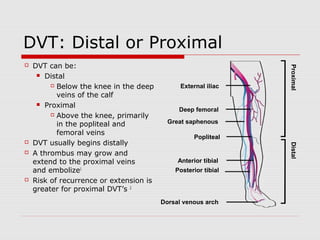
This document discusses the diagnostic and treatment approaches to venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE). It provides details on evaluating patients using Wells criteria and D-dimer testing to determine pre-test probability and decide between imaging with CT pulmonary angiogram or VQ scan. For confirmed VTE, treatment options include warfarin, novel oral anticoagulants (NOACs), inferior vena cava filters or thrombolytics. The document reviews best practices for treating isolated distal DVT, catheter-related thrombosis, and selecting appropriate long-term anticoagulation therapy.