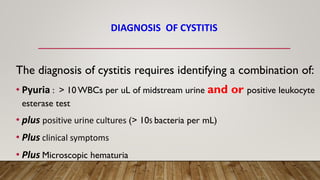
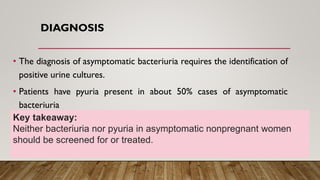
This document summarizes urinary tract infections including cystitis, pyelonephritis, asymptomatic bacteriuria, and prostatitis. It describes the anatomy of the urinary tract and defines the different types of urinary tract infections. It discusses the typical causative agents, risk factors, clinical presentations, diagnoses, and treatment approaches for each type of infection. The most common pathogen is E. coli and treatment involves antibiotics that can achieve high concentrations in the renal parenchyma like fluoroquinolones and third generation cephalosporins. Asymptomatic bacteriuria generally does not require treatment except in special populations.