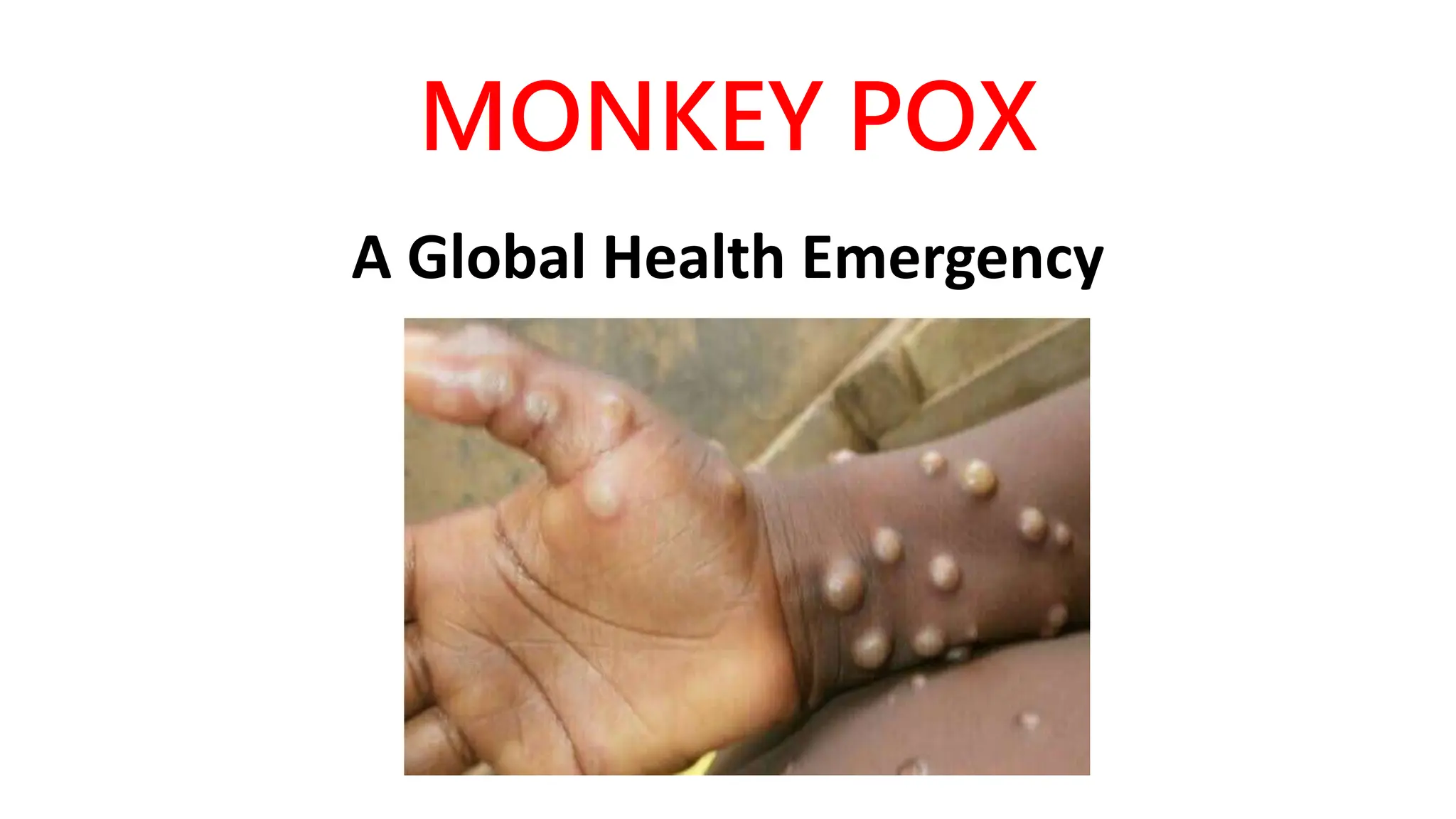
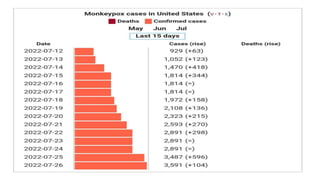
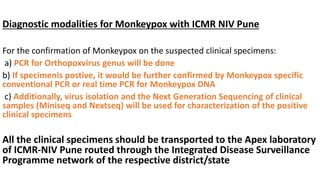
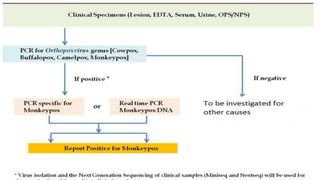
Monkeypox is a viral zoonosis that has emerged as a significant global health concern, particularly after the cessation of smallpox vaccination. The disease first identified in humans in 1970 has seen outbreaks in various countries, including a notable surge in the U.S. and India in 2022. The World Health Organization declared monkeypox a Public Health Emergency of International Concern on July 24, 2022, intensifying efforts for surveillance, treatment, and preventive measures against its spread.