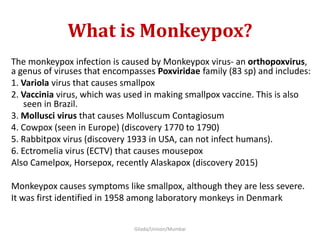
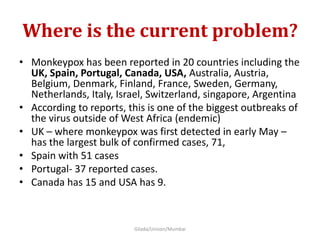
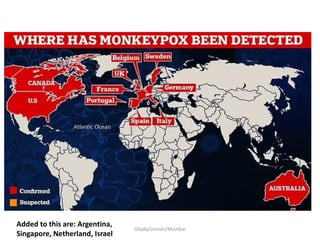
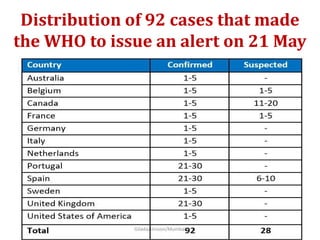
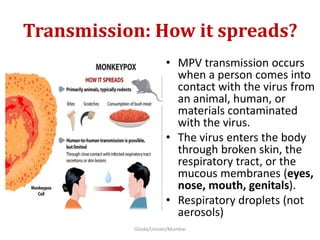
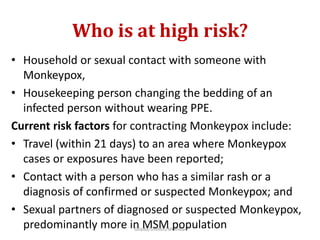
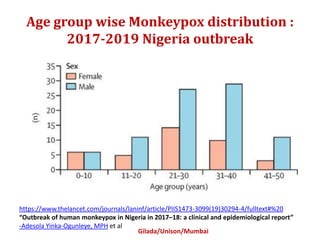
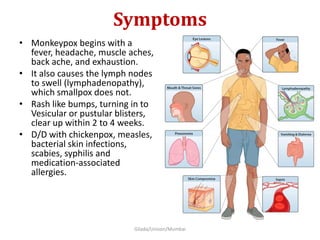
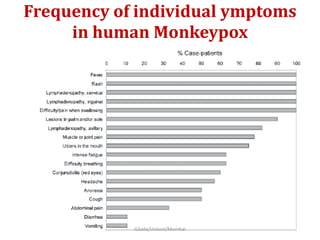
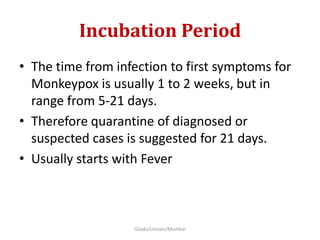
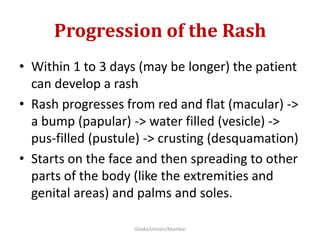
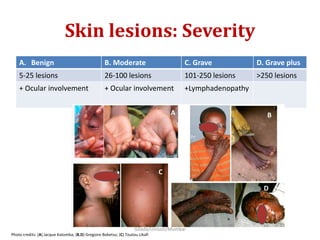
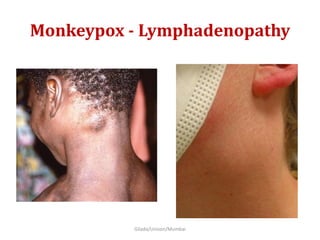
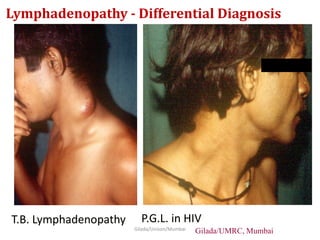
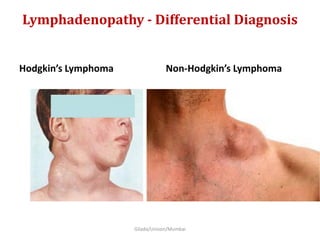
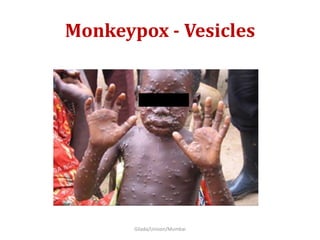
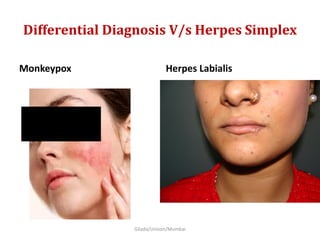
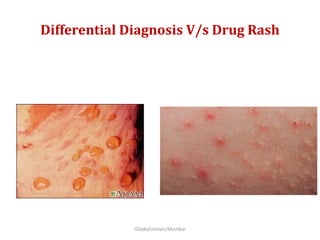
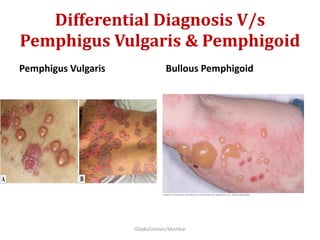
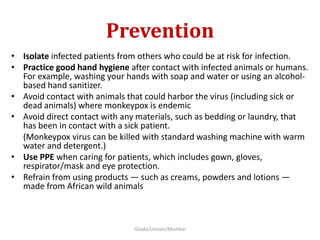
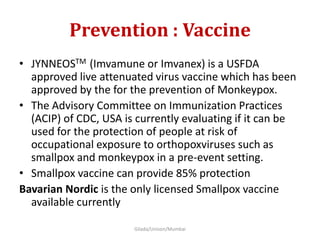
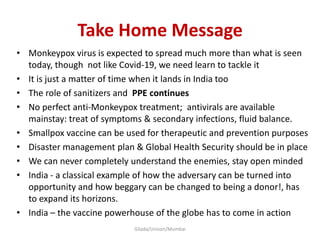
The document discusses the current monkeypox outbreak, detailing its origins, transmission, symptoms, and the global response, including containment efforts and vaccination developments. It emphasizes monkeypox as a zoonotic infection, primarily affecting individuals in certain risk categories, and outlines prevention strategies such as hygiene and PPE use. The report concludes with a call for improved disaster management and vaccine production capabilities, specifically highlighting India's potential role in addressing the outbreak.