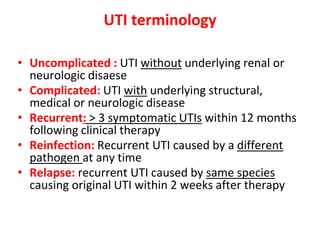
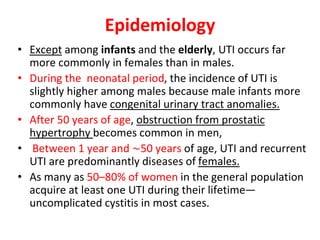
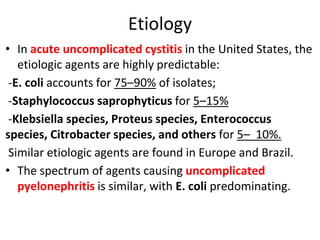
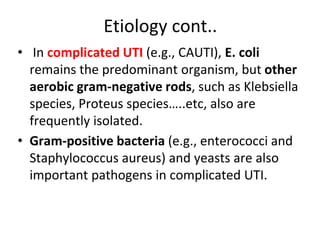
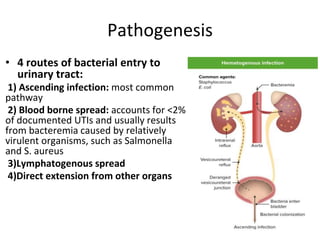
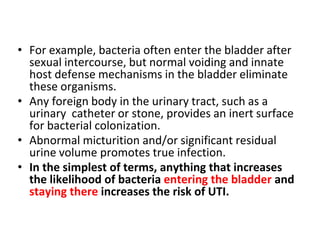
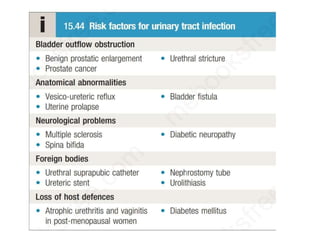
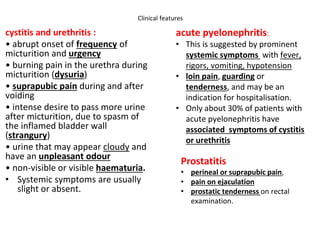
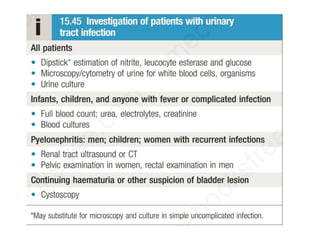
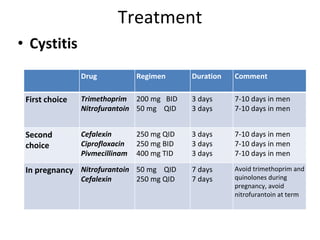
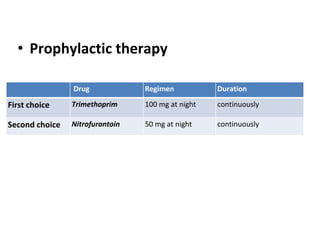
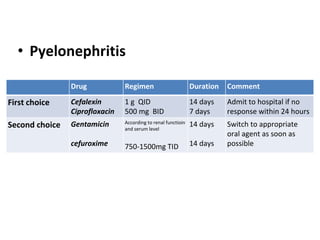
Urinary tract infections (UTIs) are caused by bacteria entering the urinary tract. Escherichia coli is the most common cause of uncomplicated UTIs. UTIs are classified as upper (e.g. pyelonephritis) or lower (e.g. cystitis, urethritis) and can be complicated or uncomplicated. Symptoms depend on the site of infection but often include pain or burning during urination. Treatment involves antibiotics, with choices depending on the type and severity of the UTI. Prophylactic antibiotics may be used for recurrent UTIs.