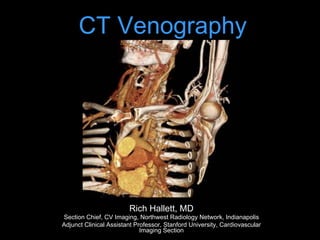
CT venography is a technique used to assess venous anatomy and determine patency. It can be performed using direct or indirect methods. Direct CTV involves slowly infusing diluted contrast directly into veins of interest. Indirect CTV uses a larger bolus of full-strength contrast followed by a delayed scan to image recirculating contrast in the veins. CTV provides non-invasive evaluation of venous anatomy from the upper extremities to the pelvis with good spatial resolution and ability to combine with arterial imaging. It is useful for evaluating issues like deep vein thrombosis, thoracic outlet syndrome, and superior vena cava syndrome.