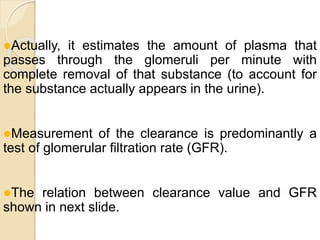
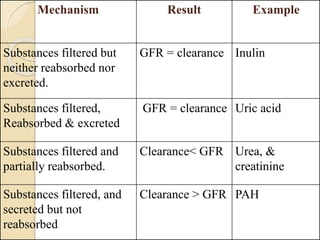
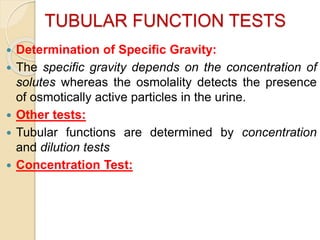
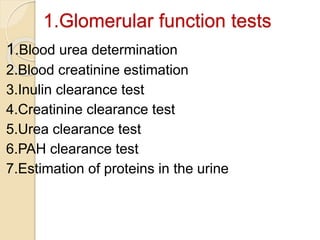
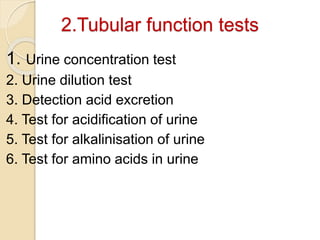
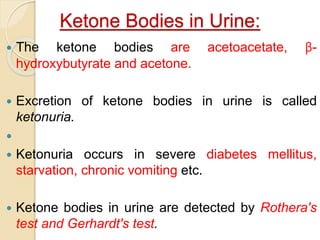
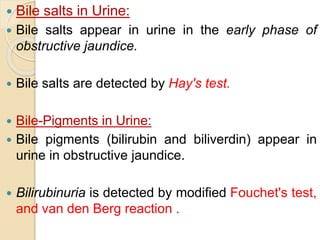
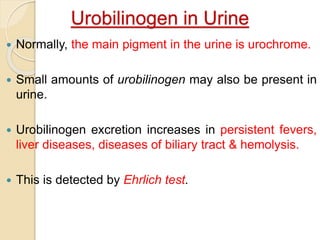
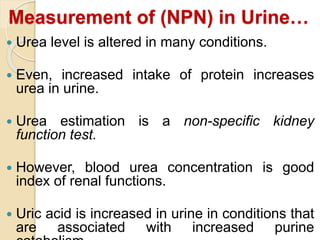
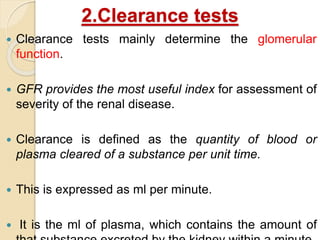
This document discusses kidney function tests which are divided into glomerular function tests and tubular function tests. Glomerular function tests like blood urea, creatinine, and clearance tests assess the kidney's filtering function. Tubular function tests like urine concentration, dilution, and acidification tests evaluate the kidney's reabsorptive and secretory abilities. Routine urine analysis includes examination of physical characteristics like volume, color, and odor as well as biochemical analytes like proteins, blood, glucose, and ketones. Clearance tests directly measure the glomerular filtration rate using calculations based on substance levels in plasma and urine.

![ Cs = Us × V
Ps
Cs = clearance rate of a substance ‘s’
Ps = plasma concentration of the
substance
Us = urine concentration of that
substance
V = urine flow rate[volume in ml/min]](https://image.slidesharecdn.com/kidneyfunctiontests2012-240403120455-2362533d/85/Kidney-Function-Tests2012-pptx-for-medical-23-320.jpg)