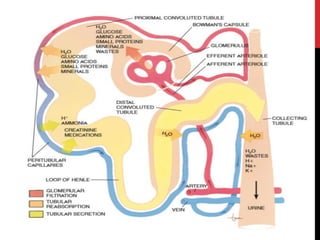
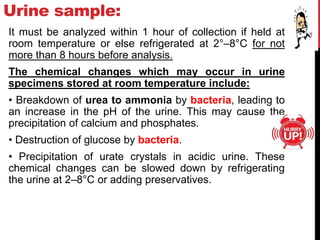
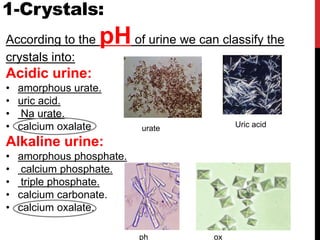
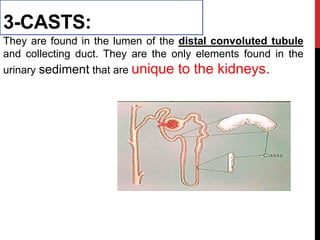
Urine analysis provides important information about kidney and metabolic function. A routine urinalysis includes physical, chemical, and microscopic examination of urine. The physical exam evaluates properties like color, clarity, specific gravity, and pH. The chemical exam checks for proteins, glucose, ketones, blood, and other substances. The microscopic exam identifies crystals, casts, epithelial cells, and other particles in the sediment. Abnormal findings can indicate conditions like urinary tract infections, kidney disease, or metabolic disorders.