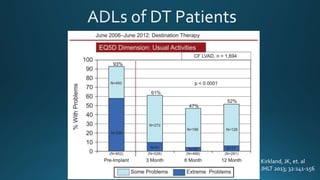
- Clinical trial results demonstrating improved survival and quality of life with LVADs.