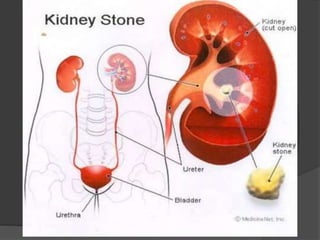
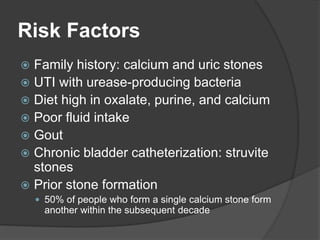
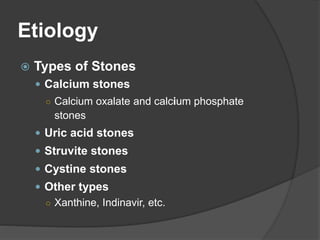
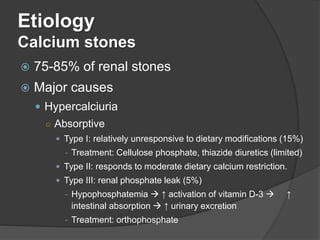
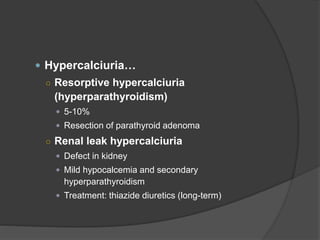
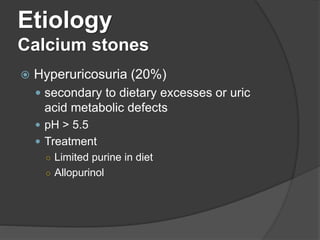
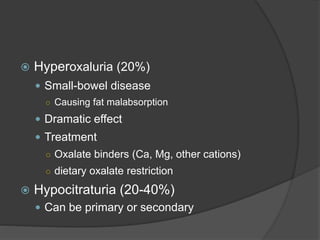
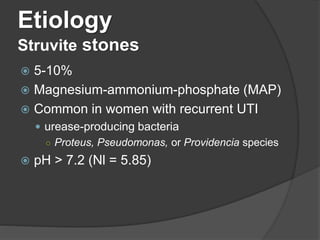
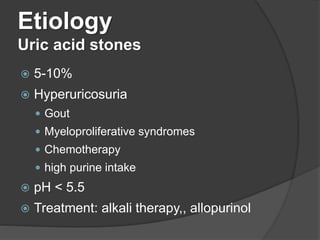
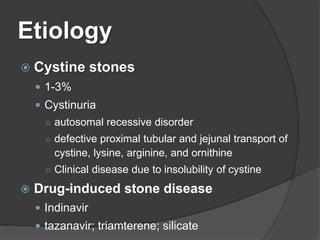
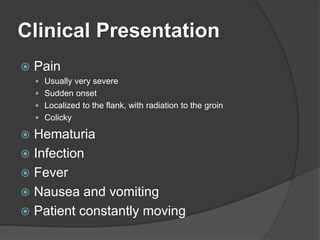
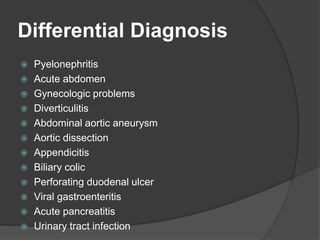
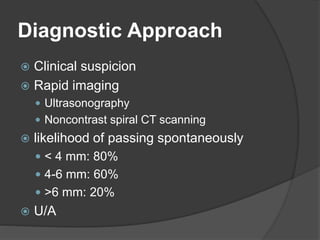
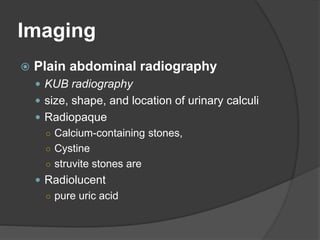
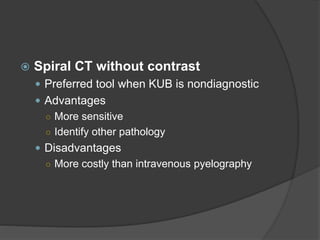
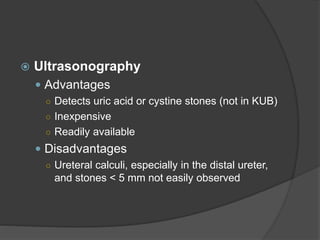
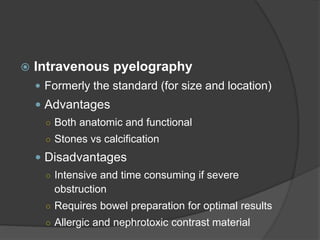
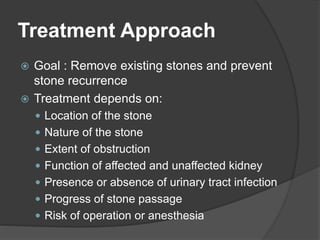
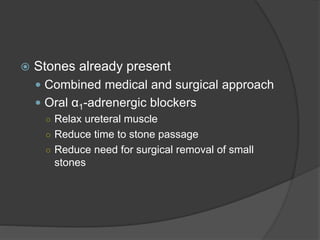
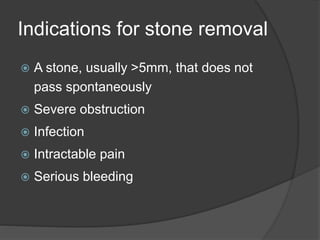
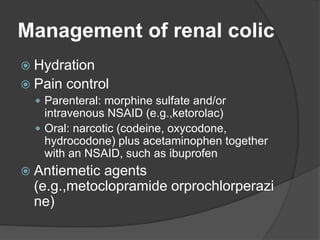
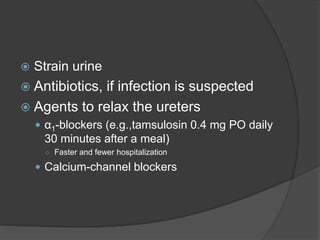
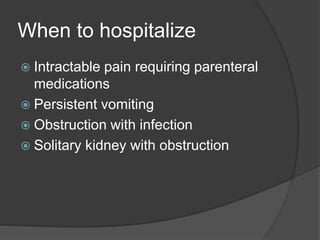
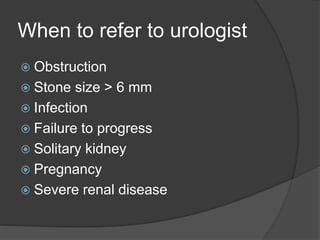
The document discusses kidney stones, which are solid, crystalline concretions that can cause pain and obstruction, with an increasing prevalence in the industrialized world. It outlines the various types, risk factors, and diagnostic approaches for kidney stones, as well as treatment options that include hydration, pain management, and potential surgical intervention. Key factors influencing stone composition, clinical presentation, and indicators for hospitalization and referral to a urologist are also addressed.